Is Conservative Treatment with Antibiotics the Correct Strategy for Management of Right Colonic Diverticulitis?: A Prospective Study
Article information
Abstract
Purpose
The goals of this study were to identify whether conservative treatment with antibiotics in right colonic diverticulitis (RCD) patients, our empirical method used until now, is adequate and to determine how the natural history of RCD is affected by conservative treatment.
Methods
This study was designed as a case-control study. Group I was comprised of 12 patients who were managed conservatively, and clinical data were retrospectively collected. In group II, a total of 49 patients, diagnosed by using diagnostic criteria for RCD and managed conservatively, were prospectively included.
Results
The period of fasting was 2.7 days, and the hospital stay was 4.6 days in all patients. The intravenous and the oral antibiotic periods were 3.8 days and 9.8 days, respectively. There were no statistically significant differences in treatment results between the two groups except the duration of fasting and the hospitalization, and there were no complications under conservative treatment. Eight patients (13.1%) had recurrent diverticulitis during the follow-up period. The recurrence risk showed no significant difference between the groups. The RCD-free period after management was 60.1 months, and patients with recurrent RCD were treated by conservative treatment or laparoscopic surgery.
Conclusion
Conservative treatment with antibiotics is the optimal treatment of choice for RCD and shows no increase in complications.
INTRODUCTION
Right colonic diverticulitis (RCD) is an unusual disease in Western countries, but it exhibits higher incidence in Asian countries [1-4]. Treatment strategies for RCD have been difficult to define due to its low diagnostic accuracy [5]. Aggressive surgical treatment is advocated by some investigators decrease incidence of complications associated with conservative treatment [6-9]. However, recent reports have shown comparable results for conservative medical treatment of uncomplicated RCD, and the results are considered as acceptable because of the benign and self-limited natural history of RCD [5, 10-12].
A previous comparative study of treatment modalities, conservative antibiotics treatment, surgical treatment, and appendectomy, demonstrated no difference in the frequency of complications or the recurrence rates [5]. Moreover, most RCD patients had multiple diverticula in the colon. If it is diagnosed preoperatively, uncomplicated RCD can be managed conservatively with intravenous antibiotics. However, segmental resection is advocated as the most effective treatment when it is diagnosed intraoperatively. Surgical intervention is also beneficial in the aspect of recurrence. Previously, a set of diagnostic criteria for RCD that increased the preoperative diagnosis rate up to 85 percent was proposed, and that set was applied in this study [13], which was aimed to evaluate prospectively the clinical implications in RCD patients receiving conservative treatment with antibiotics.
METHODS
Patients
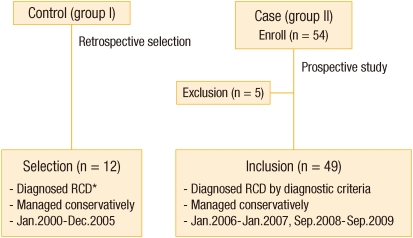
This study was designed as a case-control study to verify that there's no difference between the control group and the case (experimental) group. The flow chart of patient selection is presented below (Fig. 1).
The control group (group I) was comprised of 12 patients who were managed conservatively after making a diagnosis of RCD at the Department of Surgery, St. Mary's Hospital, The Catholic University of Korea School of Medicine, from January 2000 to December 2005. Clinical data for the control group were retrospectively collected based on medical records.
A total of 54 patients, diagnosed using the established diagnostic criteria for RCD [13], were enrolled as case group (group II) from January 2006 to 2007 and from September 2008 to 2009. Subsequently, a total of 49 patients were included, and clinical data for those were prospectively collected for analysis.
The median follow-up time was 15.1 months (range, 1 to 90 months). All patients included provided informed consent upon entering the study. This study was approved by the Institutional Review Board of Ethical Committee of the College of Medicine (SC10OESI0079).
Diagnosis
The RCD was confirmed by using abdominal ultrasound or computed tomography (CT) and barium enema (BE) in both groups. Abdominal ultrasound or CT was checked in patients complaining of symptoms at admission, and BE was performed in the outpatient clinic after discharge.
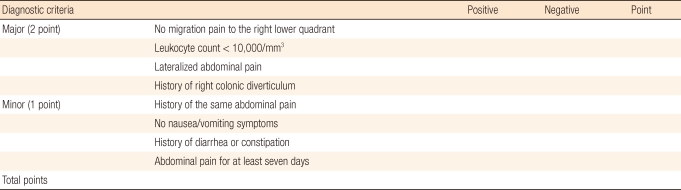
The diagnostic criteria for RDC were mentioned in Table 1 [13]. Each major criterion was given a score of two points; a minor criterion received one point. An abdominal CT scan was performed following informed consent if the total number of points exceeded two. Major diagnostic criteria included 1) non-migratory pain to the right lower quadrant; 2) a leukocyte count < 10,000/mm3; 3) lateralized abdominal pain; and 4) a history of right colonic diverticulum diagnosed by using BE or colonoscopy. Minor diagnostic criteria included 1) a history of right lower quadrant abdominal pain, 2) no symptoms of nausea or vomiting, 3) symptoms of constipation or diarrhea, and 4) abdominal pain for at least seven days.
Recurrence of RCD was defined as a condition in which abdominal pain recurred and antibiotic therapy was needed based on radiologic findings after first management. Classification of a diverticular abscess was made as proposed by Hinchey [14].
Treatment
Conservative treatment for the patients with group I included 1) broad-spectrum antibiotics or 2) percutaneous drainage (PCD) in patients with a large abscess. The patients with group II received a combination therapy of second generation cephalosporin, aminoglycoside, and metronidazole during the hospitalization periods and oral antibiotics for 7 days after discharge. If abdominal tenderness persisted, patients took oral antibiotics for a longer period. Oral intake of foods was started if there was no abdominal pain even when abdominal tenderness was present.
Statistical analysis
The clinical characteristics were compared in both the two groups. The results for continuous variables are expressed as mean ± standard deviation. A univariate statistical analysis was performed using the Mann-Whitney U-test for continuous independent samples and the chi-square or Fisher's exact test for categorical variables. Probabilities of recurrence were computed using the Kaplan-Meier method with the log-rank test. The statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA), and a P-value < 0.05 was considered to indicate a statistically significant difference at the 95% confidence interval.
RESULTS
Clinical characteristics
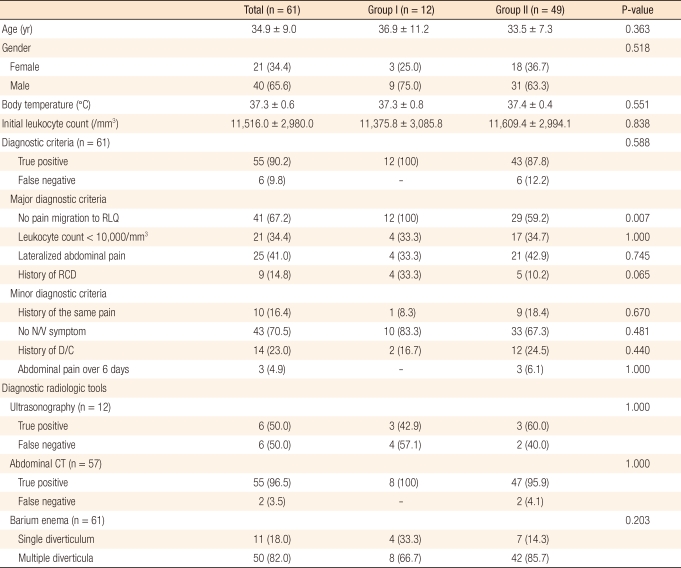
The clinical characteristics of included patients are presented Table 2. The male-to-female ratio of the patients with RCD was 1.9:1, and the mean age was 37.4 ± 1.1 years. No migratory pain in right lower quadrant (RLQ) was observed in 41 patients (67.2%) of the 61 patients in the two groups (12 in group I and 29 in group II), and the difference between the two groups was statistically significant (P = 0.007). There were no differences between group I and group II except for the symptom of migratory pain.
Using diagnostic criteria, RCD could be diagnosed in 55 patients (90.2%) of the 61l patients in the two groups. The mean scores for the diagnostic criteria were 4.3 ± 1.7 points.
Diagnostic radiographic findings
Ultrasound was performed in 12 patients and abdominal CT in 57 patients (Table 1). To confirm diverticulum, a BE was performed after 37.9 ± 13.9 days, and it presented multiple diverticula in 50 patients (82.0%). The locations of the diverticula were confined to the cecum in nine patients (14.8%) and to the ascending colon in twenty-one patients (34.4%), were found in both the cecum and the ascending colon in twenty-two patients (36.1%), ranged from the cecum to the transverse colon in four patients (6.6%), and expanded throughout the entire colon in five patients (8.2%). According to Hinchey's classification for complicated diverticulitis, only seven patients (11.5%) were diagnosed as stage I.
Clinical results of conservative treatment
There were statistically significant differences between the two groups in duration of nil per os (NPO) and hospitalization, with the duration of NPO and the hospitalization being significantly shorter in group II (P < 0.001) (Table 3). In seven patients with complicated RCD, six received conservative medical treatment, and only one patient with a large abscess underwent CT-guided PCD. There were no serious complications following the procedure.
Long-term outcomes after conservative treatment
Eight patients (13.1%) had recurrent diverticulitis during the follow-up period. However, there was no significant difference in recurrence between groups (P = 0.650). The difference of recurrence risk between groups was also not statistically significant (P = 0.602) (Fig. 2). The estimated RCD-free period after management was 60.1 months (limited to 90-month follow-up).

Probability of recurrence after first treatment in all patients (A) and according to groups (B). The Kaplan-Meier estimated recurrence risk was not significantly different between the retrospective study group (group I) and prospective study group (group II) (P = 0.602).
Among recurrent patients, six were managed by conservative treatment with bowel rest and intravenous antibiotics and were discharged without specific sequela. One patient underwent an emergency laparoscopic diverticulectomy because of a pericolic abscess at 18 months after the initial diagnosis, and another patient underwent a laparoscopic right hemicolectomy because of multiple diverticla. There was no morbidity or mortality.
DISCUSSION
The adequate treatment strategy for RCD has been controversial. Some studies have reported that conservative medical treatment would be complicated by high recurrence rates [6-9]. However, recent studies have reported that conservative medical treatment has acceptably low recurrence rates and is sufficient for treatment of recurrent RCD without complications and without the need for surgery [5, 10-12]. We previously reported that no differences in the rates of complications and recurrence existed between the conservative medical treatment and the surgical treatment groups. We also recommended adequate surgical correction in elective base after conservative medical treatment due to the high incidence of multiple diverticula [13]. Moreover, another study suggested that conservative medical therapy is a safe and effective treatment method [5], but these results were limited by the study being a retrospective analysis. Therefore, we performed this prospective study using a single arm setting.
In this study, all RCD (including complicated type I disease) patients were treated without specific sequela and revealed acceptably low recurrence rate (16.7%) after conservative medical management. Recurrent patients could be treated by using conservative treatment, followed by staged surgery only in selected patients. Recurrent patients underwent laparoscopic surgery, with additional information regarding the locations and the number of right colonic diverticula.
In this study, no significant differences in any data except for the symptom of migratory pain into RLQ were observed. These results are consistent with previous results that conservative medical treatment for RCD was beneficial, and provide further evidence that earlier results were not due to selection bias and may be correct [5, 10-12].
In methods of conservative medical treatment, sequential therapy by using intravenous and oral antibiotics for at least 3 and 7 days, respectively, was reported to be consistent with the results of 2.0 days of bowel rest and 4.2 days of hospital stay [10]. In this study, the periods of NPO and hospital stay were 2.7 days and 4.6 days, respectively. If the time to recovery is considered, however, the periods of treatment and hospitalization are shortened; the normalizations of fever and leukocyte counts occurred after 0.7 and 1.2 days, respectively.
Conservative treatment usually ranges from 1-2 weeks in duration. Broad spectrum antibiotics have generally been recommended for use in the treatment of diverticular disease because the colonic flora is comprised of aerobes and anaerobes [15]. A variety of antibiotic regimens have been proposed. If symptoms are severe, however, the use of 1) a combination of ciprofloxacin and gentamicin or metronidazole; 2) amoxicillin/clavulanic acid; or 3) sulfamethoxazole/trimethoprim is recommended. Ampicillin, gentamicin, metronidazole, piperacillin, and tazobactam have also been successfully used in clinical practice for patients with severe and complicated diverticulitis whereas ciprofloxacin, metronidazole, and rifaximin have been successfully used in cases of uncomplicated diverticulitis [16]. Recently, based on the theory that some of the pathogenesis of colon diverticulitis are similar to those involved in inflammatory bowel disease, some studies have recommended the use of mesalazine in the treatment of diverticulitis [15].
This study establishes diagnostic criteria for RCD. As in a previous report, performing a CT scan after the application of the diagnostic criteria for RCD increased the accuracy of the preoperative RCD diagnosis [13]. This study demonstrated a preoperative diagnostic accuracy of 85.7%. Use of these criteria allows for the application of principles derived from conservative medical management for sigmoid diverticulitis. In conclusion, the results of this study were similar to those from previous studies examining the management of RCD, and conservative treatment with antibiotics is the treatment of choice for RCD and can be used without increasing the complication rate.
Notes
No potential conflict of interest relevant to this article was reported.