- Search
Abstract
Purpose
Minimizing the polyp miss rate during colonoscopy is important for patients at high risk for colorectal polyps. We investigated the polyp miss rate and the factors associated with it in high-risk patients.
Methods
The medical records of 163 patients who underwent follow-up colonoscopy between January 2001 and April 2010, which was within 9 months after a polypectomy, because the index colonoscopy had shown multiple (more than 3) adenomas or advanced adenoma were retrospectively reviewed. Miss rates were calculated for all polyps, for neoplastic polyps and for advanced adenomas. Factors associated with the miss rates in these patients, such as the location, shape and size of the polyp, were analyzed.
Results
The miss rates for polyps, adenomas, adenomas <5 mm, adenomas Ōēź5 mm and advanced adenomas were 32.6%, 20.9%, 17.7%, 3.2%, and 0.9%, respectively. No carcinoma, except for one small carcinoid tumor, was missed. Flat shape and small size (<5 mm) were significantly associated with adenoma miss rate. The miss rate was significantly higher for flat-type advanced adenomas than for protruded-type advanced adenomas (27.7% vs 4.1%).
Colonoscopy is the best method of detecting and removing colonic polyps [1]. Removing adenomatous polyps before they progress to adenocarcinomas can significantly reduce the incidence of colorectal cancer. Despite the advantages of colonoscopy, its accuracy is unclear [1-4]. The colorectal cancer diagnosis rate 3 or 5 years after a "clearing colonoscopy" has been reported to range from 0.5% to 5% [5]. These tumors may arise from lesions missed on colonoscopy, suggesting the need for shorter intervals between colonoscopic examinations, a suggestion that can markedly increase healthcare costs.
A missed polyp is defined as a polyp missed at initial colonoscopy, but found on a repeat colonoscopy. The polyp miss rate is defined as the proportion of polyps detected only during the second colonoscopy relative to the total number of polyps found during the first and the second examinations. Tandem colonoscopy has shown that the polyp miss rate can range from 15% to 24% [1, 6]. Moreover, the shape, location and size of the polyps have been associated with the miss rate [2, 3, 7].
Current guidelines from the American College of Gastroenterology classify patients with an advanced adenoma-villous or high-grade dysplasia or more than 1 cm in diameter-or with more than 3 adenomas as being at high risk for recurrent adenomas [8]. The relative risk for developing colon cancer was 2.7-fold greater in patients with large polyps, Ōēź1 cm in size, and 5-fold greater in patients with multiple polyps than in patients without polyps [9]. Reducing the polyp miss rate in high-risk patients can, therefore, effectively reduce the incidence of metachronous colorectal cancer after a polypectomy. We, therefore, assessed polyp miss rates and the factors associated with missed polyps in patients at high risk for colorectal polyps.
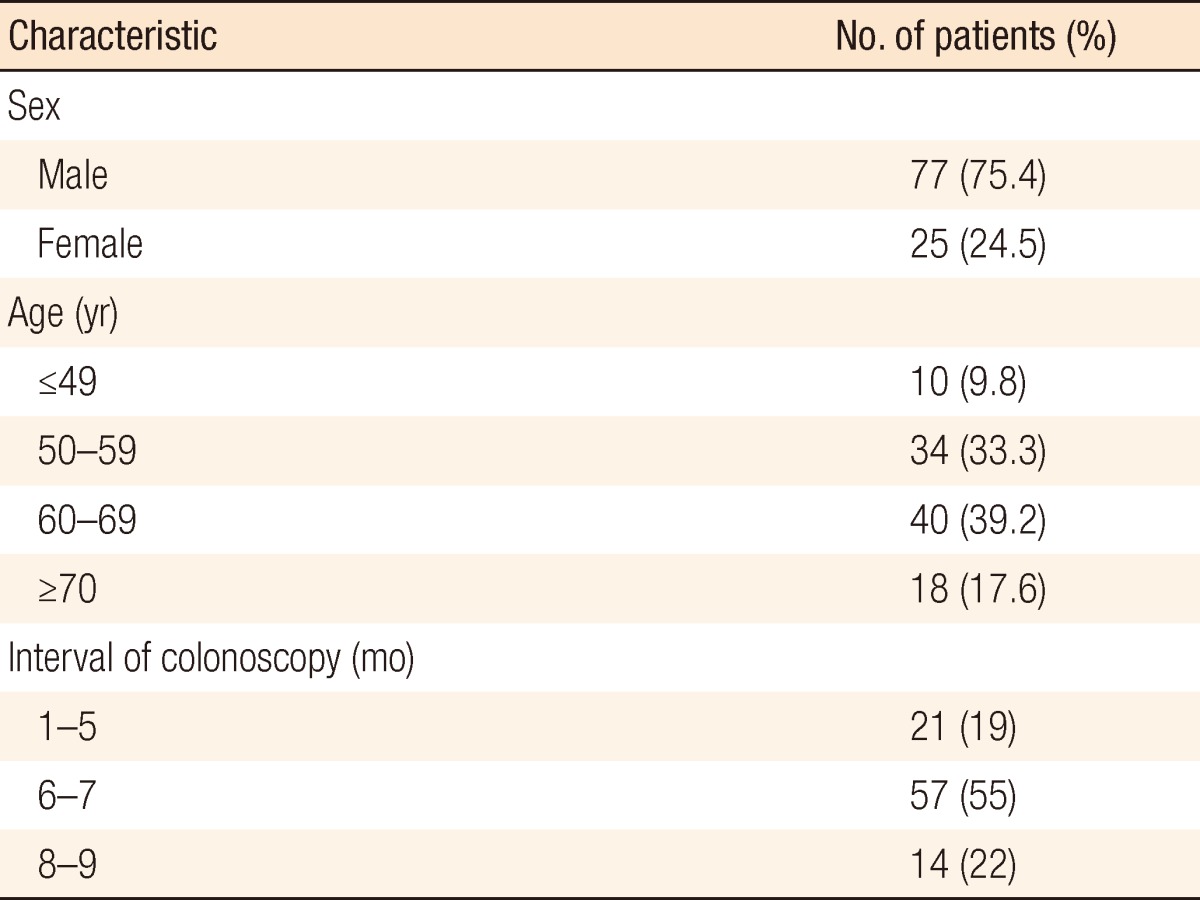
According to the recommendation of the American College of Gastroenterology, we classified patients with an advanced adenoma or with more than three adenomas as being at high risk for recurrent adenomas. The medical records of 163 patients who underwent follow-up colonoscopy between January 2001 and April 2010, within 9 months after a polypectomy, because the index colonoscopy had shown multiple (more than 3) polyps or an advanced adenoma were retrospectively reviewed. Patients were excluded if they had advanced colorectal cancer at the index colonoscopy, had undergone a bowel resection during follow-up colonoscopy (n = 3), had familial polyposis (n = 1), had undergone an initial polypectomy at another hospital (n = 33), could not undergo a polypectomy because they were taking anticoagulant medication (n = 5), or had undergone a colonoscopy due to gastrointestinal bleeding (n = 3). In addition, patients with incomplete description (n = 11) or poor bowel preparation (n = 5) were excluded. Finally, 102 patients were enrolled in this study. Patient demographics are shown in Table 1. This study was approved by the Institutional Review Board of the National Cancer Center, Korea (NCCNCS-10-360).
Bowel preparation was performed with polyethylene glycol or sodium phosphate solution and was assessed by the examiner as excellent (no residual liquid or stool), good (a small amount of liquid, with clear visualization of the entire colonic mucosa), poor (a small amount of residual stool that could be easily moved after cleansing so that most of the colonic mucosa could be clearly visualized), or bad (nonaspirable or residual stools after cleansing of the mucosa so that most of the colonic mucosa could not be clearly visualized). If bowel preparation was poor or bad, patients were excluded from the analysis. All observed polyps were removed during colonoscopic examination. If a polypectomy could not be performed due to several causes such as anticoagulant medication, we excluded these cases as described above.
We reviewed the charts and recorded the number, size, location, and morphology of the polyps at colonoscopy, as well the presence of villous architecture and degree of dysplasia on pathology. A high-risk patient was defined as a patient with an advanced adenoma or more than three adenomas at the initial colonoscopy. An advanced adenoma was defined as an adenoma with a diameter Ōēź10 mm or a villous component or severe dysplasia. The location of the polyp was divided into the proximal colon (cecum, ascending colon, hepatic flexure, transverse colon, and splenic flexure) and the distal colon (descending colon, sigmoid colon, and rectum). The size of each lesion was estimated to the nearest millimeter by visually comparing it with the known diameter of opened biopsy forceps. The polyp's shape was determined according to the Paris classification [10].
The polyp miss rate was defined as the proportion of polyps detected only during the second colonoscopy, which was performed within 9 months after the initial clearing colonoscopy, relative to the total number of polyps found during the first and the second examinations. Miss rates were calculated for "all polyps," both nonneoplastic and neoplastic; for neoplastic polyps, both adenomas and colorectal carcinomas; and for advanced adenomas (Ōēź1 cm in size or with high-grade dysplasia or an in situ carcinoma). The pooled miss rate for each specific lesion was calculated as the total number of lesions missed by the first procedure divided by the total number of polyps found during the first and the second examinations. The miss rate for specific lesions was calculated as the total number of these lesions missed by the first procedure divided by the total number of these specific lesions found during the first and the second examinations. The overall per-patient miss rate was calculated as the number of patients with lesions missed during the first colonoscopy divided by the total number of patients, and the per-patient miss rate for each specific lesion type was calculated as the number of patients with a lesion of that type missed during the first colonoscopy divided by the number of patients with at least one lesion of that type found at both the first and the second colonoscopies.
Statistical analyses were performed using SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). Fisher exact tests were used to compare baseline characteristics, numbers of missed polyps, and the miss rate according to the location, shape and size of the polyps. A P-value less than 0.05 was considered statistically significant.
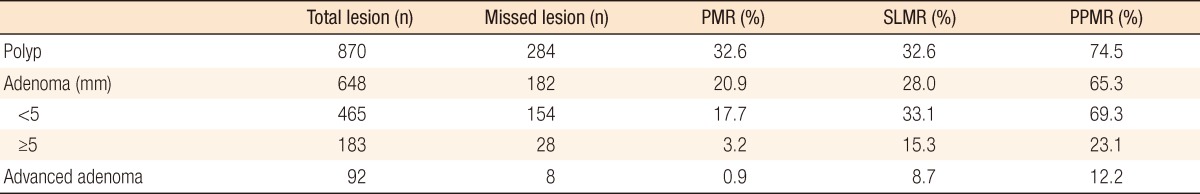
Overall, the 102 patients had 870 polyps during both colonoscopic examinations. The mean polyp size was 4.5 mm (range, 1-50 mm). When we assessed polyp type, we found 648 adenomas in 98 patients; 1 carcinoid tumor in 1 patient; and 92 advanced adenomas, including 8 Tis lesions, in 57 patients (Table 2). The average number of polyps per patient was 8.5, and the average number of adenomas was 5.5.
Pooled miss rates for polyps, adenomas and advanced adenomas were 32.6%, 20.9%, and 0.9%, respectively. The specific lesion miss rates for polyps, adenomas, and advanced adenomas were 32.6%, 28.0%, and 8.7%, respectively. Per-patient miss rates for polyps, adenomas and advanced adenomas were 74.5%, 65.3%, and 12.2%, respectively (Table 2). Of the eight Tis lesions, none was missed. A carcinoid tumor was detected at the second colonoscopy in one patient.
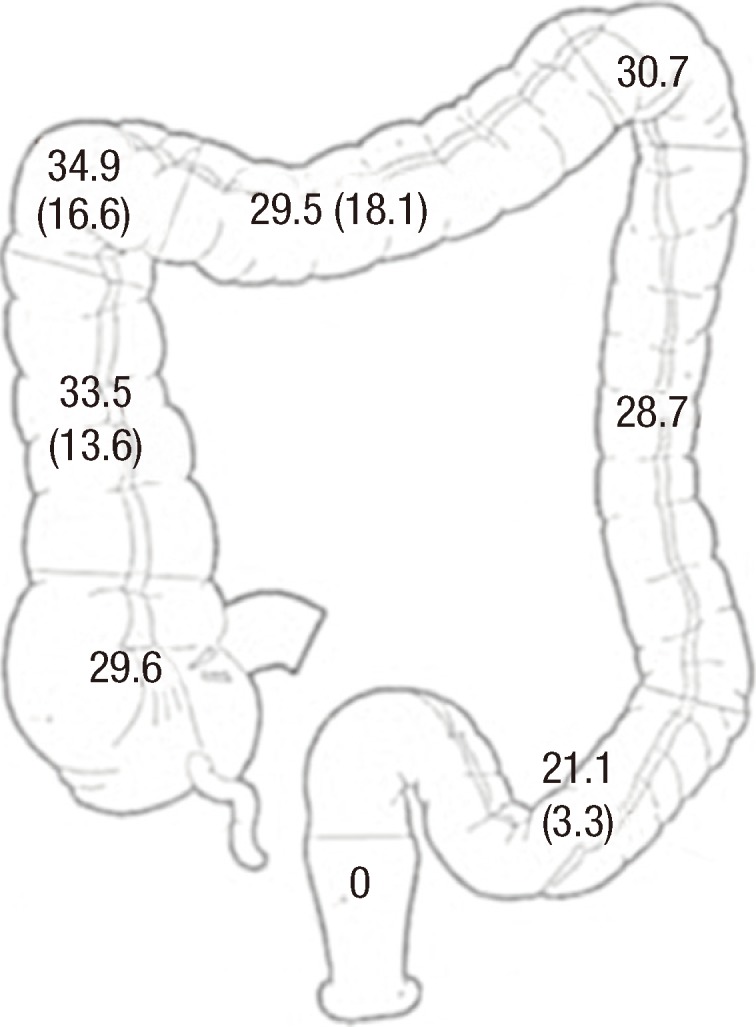
Miss rates according to polyp location are shown in Table 3 and Fig. 1. Miss rates for colorectal adenomas in the A-colon, HF-colon, D-colon, and SF-colon were 28.3%, 27.5%, 24.2%, and 23.5%, respectively. For advanced adenomas, the miss rates in the HF-colon, A-colon, and T-colon were 2.5%, 1.6%, and 0.9%, respectively.
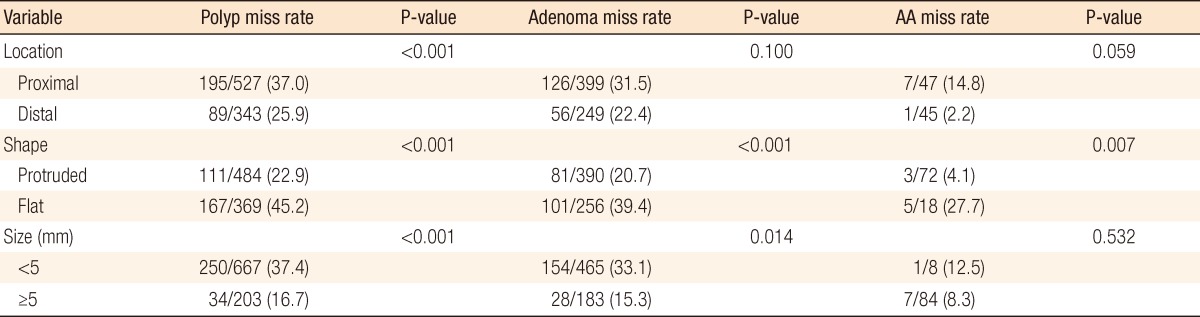
Characteristics associated with the polyp miss rate are shown in Table 3. The overall miss rate was significantly higher for polyps proximal, rather than distal, to the splenic flexure (37% vs 25.9%, P < 0.001). The miss rates for adenomas and advanced adenomas were higher in the proximal than in the distal colon, but the differences were not significant.
The miss rates were significantly higher for flat polyps (45.2%, P < 0.001), flat adenomas (39.4%, P < 0.001) and flat advanced adenomas (27.7%, P = 0.007) than for corresponding protrusive lesions. The miss rates for small (<5 mm) polyps (P < 0.001) and adenomas (P = 0.014) were significantly higher than those for larger lesions. The miss rate for advanced adenomas <5 mm was higher than for it was for larger adenomas, but the difference was not significant (P = 0.532).
Although colonoscopy is widely accepted as the gold standard for the detection of colonic neoplasia, some lesions are missed. The colorectal cancer diagnosis rate after a clearing colonoscopy is reported to be as large as 5% [5]. Tandem colonoscopy, in which patients underwent two colonoscopic examinations on the same day, showed that some lesions missed on the first colonoscopy were observed during the second [4, 6]. In contrast to these studies, which were performed in a planned research setting to reflect an ideal situation, our study was designed to assess miss rates and the relationship between the miss rates and the clinical characteristics in high-risk patients who underwent follow-up colonoscopy within 9 months after a polypectomy due to multiple polyps or an advanced adenoma. Despite the limitations of its retrospective design, we think that our study was more clinically practical because our patients were at high risk for metachronous colorectal neoplastic lesions including cancers. Reducing the miss rate in high-risk patients can, therefore, effectively reduce the incidence of metachronous colorectal cancers.
Colonoscopic miss rates were calculated according to both lesion-based and patient-based methods. According to the lesion-based method, a pooled miss rate can be defined as the total number of missed polyps relative to the total number of missed and initially detected polyps [2, 3, 6]. This method, however, cannot determine the per-person colonoscopic miss rate and, therefore, cannot help determine the proper follow-up time for each patient. In contrast, the patient-based method can help identify individual patients at high risk for missing polyps and, therefore, requiring a shorter follow-up interval. We observed a higher than expected per-patient miss rate of 65.3%, which may have been due to our selection of patients at high risk for colorectal polyps. The presence of multiple polyps on initial examination has been shown to be a strong predictor of both polyps and advanced polyps on subsequent colonoscopic examinations [1, 11]. In addition, the presence of multiple polyps was associated with an up to five-fold greater risk of synchronous carcinomas compared with the general population [12].
Patients with advanced adenomas have a high risk for metachronous colorectal neoplasia. We observed an overall adenoma miss rate of 20.9%, similar to previous reports of 20% and 24% [6]. We also observed a per-patient miss rate of initially advanced adenomas of 12.2%. In addition, eight advanced adenomas (including two in one patient) were detected on the second, but not the first, colonoscopy. Because such advanced polyps are unlikely to grow in 9 months, they must have been missed on the initial colonoscopic examination. No cancer was missed on repeat colonoscopies in the 102 patients studied.
Of the 182 missed polyps, 84.6% were <5 mm in diameter. The miss rates for adenomas <5 mm and for those Ōēź5 mm in diameter were 33.1% and 15.3%, respectively. Adenoma size has also been associated with miss rates in other series. For example, 15% of neoplastic polyps <6 mm were missed, compared with 7% of polyps >9 mm [2]. Similarly, the miss rate for adenomas Ōēź1 cm, 6-9 mm, and Ōēż5 mm were 6%, 13%, and 27%, respectively [6]. Although the clinical significance of small-sized adenomas is unclear, finding and removing polyps of any size during colonoscopic examination is required to decrease the adenoma miss rate.
We found that flat-type polyps were more likely to be missed than protruded-type polyps. Few reports have described the shapes of the missed polyps. One study showed that the miss rates for flat polyps and flat adenomas were 32% and 42%, respectively, significantly higher than those for protruded polyps and adenomas [3]. We found that polyp shape, particularly a flat pattern, is a determining feature, as 45% of flat polyps, 39% of flat adenomas and 27% of flat advanced adenomas were missed. Thus, repeat colonoscopy in patients at high risk for colorectal polyps should be done carefully to minimize the miss rate for flat adenomas.
We found that polyps in the proximal colon were more likely to be missed than polyps in the distal colon, although this difference did not reach statistical significance. In a comparison of colonoscopy and computed tomography colonography, the missed lesions were present on the proximal side of folds, the inner aspect of flexures, and the distal rectum [7], with miss rates higher in the deep folds of the A-colon, T-colon, hepatic flexure, and splenic flexure. Among the factors associated with lesions missed during colonoscopy are blind spots (especially at the flexure areas and the rectosigmoid junction), locations behind mucosal folds, and difficulty in maneuvering the scope through the sigmoid colon.
Our study had several limitations: 1) it was retrospective in nature, 2) it involved a small population at a single center, 3) no data were available on withdrawal time, 4) there was no comparison between endoscopists, and 5) especially, our results were derived from follow-up results within 9 months after the initial polypectomy, which may cause an exaggerated miss rate due to incomplete resection or newly developed polyps. A need exists to confirm our findings in a prospective study with surveillance colonoscopies such that the surveillance interval can be determined in patients at high risk for colorectal polyps. In addition, lesion miss rates may be reduced by meticulous maneuvers and technical advances to physically flatten folds or otherwise improve visualization behind folds; however, these maneuvers must be balanced with the need for efficient examination.
In conclusion, the miss rate for polyps in the high-risk group was greater than expected. Efforts to reduce miss rates, such as meticulous maneuvers and technical advances, are needed to improve the quality of colonoscopy. Also, early follow-up colonoscopy is mandatory, especially in patients at high risk.
Notes
References
1. Hixson LJ, Fennerty MB, Sampliner RE, McGee D, Garewal H. Prospective study of the frequency and size distribution of polyps missed by colonoscopy. J Natl Cancer Inst 1990;82:1769ŌĆō1772. PMID: 2231773.


2. Bensen S, Mott LA, Dain B, Rothstein R, Baron J. Polyp Prevention Study Group. The colonoscopic miss rate and true one-year recurrence of colorectal neoplastic polyps. Am J Gastroenterol 1999;94:194ŌĆō199. PMID: 9934755.


3. Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P, Potier P, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy 2008;40:284ŌĆō290. PMID: 18389446.


4. Hixson LJ, Fennerty MB, Sampliner RE, Garewal HS. Prospective blinded trial of the colonoscopic miss-rate of large colorectal polyps. Gastrointest Endosc 1991;37:125ŌĆō127. PMID: 2032595.


5. Haseman JH, Lemmel GT, Rahmani EY, Rex DK. Failure of colonoscopy to detect colorectal cancer: evaluation of 47 cases in 20 hospitals. Gastrointest Endosc 1997;45:451ŌĆō455. PMID: 9199899.


6. Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, et al. Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 1997;112:24ŌĆō28. PMID: 8978338.


7. Pickhardt PJ, Nugent PA, Mysliwiec PA, Choi JR, Schindler WR. Location of adenomas missed by optical colonoscopy. Ann Intern Med 2004;141:352ŌĆō359. PMID: 15353426.


8. Bond JH. Practice Parameters Committee of the American College of Gastroenterology. Polyp guideline: diagnosis, treatment, and surveillance for patients with colorectal polyps. Am J Gastroenterol 2000;95:3053ŌĆō3063. PMID: 11095318.


9. Lotfi AM, Spencer RJ, Ilstrup DM, Melton LJ 3rd. Colorectal polyps and the risk of subsequent carcinoma. Mayo Clin Proc 1986;61:337ŌĆō343. PMID: 3702494.


10. The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58(6 Suppl): S3ŌĆōS43. PMID: 14652541.


11. Winawer SJ, Zauber AG, O'Brien MJ, Ho MN, Gottlieb L, Sternberg SS, et al. The National Polyp Study Workgroup. Randomized comparison of surveillance intervals after colonoscopic removal of newly diagnosed adenomatous polyps. N Engl J Med 1993;328:901ŌĆō906. PMID: 8446136.


12. Olsen HW, Lawrence WA, Snook CW, Mutch WM. Review of recurrent polyps and cancer in 500 patients with initial colonoscopy for polyps. Dis Colon Rectum 1988;31:222ŌĆō227. PMID: 3349879.