- Search
|
|
Abstract
Purpose
Circular stapled hemorrhoidopexy (CSH) is widely used to treat patients with grades III–IV hemorrhoids because of less pain and short hospital stay. However, this procedure is associated with some complications, such as urge to defecate, anal stenosis, staple line dehiscence, abscess and sepsis. To avoid these complications, surgeons perform a partial stapled hemorrhoidopexy (PSH). The aim of this study is to present our early experience with the PSH.
Methods
We retrospectively reviewed the medical records of 58 patients with hemorrhoids who were treated with a PSH at Busan Hang-Un Hospital from January 2016 to June 2016. A specially designed tri-window anoscope was used, and a purse string suture was made at the mucosae of the protruding hemorrhoids through the window of the anoscope. The hemorrhoidopexy was done by using a circular stapler.
Results
Of the 58 patients included in this study, 34 were male and 24 were female patients (mean age, 50.4 years). The mean operation time was 12.4 minutes, and the mean postoperative hospital stay was 3.8 days. Three patients experienced bleeding (5.1%) 5 urinary retention (8.6%) and 5 skin tags (8.6%). Urge to defecate, tenesmus, abscess, rectovaginal fistula, anal stricture, incontinence, and recurrence did not occur.
A hemorrhoid is a common anomalous disease with a prevalence rate of 4% to 34% [1], and surgery is required in about 10% to 20% of patients with hemorrhoids who are complaining of symptoms [2]. In accordance with the Main Surgery Statistical Yearbook for 2014 released by the National Health Insurance Corporation of South Korea in 2015, hemorrhoid surgery was the second most common surgery after cataract surgery and accounted for 197,648 procedures [3]. In general, surgery is necessary in cases of grade-III hemorrhoids that are reduced by pushing the protruding hemorrhoids out of the anus by hand and in cases of grade-IV hemorrhoids that cannot be reduced manually. Many different methods of hemorrhoid surgery have been introduced and used, and the methods vary from a whole resection to a partial resection. In 1937, Milligan et al. [4] introduced a surgical procedure for partial resection of hemorrhoidal tissues, sparing mucocutaneous bridges, and that procedure was widely used as standard surgery because postoperative anal stenosis was uncommon [5]. However, postoperative anal pain and a long treatment period still remained as challenges to overcome. Longo [6] introduced a hemorrhoid surgical procedure using a circular stapler suturing device to overcome those shortcomings. That procedure was called by various names, for example, procedure for prolapse and hemorrhoid (PPH); the name of the procedure was determined at a consensus conference for hemorrhoid surgery held in France as stapled hemorrhoidopexy (SH) [7].
Currently, SH is being widely used as a surgical method for the treatment of patients with hemorrhoids and has been extensively studied for its safety, efficacy, and therapeutic results. In a randomized controlled study comparing it to conventional hemorrhoidectomy, SH was reported to be associated with less postoperative pain and faster recovery than conventional hemorrhoidectomy [8,9,10,11,12]. The surgical procedures are not difficult for the surgeon to perform, and many surgeons have performed this procedure on patients with hemorrhoids. However, at the same time, side effects have also been continuously reported. In addition to common complications, such as postoperative hemorrhage, anal stenosis and skin tags, postoperative complications, including postoperative early urge to defecate, rectovaginal fistula, pelvic abscess, and abdominal pneumoperitoneum due to perforation of the rectum, have been reported to occur in patients undergoing a SH [13,14,15,16,17,18]. Lin et al. [19] assumed that these problems were due to the presence of too many staples in the sensitive lower rectum and the 360 degrees of the stapled line, and introduced a partial SH (PSH) by improving the circular SH (CSH). This procedure selectively pure-string sutures only the hemorrhoidal tissues protruding through a specially fabricated window of an anoscope, and the hemorrhoidectomy is conducted using an automatic stapler to preserve the normal mucosa between the resection sites. At our hospital, the PSH was performed on patients who needed surgery for hemorrhoids for a period of 6 months, after which the results of the surgery were reviewed retrospectively. The stability and the advantages of this procedure and the complications associated with it were investigated.
This study was conducted using retrospective chart reviews in a total of 58 patients out of 64 patients diagnosed with grade III or higher grade hemorrhoids who needed surgical treatment and underwent PSH at Busan Hang-Un Hospital from January 1, 2016, to June 30, 2016; 6 patients who had a history of surgery and who had a concurrent anal fistula, rectal fistula or anal stenosis were excluded. Patients underwent physical examinations and anoscopic examinations before surgery, and basic blood tests were performed to identify any blood coagulation dysfunction or other abnormalities. The age and the sex of the patient, the operation time, and the severity of the hemorrhoids were also recorded. The severity of the hemorrhoids was classified into 4 grades in accordance with the Goligher classification; a hemorrhoid with hemorrhage but no prolapse is grade I, a hemorrhoid for which the prolapse protrudes during defecation but is spontaneously restored is grade II, a hemorrhoid with a prolapse that occurs while bearing down but requires manual restoration is grade III, and a hemorrhoid with a prolapse that cannot be restore manually is grade IV [20]. The duration of surgery, severity of postoperative pain, and postoperative hospital stay were also investigated. Postoperative pain was recorded on the first day and the third day after surgery by using a visual analogue scale (VAS). The VAS was rated at 0 for the absence of pain and at 10 for the most severe pain that the patient had ever experienced. The presence of complications, such as hemorrhage, urge to defecate and urinary retention (for patients treated with nelaton catheterization for at least one time), during the hospital stay were investigated. After discharge, the incidences of complications, such as hemorrhage, fecal incontinence, abscess, rectovaginal fistula, anal stricture, and skin tags, were checked during 4 to 6 weeks of regular out-patient observation; after the sixth week, the patients were asked to visit the outpatient clinic if they experienced any abnormal symptoms such as pain, fecal incontinence, difficulty in defecation, or palpable mass around the anus. Follow-up observations to detect recurrence were done for 2 to 8 months.
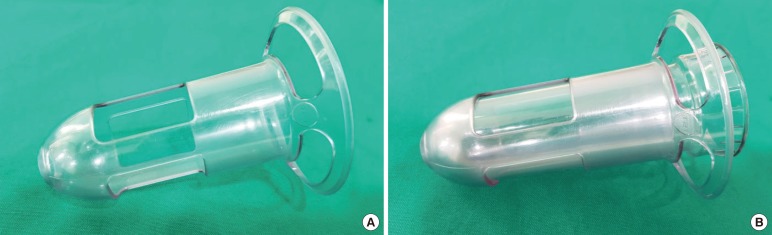
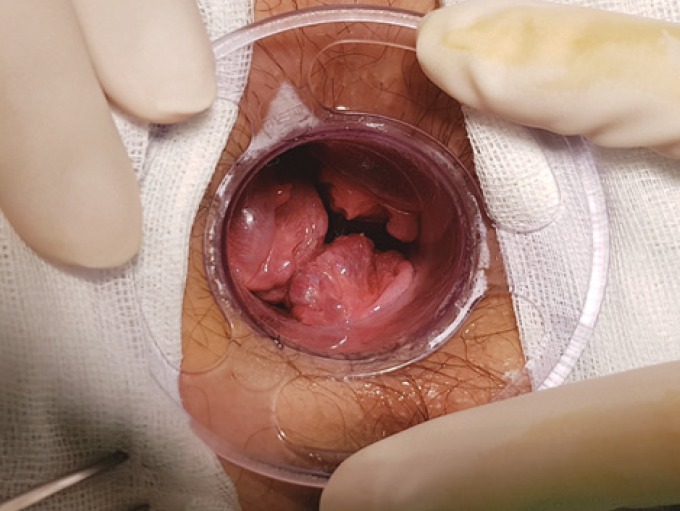
All 58 patients underwent surgery under spinal anesthesia in the Jack-knife prone position. Surgery was performed using the method introduced by Lin et al. [19]. An anoscope with a specially-designed window (Touchstone, Suzhou, China) attached was used (Fig. 1A), and a 33-mm PPHplus (Procedure for Prolapsed and Hemorrhoids, Touchstone, Suzhou, China) stapler was used as an automatic stapler. The anus was fully expanded using a lubricated circular anal dilator (CAD). The CAD was inserted into the tri-window anoscope, and the anoscope, as well as the CAD (Fig. 1B), were inserted into the anus and adjusted to pull the protruding hemorrhoids out through the window. After the location that allowed the protruding hemorrhoids to be pulled out well through the window of the anoscope had been determined, the anoscope was fixed to the anus (Fig. 2). A purse-string suture was performed on the mucosal and the submucosal layers of the 3 hemorrhoids protruding through window by using a 2/0 Polypropylene at 3 cm above the dentate line (Fig. 3). After the automatic stapler had been fully opened, the anvil was inserted into the anus to pass through the purse-string suture, and a knot was made by pulling the purse-string suture so that the mucosae of the three parts could enter the stapler while forming a fan-wing shape (Fig. 4). Then, the anvil was completely closed and the stapler was fired, after which the anvil was loosened and the stapler removed. Sometimes, a mucosal bridge was formed between the sites where the hemorrhoidal mucosae had been removed (Fig. 5) and in such cases, the bridge was removed by using an electric cauterizer (Fig. 6). Dog-ears were sometimes formed at both ends of the mucosal bridge. In such cases, they were sutured and ligated if necessary. The perianal area and the surgical site were carefully observed. If bleeding was present at the staple line, hemostasis was performed with an electric cauterizer, and if necessary, suturing and ligation were done. In cases of external hemorrhoids or skin tags that were intractable after the PSH, an additional excision was performed.
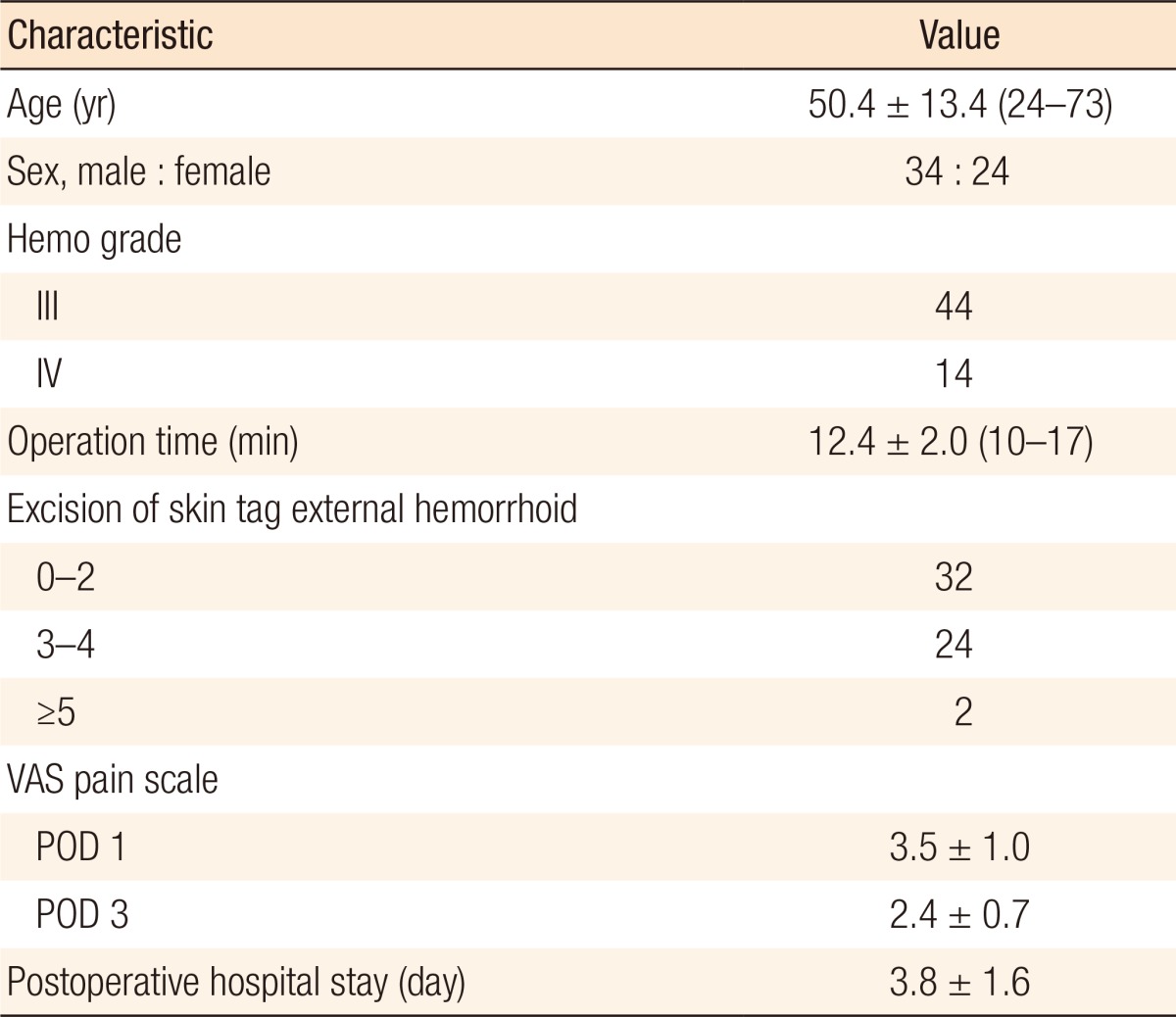
Of the 58 patients included in this study, 34 were male and 24 were female patients, and the mean age was 50.4 years. For the degree of hemorrhoids, 44 patients were grade III and 14 patients were grade IV. None of the 58 patients had a previous history of surgery for hemorrhoids, and none had any concurrent anal diseases other than hemorrhoids. No other procedures were performed together with the PSH and resections of external hemorrhoids and skin tags. No specific findings were found in the preoperative blood tests and coagulation profiles. The average operation time was 12.4 minutes. Thirty-two patients underwent additional resections for fewer than 2 external hemorrhoids or skin tags, and 24 patients underwent additional resections for 3 or 4 external hemorrhoids or skin tags. Two patients underwent additional resections for more than 5 external hemorrhoids or skin tags. The mean pain score measured using the VAS on day 1 after the surgery was 3.4 points whereas the mean pain score measured on day 3 after the surgery was 2.4 points. Those who were discharged before day 3 were excluded from the measurement. The mean postoperative hospital stay was 3.8 days (Table 1).
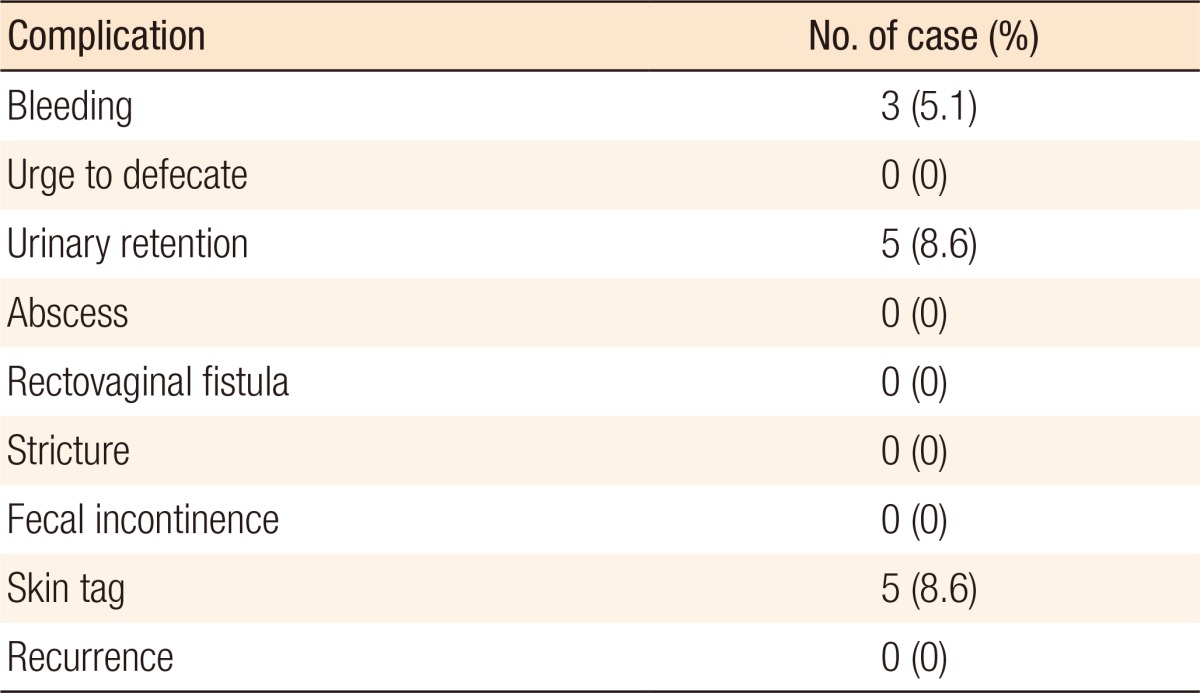
Postoperative bleeding occurred in three patients. One was an in-patient at the hospital on day 2 after the surgery who was found with bleeding from the staple line; hemostasis was done by using an electric cauterizer and ligation. Two were out-patients who were found on day 7 and on day 8 after the surgery with bleeding from the ‘dog-ear’ site; hemostasis was done by suturing and ligation. Those three were patients who had undergone the surgery at a relatively early stage as they were the 6th and the 10th patients on whom PSH had been performed and in whom the ‘dog-ear’ sites had not undergone suture ligation. All 3 patients recovered well without further complications such as hemorrhage. Urinary retention was determined based on the patients who had undergone urinary catheterization at least once and was found in a total of 5 cases. The urinary retentions had occurred mainly on the night of the surgery day and on day 1 after surgery and improved spontaneously without special treatment. No patient complained of an urge to defecate. Skin tags were confirmed in 5 cases, and four of those underwent simple resections 2 to 3 months later; one patient did not consent to the having resection. No postoperative complications, such as rectovaginal fistula, abscess, fecal incontinence and anal stenosis, were noted, and no recurrences were detected during the follow-up period (Table 2).
Although the etiology of hemorrhoids is not yet known, they are thought to be caused by a pathological change in the anal cushion. One of the main causes is thought to be a breaking of Parks' ligament, which supports the anal cushion, due to the degeneration of the anal canal epithelium, after which the anal cushion prolapses out of the anus to cause various symptoms [21]. CSH involves the resection of an abnormally enlarged mucosa of the lower rectum, followed by a mucosa-to-mucosa anastomosis and a repositioning back to their normal anatomical positions of the hemorrhoid cushions that had moved downward. The submucosal blood vessels are then blocked to reduce submucosal venous congestion [21,22]. The principle of the PSH is not much different from that of the CSH. However, in the PSH, the mucosa is not excised at 360 degrees; only the protruding hemorrhoids are selectively removed while preserving the normal mucosa between the resected mucosae. Therefore, the PSH is characterized by a reduction in the number of staples stuck to the rectal mucosa compared to the CSH, and it is less invasive [19].
Lin et al. [19], who first introduced the PSH, performed it on 44 patients and had a follow-up period of about 1 year. During the first year, 1 case of recurrence and 1 case of bleeding were found while no symptoms, such as anal stenosis and fecal incontinence, were found. Lin et al. [23] also conducted a prospective, controlled study comparing the CSH and the PSH, for which the follow-up period was 2 years. The PSH was performed on 34 patients, and the CSH was performed on 38 patients. Postoperative bleeding was found in 2 cases (5.8%) in the CSH group and 2 cases (5.2%) in the PSH group whereas fecal incontinence was identified as gas feces in three cases in the CSH group only. Recurrence during the 2-year follow-up was confirmed in 1 case (2.9%) in the PSH group and 2 cases (5.3%) in the CSH group. Wang et al. [24] performed surgery in the same way as the PSH and newly named it as tissue selecting therapy (TST). They presented a study comparing the Milligan-Morgan hemorrhoidectomy (MMH) with the TST. Each procedure was conducted on 240 subjects, and the subjects were followed for 1 year after surgery. In the TST group, the mean VAS score at 12 hours postoperatively was 5.08 ± 1.62, and in the MMH group, it was 7.19 ± 2.01, which was significantly lower in the TST group (P < 0.05). Postoperative urinary retention was present in 22 cases in the TST group and 47 cases in the MMH group. The TST group had a significant lower incidence of urinary retention (P < 0.05). The operation time was also significantly shorter in the TST group, and the number of hospital days was significantly lower in the TST group. No rectovaginal fistula was found in either group, and fecal incontinence was confirmed in 3 cases with a hemorrhoidectomy in the TST group and in 16 cases with a hemorrhoidectomy in the PSH group, being significantly lower in the PSH group (P < 0.05). In the study of Lin et al. [25], the surgery was performed in the same way as the PSH and was named as tissue selecting technique (TST). They conducted a retrospective patient controlled study comparing the MMH with the TST. One hundred twenty-one patients and 74 patients were included in the TST group and in the MMH group, respectively, and they were followed for 1 year. On the pain comparison using the VAS at 12 hours after surgery, as well as on day 3 and day 7 after surgery, the TST group showed significantly lesser pain than the MMH group (P = 0.01). In the TST group, no rectovaginal fistula or anal stenosis was observed. Recurrence was observed in 4 cases (3.3%) in the TST group and 2 cases (2.7%) in the MMH group, but the difference between the 2 groups was not statistically significant (P = 0.170).
In addition to the results of this study, other studies [19,23,24,25] have shown that surgical removal of the protruding hemorrhoids selectively by using an automatic stapler was an effective and safe procedure for treating patients with hemorrhoids. In this study, no recurrence of the hemorrhoids was noted, although the follow-up period was rather short. No complications that could be problematic, compared with other surgical treatments, were observed. Other studies have also shown low recurrence rates and tolerable complications [19,23,24,25]. The pain scores on day 1 and day 3 after the surgery, as measured with the VAS, were 3.5 ± 1.0 and 2.4 ± 0.7, respectively, in this study, indicating relatively less pain. Other studies have reported similar results. In a study that compared the CSH with a conventional hemorrhoidectomy [10,11], the results indicated that less pain and a shorter hospital stay were observed in the CSH group of patients. Likewise, in a study that compared the PSH with a conventional hemorrhoidectomy, the PSH had more advantages than the conventional hemorrhoidectomy [24,25]. When compared with a conventional hemorrhoidectomy, the PSH had characteristics similar to those of the CSH.
The precise mechanism of pain occurring after a SH is not yet known. However, a suggestion had been made that the pain might be associated with minor inflammation occurring in the stapled ring [26]. In the case of the PSH, the staple count is lower than it is in the case of the CSH; thus, the PSH might be predicted to have a reduced incidence of staple-induced inflammation, thus resulting in less pain. In a prospective controlled study performed by Lin et al. [23] that compared the PSH with the CSH, the postoperative pain was measured using the VAS, and the pain at the first defecation after the surgery was significantly less in the PSH group. In the study, they assumed that the stapled ring formed in the CSH was pulled when the rectum was inflated and that at the time of the first defecation after the surgery, the staples were immobile with degraded elasticity, so more pressure was exerted during defecation, which would further stimulate the sensitive epithelium, causing the pain to be more severe. On the other hand, they explained that the normal mucosa existing between resection sites of the rectal mucosa would be well stretched with elasticity, suggesting that the pain would be less in the case of the PSH. The urge to defecate occurring after a SH has also been reported to range from 3% to 40% [26,27], but its exact mechanism is not yet fully understood. In some studies, the stapled ring is thought to affect the urge to defecate [26], and the study of Lin et al. [23] also showed that the frequency of complaining about the urge to defecate was statistically significantly lower in the PSH group than in the CSH group. Lin et al. [23] also thought that a decrease in the number of staples may have been the reason for this result. In our study, no patients complained of an urge to defecate after surgery.
In addition to the reduction of staple line inflammation caused by a decrease in the number of staples used in the PSH, which is thought to be an advantage of the PSH with respect to the pain and the urge to defecate, in the PSH, the protruding mucosa is selectively resected while preserving the normal rectal mucosa between the resection margins, so it can be said to be anatomically less invasive. After the CSH, some incidences of abdominal pneumoperitoneum caused by perforation of the rectum and pelvic abscess may occur, possibly leading to sepsis and being life-threatening [13,16,17,18]. The incidence of such complications is thought to be lower in the PSH because the PSH has fewer resection sites on the rectal mucosa. In addition, the possibility of complications, such as rectovaginal fistulas, anal stenosis and fecal incontinence, is also thought to be lower in the PSH. A large-scale, randomized, controlled trial is needed to confirm the benefits and the utility of the PSH.
In conclusion, in this study, the PSH was found to be an effective and safe surgical method for treating patients with grades III and IV protruding hemorrhoids. It is a less invasive procedure compared to the CSH and is safer than the CSH in patients with high risk of pelvic abscess, rectovaginal fistula, and anal stenosis.
References
1. Loder PB, Kamm MA, Nicholls RJ, Phillips RK. Haemorrhoids: pathology, pathophysiology and aetiology. Br J Surg 1994;81:946–954. PMID: 7922085.


2. Bleday R, Pena JP, Rothenberger DA, Goldberg SM, Buls JG. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum 1992;35:477–481. PMID: 1568400.


3. 2014 major surgery statistics [Internet]. Wonju: National Health Insurance Service; c2014.cited 2015 Dec 28. Available from: http://www.nhis.or.kr/bbs7/boards/B0079/16017
4. Milligan E, Morgan CN, Jones L, Officer R. Surgical anatomy of the anal canal, and the operative treatment of haemorrhoids. Lancet 1937;230:1119–1124.

5. Khubchandani IT. Operative hemorrhoidectomy. Surg Clin North Am 1988;68:1411–1416. PMID: 3194822.


6. Longo A. Treatment of hemorrhoids disease by reduction of mucosa and hemorrhoidal prolapse with a circular stapler suturing device: a new procedure In: Proceedings of the 6th World Congress of Endoscopic Surgery; 1998 Jun 3-6; Rome, Italy. Bologna, Monduzzi Editore; 1998. p. 777–784.

7. Corman ML, Gravié JF, Hager T, Loudon MA, Mascagni D, Nyström PO, et al. Stapled haemorrhoidopexy: a consensus position paper by an international working party - indications, contra-indications and technique. Colorectal Dis 2003;5:304–310. PMID: 12814406.


8. Laughlan K, Jayne DG, Jackson D, Rupprecht F, Ribaric G. Stapled haemorrhoidopexy compared to Milligan-Morgan and Ferguson haemorrhoidectomy: a systematic review. Int J Colorectal Dis 2009;24:335–344. PMID: 19037647.


9. Shao WJ, Li GC, Zhang ZH, Yang BL, Sun GD, Chen YQ. Systematic review and meta-analysis of randomized controlled trials comparing stapled haemorrhoidopexy with conventional haemorrhoidectomy. Br J Surg 2008;95:147–160. PMID: 18176936.


10. Kairaluoma M, Nuorva K, Kellokumpu I. Day-case stapled (circular) vs. diathermy hemorrhoidectomy: a randomized, controlled trial evaluating surgical and functional outcome. Dis Colon Rectum 2003;46:93–99. PMID: 12544528.


11. Pavlidis T, Papaziogas B, Souparis A, Patsas A, Koutelidakis I, Papaziogas T. Modern stapled Longo procedure vs. conventional Milligan-Morgan hemorrhoidectomy: a randomized controlled trial. Int J Colorectal Dis 2002;17:50–53. PMID: 12018455.


12. Yun KJ, Cho HC. Clinical experience with a circular stapled hemorrhoidopexy without circular anal dilator (CAD). J Korean Soc Coloproctol 2007;23:431–436.

13. Park YJ. Pneumoretroperitoneum after procedure for prolapsed hemorrhoid. Ann Coloproctol 2013;29:256–258. PMID: 24466542.



14. Brisinda G, Vanella S, Cadeddu F, Marniga G, Mazzeo P, Brandara F, et al. Surgical treatment of anal stenosis. World J Gastroenterol 2009;15:1921–1928. PMID: 19399922.



15. Lee KY. Complications after stapled hemorrhoidopexy. J Korean Surg Soc 2005;68:327–331.
16. Wong LY, Jiang JK, Chang SC, Lin JK. Rectal perforation: a life-threatening complication of stapled hemorrhoidectomy: report of a case. Dis Colon Rectum 2003;46:116–117. PMID: 12544531.


17. Ripetti V, Caricato M, Arullani A. Rectal perforation, retropneumoperitoneum, and pneumomediastinum after stapling procedure for prolapsed hemorrhoids: report of a case and subsequent considerations. Dis Colon Rectum 2002;45:268–270. PMID: 11852343.


18. Molloy RG, Kingsmore D. Life threatening pelvic sepsis after stapled haemorrhoidectomy. Lancet 2000;355:810PMID: 10711934.


19. Lin HC, He QL, Ren DL, Peng H, Xie SK, Su D, et al. Partial stapled hemorrhoidopexy: a minimally invasive technique for hemorrhoids. Surg Today 2012;42:868–875. PMID: 22160324.


20. Goligher JC. Surgery of the anus rectum and colon. 4th ed. London: Bailliere Tindall; 1980.
22. Beattie GC, Lam J, Loudon MA. A prospective evaluation of the introduction of circumferential stapled anoplasty in the management of haemorrhoids and mucosal prolapse. Colorectal Dis 2000;2:137–142. PMID: 23578037.


23. Lin HC, Ren DL, He QL, Peng H, Xie SK, Su D, et al. Partial stapled hemorrhoidopexy versus circular stapled hemorrhoidopexy for grade III-IV prolapsing hemorrhoids: a two-year prospective controlled study. Tech Coloproctol 2012;16:337–343. PMID: 22402919.


24. Wang ZG, Zhang Y, Zeng XD, Zhang TH, Zhu QD, Liu DL, et al. Clinical observations on the treatment of prolapsing hemorrhoids with tissue selecting therapy. World J Gastroenterol 2015;21:2490–2496. PMID: 25741159.



25. Lin HC, Luo HX, Zbar AP, Xie SK, Lian L, Ren DL, et al. The tissue selecting technique (TST) versus the Milligan-Morgan hemorrhoidectomy for prolapsing hemorrhoids: a retrospective case-control study. Tech Coloproctol 2014;18:739–744. PMID: 24952734.


26. Fueglistaler P, Guenin MO, Montali I, Kern B, Peterli R, von Flüe M, et al. Long-term results after stapled hemorrhoidopexy: high patient satisfaction despite frequent postoperative symptoms. Dis Colon Rectum 2007;50:204–212. PMID: 17180255.


27. Mlakar B, Kosorok P. Complications and results after stapled haemorrhoidopexy as a day surgical procedure. Tech Coloproctol 2003;7:164–167. PMID: 14628160.


- TOOLS