Management of Colorectal Trauma
Article information
Abstract
Although the treatment strategy for colorectal trauma has advanced during the last part of the twentieth century and the result has improved, compared to other injuries, problems, such as high septic complication rates and mortality rates, still exist, so standard management for colorectal trauma is still a controversial issue. For that reason, we designed this article to address current recommendations for management of colorectal injuries based on a review of literature. According to the reviewed data, although sufficient evidence exists for primary repair being the treatment of choice in most cases of nondestructive colon injuries, many surgeons are still concerned about anastomotic leakage or failure, and prefer to perform a diverting colostomy. Recently, some reports have shown that primary repair or resection and anastomosis, is better than a diverting colostomy even in cases of destructive colon injuries, but it has not fully established as the standard treatment. The same guideline as that for colonic injury is applied in cases of intraperitoneal rectal injuries, and, diversion, primary repair, and presacral drainage are regarded as the standards for the management of extraperitoneal rectal injuries. However, some reports state that primary repair without a diverting colostomy has benefit in the treatment of extraperitoneal rectal injury, and presacral drainage is still controversial. In conclusion, ideally an individual management strategy would be developed for each patient suffering from colorectal injury. To do this, an evidence-based treatment plan should be carefully developed.
INTRODUCTION
The mortality of colorectal injury was higher than 90% during the U.S. Civil War (1861-1865), and it decreased to 40% during the Second World War (1941-1945) and noticeably to less than 10% through the Vietnam War. In the recent 100 years, the management of traumatic injury to the colon and the rectum was improved greatly. Nonetheless, the mortality rate is still 3%, and the abdominal sepsis rate is higher than 20%, proving that the management of colon injury is one of the important fields of trauma medicine that still requires further studies [1]. In addition, the choice of the treatment method for colon injury has changed greatly; nonetheless, many controversial areas still require attention. Especially, in Korea, colorectal subspecialty branches have become recognized more because of current trends in general surgery. Thus, surgeons who specialize in colorectal surgery should pay more attention to colorectal trauma. For all these reasons, in this study, the most recent trends in treatment of the colorectal injuries, as well as most controversies surrounding such treatment trends, have been thoroughly reviewed via an evidence-based literature review and analysis covering the last 30 years.
HISTORICAL BACKGROUND
A discussion of the historical changes that occurred because of the wars during the recent 100 years, and even earlier wars, is to be essential for understanding the general trend of treatments for traumatic colorectal injuries. The first record of traumatic colon injury is in the Old Testament (Book of judges 3, p.17-25), where Ehus stabbed Eglon with a knife, the colon was injured, feces were released due to the wound, and he ultimately died [2]. Medically relevant records from the U.S. Civil War (1861-1865) show that during the war, the standard treatment for colorectal injuries was non-surgical treatments; thus, the mortality rate was higher than 90%. With the introduction of anesthetic techniques and sterile surgical manipulation, surgical treatments for colorectal injury were initiated during the First World War (1914-1918), and primary repair was mainstreamed. At that time, the mortality rate was higher than 60%. During a similar time period, Wallace [3] treated 102 of 155 cases (66%) of gunshot wounds with colorectal injury by using primary repair and showed a 50% mortality rate, which was better than the 73.5% mortality rate for diverting colostomy cases. During a similar period, Fraser and Drummond [4] reported that primary repair showed better results except for cases with severe colorectal injury.
During the Second World War, the mortality rate of colorectal injury still remained high because more severe colorectal injuries were inflicted due to the advancements in firearms, such as high-velocity bullets, and due to inexperienced young surgeons. Thus the U.S. Surgeon General (USG) [5] enforced the treatment guideline that for colorectal injury, exteriorization or proximal diversion must be performed. In England, similarly, Ogilvie [6] enforced compulsive proximal diversion; consequently, a noticeable reduction of the mortality rate (35%) was shown. At that time, Imes [7], Tayler and Thompson [8], and Gordon-Taylor [9] reported that in elective cases, primary repair showed better results. Nevertheless, during the same period, Hurt [10] and Mason [11] reported that proximal diversion was safe and had many advantages. Thus, at the time of the Second World War, the standard treatment for colorectal injury was proximal diversion. Afterward, through the Korean War and the Vietnam War, because of the rapid transport of injured soldiers and improvement in patient management, as well as development of new antibiotics, the mortality and the morbidity rates were noticeably reduced.
In addition to the above, low-speed bullets are causing major colon injuries in peace time, and the trend toward increasingly performing a proximal diversion for traumatic colon injury has continued without scientific evidence. This phenomenon is due to surgeons who returned from war and who had become too familiar with war-time guideline and had accepted the proximal diversion as the standard treatment for traumatic colorectal injury, even during peace time [12]. In 1951, Woodhall and Ochsner [13] reported a study on primary repair and proximal diversion performed for traumatic colorectal injury, and the mortality rates were 9% and 40%, respectively. Thus, the primary repair showed noticeably good results during peace time. In 1979, Stone and Fabian [14] showed significant results for primary repair through prospective randomized studies, which was contradictory to the past guideline. For approximately a 30-year-time period, several prospective studies on the treatment of traumatic colorectal injury showed that primary repair, as well as resection and anastomosis, had become a new trend in treatment methods, and they became rapidly emerging methods [15-18].
Recently, treatments for traumatic colorectal injuries have improved markedly based on scientific evidence. Nonetheless, excessive proximal diversions are still being performed, because of a vague anxiety about the primary repair, as well as the resection and anastomosis.
TREATMENTS FOR COLORECTAL INJURY
General care
Comparable to patients with other general trauma, patients with traumatic colorectal injury should be first evaluated and treated for injury that may threaten life, sufficient resuscitation by fluid and transfusion is required, and efforts should be made to reduce hypothermia, hypotension, shock, and acidosis, all of which can influence the morbidity and the mortality rates. Next, tests and evaluation that assess colorectal injury are required. For critical patients, movement of the patient should be limited; thus, physical examination cannot be performed efficiently.
Injuries from the back-side can be missed easily due to the patient's condition, so more a thorough physical examination needs to be carried out. Also, accurate assessment is required to see whether other injuries are present, to diagnosis underlying diseases, and to clearly evaluate the mechanism of trauma. In addition, it is necessary to understand the interval from trauma time to surgery. In operating rooms, in order to achieve an objective evaluation of the level of fecal contamination within the abdominal cavity, accurate exploratory open abdominal surgery including other organs is required, and an evaluation of the possibility of injury to the colon located in the retroperitoneum is required.
Colon injury grading scales
To select treatment methods for colon injury, first, colon injury grading scales that evaluate the level of colon injury should be accurately understood. As grading scales limited to colon injury, two systems, the Flint scale prepared by Flint et al. [19] and the colon injury scale (CIS) of the American Association for the Surgery of Trauma (AAST) [20, 21], are frequently applied (Table 1). The two scales are applied to quantify and objectify the level of colon injury. Based on them, the level of colon injury can be objectified by classifying colon injuries as destructive colon injuries or non-destructive colon injuries. Other evaluation tools, such as the Penetrating Abdominal Trauma Index (PATI), show address associated injuries to other organs and are helpful in evaluating the overall seriousness of the trauma [20, 21].
Treatments for penetrating colon injuries
Generally, colorectal injuries can be categorized as penetrating, blunt, and iatrogenic injuries, and treatment methods may differ depending on the mechanism of colon injuries. Most traumatic colon injuries have been reported to be caused by penetrating trauma, and colon injury is associated in 20% of abdominal penetrating traumas [12]. Penetrating traumas are gunshots and stabs in most cases. Gunshots can be divided into injuries caused by high-speed bullets and by low-speed bullets. High-speed bullets are known to be related with more associated organ injuries and wider soft tissue damage. During war times, injuries caused by high-speed bullets and explosives are more frequent, and during peace times, injuries are caused by low-speed bullets primarily. In recent trends, even during peace times, high-speed-bullet injuries have been increasing. In case of gunshot injury, the ascending colon and the transverse colons are more frequently injured, and multiple colon injuries may be associated.
Comparing the gunshots to the stabbings in cases of penetrating injuries, in the United states, gunshot injuries are predominant (gunshot wounds:stabbings = 10:1) [22], but in Korea, out of 47 penetrating injuries, only a single gunshot wound was noted, making stabbings absolutely the dominant injury mechanism [23-27]. In gunshot injuries, exploratory open abdominal surgery is required because 95% of the cases involve intra-abdominal organ injuries. In stabbing injuries, selective surgical observation can be used because only 50% of the cases involve intra-abdominal organ injuries, although exploratory open abdominal surgery can be performed as well [12].
Treatments for non-destructive colon injuries
In the treatment of the colon injuries, whether the primary repair and the proximal diversion is selected will depend on the severity of the colon injury. Maxwell and Fabian [28] classified colon injuries as non-destructive colon injuries and destructive colon injuries. Non-destructive colon injuries correspond to Flint grades 1 and 2 and to CIS grades 1-3, and in many cases, primary repair can easily be done.
In 1979, Stone and Fabian [14] provided evidence for the first time that the primary repair was superior to the colon diversion through a prospective randomized study conducted on selective patients, excluding risk factors. Since then, several prospective studies and prospective randomized studies have been conducted. Chappuis et al. [29] reported that in a prospective randomized study without exclusion of risk factors conducted on 28 patients in the primary repair group and 28 patients in the proximal diversion group, the primary repair showed less intra-abdominal sepsis, regardless of risk factors (the number of associated injuries, the level of fecal contamination, with or without shock, and transfusion volume). Demetriades et al. [30] conducted a prospective, non-randomized study involving the treatment of 100 cases of gunshot colon injury in which the primary repair was performed on all cases except cases requiring resection of the colon or cases with severe intra-abdominal contamination, without considering other risk factors, and they showed that the primary repair group presented good treatment outcomes compared to the proximal diversion group (11.8% vs. 29.2%, respectively).
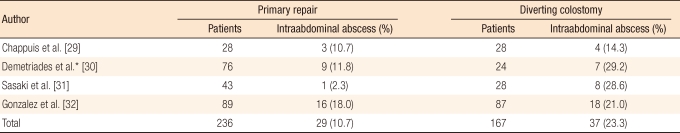
In four prospective or prospective, randomized studies [29-32], the primary repair group presented better results than the proximal diversion group (10.7% vs. 23.3%, respectively) (Table 2). By reviewing other prospective and retrospective studies, Maxwell and Fabian [28] reported that the primary repair group presented better results compared to the proximal diversion group not only for complications (14% vs. 31%) but also for intra-abdominal sepsis (5% vs. 12%) and mortality rate (0.11% vs. 0.14%). Therefore, based on several prospective and retrospective studies, one can conclude that in non-destructive colon injuries, primary repair should be the standard treatment regardless of associated risk factors. Nevertheless, despite such a scientific basis, as shown by a survey of 317 Canadian surgeons conducted in 1999 [33], even in cases of colon injuries caused by low-speed bullets, 75% of the surgeons still performed proximal diversion to treat colon injuries. This fact implies that surgeons are still being driven by a past preference for the proximal diversion.
Treatments for destructive colon injuries
Destructive colon injuries are injuries corresponding to Flint grade 3 or CIS grades 4-5, and such injuries require resection. The causes of such injuries are high-speed bullets and explosives; safety belts cause abdominal blunt injuries. During the peace time, 80-90% of colon injuries are non-destructive colon injuries [12]. In contrast, in war time, 72% of colon injuries are destructive injuries [34]. In most cases (60-93%) [35] of non-destructive colon injuries caused by penetrating trauma, the primary repair is the standard treatment without considering the risk factors, but guidelines for the treatment of destructive colon injuries are still controversial due to their lower incidence rate and the lack of definitive data.
Maxwell and Fabian [28] reviewed two prospective studies and three prospective, randomized studies and found the incidence rates of overall complications, intra-abdominal abscess, and anastomosis leakage to be 35%, 23%, and 3.1%, respectively. In addition, no mortalities were reported for the 65 patients who underwent end-to-end anastomosis after the colon resection. According to the guideline of the Eastern Association for the Surgery of Trauma (EAST guidelines, 1998) [36], even in destructive colon injury cases, if patients are hemodynamicaly stable during surgery, have fewer associated injuries (PATI < 25, Injury Severity Score < 25), do not have severe peritonitis, and have with no prior underlying medical diseases, the end-to-end anastomosis after the colon resection is recommended without the proximal diversion. In cases of shock or severe associated diseases with severe peritonitis and with prior underlying medical diseases, the colon resection and the proximal diversion are the standard treatments. However, the guideline is not based on sufficient evidence (class III evidence), and it has clear limitations. Demetriades et al. [37] conducted a multicenter, randomized, prospective study to augment the guideline. Out of 297 destructive colon injuries, on 197 patients, anastomosis was done after the colon resection, and on 100 patients, proximal diversion was performed. The results showed that in the patient group receiving anastomosis after the colon resection, 13 cases (6.6%) developed anastomosis leakage, and in the patient group receiving proximal diversion, 1 case presented with anatomosis leakage. In the univariate analysis, intra-abdominal complications were increased in cases treated with a single prophylactic antibiotic, in cases with severe intra-abdominal fecal contamination, and in cases with transfusions of more than 4 units. In the multivariate analysis, the mortality rates and the incidences of intra-abdominal sepsis between the two groups, without regarding the risk factors, were not different. Thus, even for destructive colon injury cases, the colon resection followed by anastomosis without the proximal diversion has been recommended as the standard treatment. Therefore, even though in cases of destructive colon injury, the primary repair or the end-to-end anastomosis after the colon resection is usually performed in selected patients, the selection of the correct treatment for destructive colon injuries is still a subject of controversy and depends on associated risk factors, injury mechanism, anatomical site, and severity. In the future, more studies are required to address this debate.
Treatments for blunt colon injuries
Approximately 4% of colon injuries are caused by blunt trauma, mostly traffic accidents [38]. Blow out injuries by seat belts and wheels are the most common, ischemia is developed due to vascular injuries, and delayed colon perforation may occur. Therefore, the possibility of delayed colon perforation should be kept in mind. The injuries caused by blunt trauma frequently occur in the movable areas of the colon, such as the cecum, the transverse colon, and the sigmoid colon, and secondary injuries caused by mesenteric devascularization frequently happen in the right-side colon. Blunt injuries to the perineum may cause detachments of the rectosigmoid junction and the surgical anal canal from the levator muscle sling [39, 40]. The possibility of delayed diagnosis of colon injury caused by blunt trauma is higher than it is for colon injury caused by penetrating trauma, and associated organ injuries are severe; thus, high morbidity and mortality rates are shown [35]. In penetrating injury cases, 60-93% are treated with primary repair or with resection and anastomosis [35]. Regarding treatments for colon injuries caused by blunt trauma, according to the study reported by Miller and Schache [41], primary repair could be performed only in 39% of the cases; thus, for colon injury cases caused by blunt trauma, proximal diversion is performed more frequently.
In blunt traumatic colon injuries, delayed perforations may found a few days later, and in case of severe fecal contamination during the operation and septic conditions, resection and diverting colostomy are preferred rather than the primary repair [12]. In cases with destructive colon injuries, hypovolemic shock, severe intra-abdominal fecal contamination, old age, associated severe underlying medical disease and less experienced trauma centers, the proximal diversion is performed more frequently for blunt-trauma colon injuries [18, 42]. Carrillo et al. [40] reported that complications between the group who received end-to-end anastomosis after resection and the group who received proximal diversion after resection were not different. Nevertheless, for patients with unstable vital signs, cases with severe fecal contamination, and cases with severe associated extra-abdominal organ injuries, proximal diversion is recommended. Fallon [42] explained that the proximal diversion would be performed on the abdominal blunt trauma patients rather than on penetrating trauma patients because the former has more associated organ injuries.
TREATMENT FOR RECTAL INJURIES
Treatments for penetrating rectal injuries
Since the Second World War, the fundamental principles of treating rectal injuries have been the proximal colon diversion, the primary repair, and the presacral drainage (PSD) [43]. Two more treatments, distal rectal washout (DRWO) and primary repair without proximal colon diversion, were introduced afterward. However, controversy still exists [44, 45]. Shannon et al. [46] reported that the DRWO showed promising results and was most effective in cases with high-energy pelvic crush or large-caliber handgun injuries. A study by Burch et al. [47] and other studies provided no definite evidence for the efficacy of the DRWO [45, 48, 49]; a small number of cases required only primary repair without proximal diversion for rectal injuires.
Depending on the anatomical location of the rectal injury, such injuries can be classified as intraperitoneal and extraperitoneal rectal injuries. The former can be treated with the standard treatment for colon injuries, which is the primary repair, while the latter may be treated with the primary repair without proximal diversion, and no anastomotic leakage has been reported [28, 45, 48, 50]. However, because of the small number of cases, its effectiveness needs to be confirmed by follow-up studies in near future. The PSD is also a subject of debate. For example, there are numerous studies proving the advantages of PSD, but only Burch et al. [47] reported statistically significant results. In contrast, Gonzalez et al. [51] reported in a prospective, randomized study that in only the proximal colon diversion without PSD group, did the mortality and the morbidity rates not increase. This raises the question whether PSD is really required. In cases of destructive rectal injuries, where the presacral area is severely contaminated, PSD would be the effective treatment [35]. Cleary et al. [35] proposed a treatment algorithm for penetrating trauma cases; in this algorithm, when the rectal injury site cannot be treated with the primary repair or cannot be identified in cases of destructive extraperitoneal rectal injuries, the proximal colon diversion and PSD seem to be the appropriate treatments. However, in less severe cases without serious associated injuries or with no underlying medical diseases, the primary repair without proximal colon diversion is the more appropriate treatment.
Treatments for blunt rectal injuries
Rectal injuries caused by blunt trauma are associated with pelvic blood vessel injuries and with bladder or ureter injuries; thus, high mortality and morbidity rates are shown. When complex injuries, such as severe pelvic injuries, injuries in the peritoneal area, pelvic vascular injuries, and pelvic bone injuries, occur, multidisciplinary treatment is required.
Because the mortality rate of rectal injuries caused by blunt trauma is more than 50%, which is higher than the mortality rate of colon injuries caused by blunt trauma (17%) and because the possibilities of associated rectal injuries is higher, more attention needs to be paid to patients with pelvic fractures or peritoneal injuries [52]. In regard to the principle of treatment and to existing controversies, intraperitoneal rectal injuries are similar to colon injuries. Treatments for extraperitoneal rectal injuries caused by blunt trauma follow the treatment principle for extraperitoneal rectal injuries caused by penetrating injuries, and the points of controversy are similar.
ASSOCIATED RISK FACTORS & CONTROVERSIAL ISSUES
In regard to the treatment for colorectal injuries, the controversial points are indications for proximal diversion, resection and anastomosis, or primary repair in destructive colorectal injuries, selection of treatment depending on the associated risk factors, different treatment approaches for different anatomical locations (left-/right-side colon injuries), and effectiveness of DRWO and PSD in extraperitoneal rectal injuries. However, here, only the selection of treatment based on associated risk factors and different treatment approaches for different anatomical locations (left-/right-side colon injuries) will be discussed without mentioning the other controversial issues.
Risk factors influencing the morbidity and the mortality rates after colon injuries are hypotension, the presence of shock and excessive transfusion, the level of intra-abdominal contamination at the time of surgery, the interval from injury to surgery, and associated organ injuries. Generally, these risk factors influence the overall morbidity and mortality rates. Nonetheless, whether they exert effects on the morbidity rate that are directly associated with colon injuries and anastomotic leakage is still controversial.
In non-destructive colon injuries, it is already a known fact that after primary repair, some risk factors raise the overall morbidity rate, but none of the risk factors affect on anastomosis leakage [30, 32, 53, 54]. However, in destructive colon injury, there are several contradictory reports on the risk factors causing anastomotic leakage, which causes controversy. In several studies, shock and hypotension increased the overall incidence and the risk for intra-abdominal abscess [32, 55, 56].
Transfusion elevates the overall incidence of complications and sepsis in both destructive and non-destructive colon injuries, although there are no reports on raising the risk of anastomostic leakage in non-destructive colon injuries [54-56]. In regard to the risk of transfusion for anastomostic leakage, Stewart et al. [57] recommended the colon diversion when a transfusion of more than 6 units is received during surgery. On the contrary, Demetriades et al. [37] reported that a transfusion of more than 4 units within 24 hours increased the rate of intra-abdominal infection without causing anastomostic leakage, and Maxwell and Fabian [28] favored the primary repair regardless of transfusion amount.
Intra-abdominal contamination is known to increase the incidence of sepsis and the risk for intra-abdominal abscess [28, 53, 56]. However, in a prospective study in which thorough irrigation of the intra-abdominal cavity was performed, there was no difference in the septic complications between two groups, the group with severe intra-abdominal contamination and the group without it. Demetriades et al. [37] reported that in destructive colon injury patients with severe intra-abdominal contamination, the risk for anastomosis leakage was not different; thus, proximal diversion should not be selected based on the level of intra-abdominal contamination only [28, 32, 43]. The number of associated organ injuries (PATI) is known to increase infectious complications, as well as non-infectious complications, but without increasing incidence of anastomotic complications [28, 29, 31, 32, 42, 43, 52, 54, 57-59].
As for the interval from injury to surgery, prospective, randomized studies showed that an interval of less than 4 to 6 hours is not a risk factor in either destructive colon injuries or non-destructive colon injuries [29, 31, 32]. Nonetheless, Maxwell and Fabian [28] recommended the proximal diversion for destructive colon injury patients with severe intra-abdominal fecal contamination whose surgery had been delayed for longer than 6 hours and for non-destructive colon injury patients with severe peritonitis or hypotension whose surgery had been delayed for longer than 12 hours. Thus, this issue is has also been controversial.
For the treatment of right colon injuries and left colon injuries, it has been believed generally that right colon injuries have better outcomes. Nonetheless, Thompson and Moore [60] reported that in penetrating injury cases, the selection of the treatment method for right colon injuries and left colon injuries was not different. Stewart et al. [57] reported that in destructive colon injury cases, development of anastomosis leakage and intra-abdominal abscess in the two groups was not different. Demetriades et al. [61] reported that in cases without severe fecal contamination or severe tissue damages and in cases without abundant feces within the colon, regardless of the location of the colon injury, the primary repair could be performed safely, thus causing controversy. Nonetheless, a general consensus exists that the treatment methods for right colon injuries and left colon injuries need to be differentiated [12].
CONCLUSION
If colon injuries caused by trauma are not treated appropriately, severe complications leading to death may be induced; nonetheless, controversy still exists concerning the standard treatment. In this regard, unnecessary proximal diversions should be avoided, and in order reduce irreversible complications, the selection of conservative treatments or primary repair without evidence should be avoided. The treatment method should be selected based on considerations of diverse risk factors, such as the injury mechanism, the severity of colon injury, the general condition of the patient, the interval from injury to surgery, whether or not vital signs are stable, whether or not excessive transfusion was needed, the level of fecal contamination, and associated organ injuries. In other words, the therapy for each colorectal injury should be individualized. A more thorough selection of treatment based on more evidence-based studies is needed.
Notes
No potential conflict of interest relevant to this article was reported.