INTRODUCTION
Rectal prolapse is a benign condition in which the rectum protrudes outside the anus; this occurs mainly in elderly women [1]. Although rarely fatal, it can lead to distressing symptoms that have a significant impact on the patientãs quality of life [2]. Surgery is the only curative treatment. However, despite multiple randomized prospective trials, there is still no consensus on the standard procedure for rectal prolapse repair [3-6].
Surgery for rectal prolapse has been broadly categorized into 2 procedures; the abdominal and the perineal approach. Each approach has its own advantages and drawbacks. The perineal approach is considered suitable for frail and elderly patients because it can be performed under local or spinal anesthesia, with lower morbidity [7]. It is also recommended for young male patients because pelvic nerve injury can be avoided, which preserves sexual or urinary function [8]. Notwithstanding the advantages, a higher recurrence rate with the perineal approach has been reported as compared to the abdominal approach [2, 7].
Delormeãs procedure is one of the best-known perineal operations for full-thickness rectal prolapse; it involves sleeve resection of the mucosa and plication of the rectal wall muscle. Generally, surgeons prefer this procedure for short rectal prolapse [9, 10]. However, few studies have examined the association between the length of the prolapsed rectum and recurrence after Delormeãs procedure. Therefore, we aimed to examine whether the length of the prolapsed rectum was associated with recurrence after the Delormeãs procedure in order to predict patients with a higher risk of recurrence before Delormeãs procedure.
METHODS
Study population and design
We performed a retrospective review of all consecutive patients who underwent surgery for full-thickness rectal prolapse at the Tokyo Yamate Medical Center from January 2014 to December 2019. The study population comprised all patients on whom Delormeãs procedure was performed. Patients with short-segment of full-thickness rectal prolapse underwent Delormeãs procedure in accordance with clinical practice guidelines [11, 12]. Patients with a history of treatment failure after a previous operation for rectal prolapse were also included. Finally, patients whose medical records were incomplete were excluded from the analysis.
This retrospective study was approved by the Institutional Review Board of the Tokyo Yamate Medical Center (No. J-075), and the requirement to obtain informed consent was waived.
Data collection
The data that were retrospectively obtained through the review of a prospectively generated database were as follows: age, sex, body mass index, previous history of anal surgery, previous history of surgery for rectal prolapse, and length of the prolapsed rectum. Length of the prolapsed rectum was defined as the length between the apex of the prolapse and the level of the perineum while straining in the squatting position. Follow-up data was documented prospectively until recurrence occurred, or until the cutoff date of the study, i.e., March 2020. Recurrence was defined as anatomical recurrence of external full-thickness prolapse of the rectal wall and diagnosed clinically at outpatient clinic.
Perioperative management
All patients had the length of prolapsed rectum measured while straining. Preoperative defecography was performed on patients for whom an accurate length of the prolapsed rectum could not be measured. Patients who were suspected as having intraluminal malignancy because of their symptoms such as anemia, bloody stool, or history of body weight loss, underwent preoperative colonoscopy to exclude intraluminal pathology. Similarly, patients who were suspected as having poor sphincter function by digital exam underwent preoperative anal manometry to evaluate rectal physiology. Delormeãs procedure was indicated for patients who had a prolapsed rectum sized < 5 cm without pelvic organ prolapse or for patients who could not tolerate general anesthesia. Preoperatively, all patients received bowel preparation, and intravenous antibiotics were administered prophylactically. All patients had the surgery under hyperbaric spinal anesthesia. During the surgery, a mucosectomy was performed until greater than twice the length of the prolapsed rectum was obtained. The patients were followed up 3 weeks after surgery and every 3 months thereafter.
Statistical analysis
The outcome was to determine the clinicopathological risk factors for recurrence of full-thickness rectal prolapse after Delormeãs procedure. Recurrence-free time (RFT) was defined as the period between the date of rectal prolapse surgery and the date of recurrence. Kaplan-Meier analysis was used to estimate RFT, and survival curves were compared using the log-rank test. Multivariable Cox proportional hazards regression models were subsequently fitted to evaluate factors independently associated with RFT. Patient age, sex, length of the prolapsed rectum, and variables found to have a P-value of < 0.20 in univariate analysis were included in the multivariate analysis models [8, 13, 14]. Results are presented as hazard ratios (HRs) and 95% confidence intervals (CIs). All statistical analyses were performed using the JMP15 software program (SAS Institute Japan Ltd., Tokyo, Japan).
RESULTS
The details of our study cohort are summarized in Fig. 1. During the study period, a total of 104 patients underwent Delormeãs procedure for rectal prolapse, with a median follow-up time of 6.4 months (interquartile range [IQR], 3.2ã13.4 months). Eight patients were excluded due to missing data on prolapsed rectum length. Accordingly, the final study population consisted of 96 patients.
Baseline characteristics of patients in this study are shown in Table 1. A total of 82 female patients (85.4%) and 14 male (14.6%), with a median age of 78.5 years (IQR, 72ã84.5 years) were enrolled. Among the 96 patients, 24 patients had undergone previous surgery for rectal prolapse; laparoscopic rectopexy (n=8), Gant-Miwa-Thiersch procedure (n=3), and Delormeãs procedure (n=13). Sixteen patients had undergone previous anal surgery; 12 cases had surgery for hemorrhoids, 3 cases for anal fistula, and 1 case for rectal cancer (intersphincteric resection). The median prolapsed rectal length was 3.0 cm (range, 1.0ã6.6 cm).
No mortality occurred during the follow-up period. One patient developed anal stricture after surgery and required bougie dilation. No other complication including sexual or urinary dysfunction was reported.
Recurrence after Delormeãs procedure
Among the 96 patients, full-thickness rectal prolapse recurrences occurred in 26 patients (27.1%) at a median of 7.5 months (range, 1ã62 months). After recurrence, 4 patients underwent a revised Delormeãs procedure, 9 received a laparoscopic rectopexy, 9 received Thiersch procedure, and 4 refused further surgery.
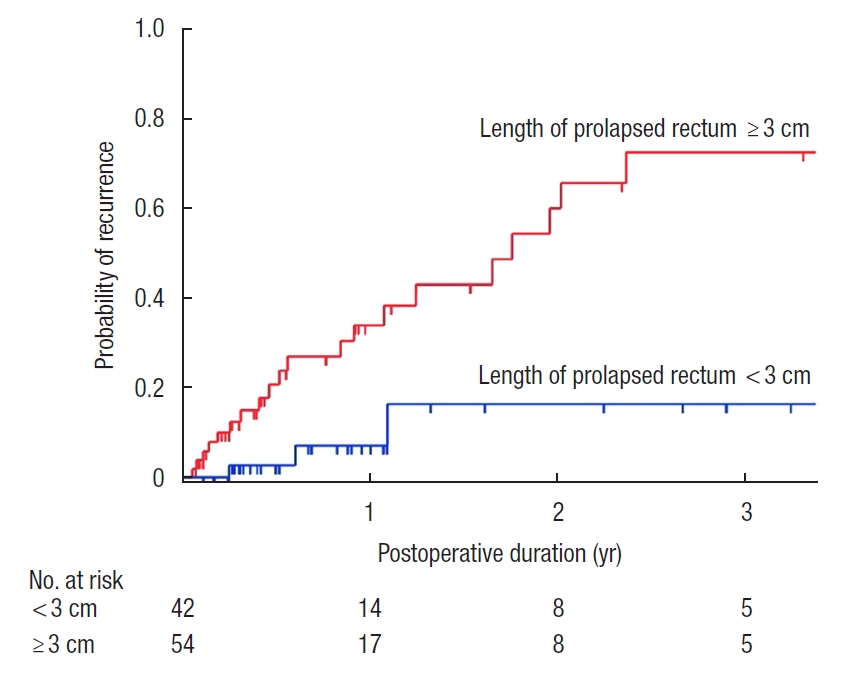
In univariate analysis, prolapsed rectum length of ãË 3 cm was significantly associated with prolapse recurrence (42% vs. 7%, P<0.001; Fig. 2). Patients with shorter length of prolapsed rectum experienced recurrence within 14 months of surgery. In contrast, there was no definitive pattern for recurrence in patients with longer prolapses. No other significant predictors for recurrence were revealed.
In multivariate analysis, prolapsed rectum length of ãË 3 cm was found to be independently associated with prolapse recurrence after Delormeãs procedure (HR, 6.28; 95% CI, 1.83ã21.5; P<0.001) (Table 2). Advanced age and being female were not significantly associated with recurrence in this study.
DISCUSSION
The aim of the present study was to investigate the association between the length of prolapsed rectum and recurrence of rectal prolapse. We demonstrated that patients with a prolapse length of ãË 3 cm had a significantly higher risk of recurrence after Delormeãs procedure. In previous studies, although the difference was not significant, patients with long rectal prolapses had a higher rate of relapse than patients with smaller prolapses [8, 15]. To our knowledge, this is the first study to demonstrate the relationship between the length of rectal prolapse and recurrence rate after Delormeãs procedure. While treating patients with long rectal prolapses, it can be better to have alternative options for surgery such as rectopexy or Altemeier surgery.
In contrast to previous studies, our study did not reveal a significant association between advanced age and increased risk of recurrence [8]. Elderly patients generally have a weak pelvic floor that contributes to recurrence after Delormeãs procedure [16, 17]. In our study, more than 80% of patients were over 65 years of age. The relatively low number of young people in this current study did not significantly increase the risk of prolapse recurrence.
Another important finding of this study was the low morbidity and complication rate after Delormeãs procedure. Despite 25% of patients have had previous surgery for rectal prolapse, there were no reported cases of mortality, sexual or urinary dysfunction. With the development of laparoscopic surgery, although the abdominal approach now allows performing procedures with greater safety, it is yet to be determined whether the abdominal approach is the safest approach for patients with previous rectal prolapse surgery. Our study demonstrated that the perineal approach can be safely performed even in patients with previous surgery.
Previous studies reported that the rate of recurrence after Delormeãs procedure ranged from 9.6% to 29.7% [6, 8, 13-15, 18-21]. The rate of recurrence in this current study was 27.1%, which is relatively higher than previous reports. Two factors may account for the high rate of recurrence in our study. Firstly, our cohort includes a large number of elderly patients compared with the demographics of previous studies. Elderly patients with rectal prolapse have poor sphincter function, which contributes to a higher risk of recurrence. Secondly, 24 of the 96 patients (25.0%) had undergone previous surgery for rectal prolapse. Failure of previous rectal prolapse surgery may indicate a more severe prolapse, which has a higher risk of recurrence.
Our study has several limitations. First, because the study was retrospective in design, selection bias may exist. Second, although the sample size in this study is the largest to be reported in a study on risk factors after Delormeãs procedures, the sample size was still relatively small. Third, not all patients underwent the same initial metrics evaluation; some underwent defecography, others received anal manometry, and others underwent a colonoscopy. Such evaluations may reveal factors, such as sphincter dysfunction, which are associated with prolapse recurrence after surgery. Finally, a relatively short median follow-up of 6.5 months may underestimate the rate of recurrence after Delormeãs procedure.
In conclusion, we found an association between recurrence after Delormeãs procedure and rectal prolapse length. Therefore, the prolapsed rectum should be measured prior to performing Delormeãs procedure. A prospective study is required to better determine other predictors of prolapse recurrence after Delormeãs procedure.