- Search
Abstract
Purpose
The aim of this study was to evaluate the prognostic effectiveness of multivisceral resections of organs involved by locally advanced colorectal cancer.
Methods
A retrospective study was performed to analyze the data collected for 266 patients who underwent a curative resection for pT3-pT4 colorectal cancer without distant metastasis from January 2000 to December 2007. Of these 266 patients, 54 patients had macroscopically direct invasion of adjacent organs and underwent a multivisceral resection. We evaluated the short-term and the long-term outcomes of a multiviceral resection relative to that of standard surgery.
Results
The most common location for the primary lesion was the rectum, followed by the right colon and the sigmoid colon. Among the combined resected organs, common organs were the small bowel, ovary, and bladder. In the multivisceral resection group, tumor infiltration was confirmed histologically in 44.4% of the cases while in the remaining patients, a peritumorous adhesion had mimicked tumor invasion. Postoperative complications occurred in 17.5% of the patients who underwent standard surgery vs. 35.2% of those who underwent a multivisceral resection (P < 0.0001). But the survival rate of patients after a multivisceral resection was similar to that of patients after standard surgery (5-year survival rates: 61% vs. 58%; P = 0.36).
Conclusion
For locally advanced colorectal cancer, multivisceral resection was associated with higher postoperative morbidity, but the long-term survival after a curative resection is similar to that after a standard resection. Thus, a multivisceral resection can be recommended for most patients of locally advanced colorectal cancer.
According to the annual report of the Cancer Registry of the Ministry for Health, Welfare and Family Affairs of Korea published in December 2009 [1, 2], colorectal cancer accounts of 12.7% of all cancers, and the trend is for an approximately 6.4% annual increase [1]. Because the life style in Korea has become westernized, the incidence of colorectal cancer is on the rise. The national program for the early detection of colorectal cancer, which is one of 5 major cancers in Korea, recommends that the guaiac test be performed annually on both males and females older than 50 years, and if an abnormality is detected, that perform colonoscopy or a double-contrast barium enema study be perfomed.
However, colorectal cancer is a disease preferentially occurring in the population older than 60 years. In Korea, it is diagnosed as symptomatic and advanced stage cancer in many cases rather than as early cancer through the use of an early diagnosis program for colorectal cancer [2]. Thus, it is usually diagnosed as locally advanced colorectal cancer, and tumor infiltration or adhesion is detected during surgery. Consequently, an en-bloc resection, a radical resection including adjacent organs and structures, is required [3-14].
In locally advanced colorectal cancer, when a multivisceral enbloc resection is selected, postoperative morbidity and an increase in mortality should be considered. Particularly, for elderly patients, patients whose risk level for surgery is high, and patients requiring a technically difficult combination of resections involving organs such as intrapelvic organs, the pancreas, etc., the decision to use a multivisceral resection must be made carefully [3, 4]. In our study, the characteristics of patients who underwent a multivisceral resection for suspicious local infiltration to adjacent organs other than primary organs were examined, and the risks of a multivisceral resection and the difference in prognoses between a multivisceral resection and standard surgery were examined.
From January 1, 2000, to December 31, 2007, a total of 356 colorectal cancer patients underwent surgery. Among pT3-pT4 stage patients, excluding patients with distant metastasis at the time of diagnosis, patients with recurrent or synchronous cancer, and patients who had undergone a palliative colostomy instead of a colon resection, 266 patients were examined retrospectively.
As preoperative diagnosis methods, colonoscopy, abdominal ultrasound, abdominal CT, etc. were applied, and all cases were operated on by a single surgeon using the open method. Clinicopathological findings were analyzed by using the hospital records, and follow-up information was obtainded from visits to outpatient clinics and telephone surveys.
The 266 patients were divided into a group of patients who did not have infiltration to adjacent organs and who underwent a standard resection (212 patients) and a group of patients who were suspected of having invasion to neighboring organs and who, thus, underwent a multivisceral resection (54 patients), and the age, gender, location of the primary lesion, tumor size, infiltration depth, stage, histological type and differentiation grade were analyzed. In addition, for cases in which tumor infiltration was suspected macroscopically, actual tumor infiltration was examined pathologically. In addition, the incidences of postoperative complications in the group that underwent a standard resection were analyzed and compared with those in the group that underwent a multivisceral resection, as were the 5-year survival rates. The stage of colorectal cancer was determined according to the classification of cancer disease stage of the 7th American Joint Committee on Cancer (AJCC) [15]. Postoperative complications and mortality were examined in a limited way during the hospital stay at the time of surgery only.
For all statistical analyses, the SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used. For the comparison of variables, the unpaired t-test and the Žć2-test were used. Survival rates were calculated by using the Kaplan-Meier method and the results were validated by using the log-rank test. A P-value less than 0.05 was considered to be statistically significant.
The average age of the 266 patients was 63.8 ┬▒ 12.1 years, the mean age of the 212 patients who underwent a standard procedure was 63.7 ┬▒ 12.4 years, and the mean age of the 54 patients who underwent a multivisceral resection was 64.4 ┬▒ 11.9 years. The ratio of males to females was 1:0.97, the ratio for the group that underwent a standard resection being 1:0.98 and that for the group that underwent a multivisceral resection being 1:0.93. The gender ratios were not significantly different (Table 1).
As the site at which the primary tumor developed, the rectum was most prevalent, followed in order by the right large intestine, the sigmoid colon, the left large intestine, and the transverse colon. The average tumor size of the group that underwent a standard procedure was 5.6 ┬▒ 1.1 cm, and that of the group that underwent a multivisceral resection was 6.2 ┬▒ 1.3 cm.
Among the 54 patients of the group that underwent a multivisceral resection, in 28 pT3 (52%) cases, neighboring organ invasion was suspected macroscopically, so a multivisceral resection was performed. However, postoperative pathohistological findings showed only inflammatory adhesion to adjacent tissues without the penetration of cancer cells to the large intestine serosa; 26 pT4 (48%) cases did show actual cancer cell invasion.
Based on the AJCC disease classification, stage IIA disease was detected in 16 (29.6%) of the cases that underwent a multivisceral resection, stage IIB disease in 3 cases (5.6%), stage IIC disease in 10 cases (18.5%), stage IIIB disease in 7 cases (13%), and stage IIIC disease in 18 cases (33.3%). Stage IIIC disease was the most prevalent.
Regarding the histological morphology and differentiation of cells, an adenocarcinoma was found in 49 cases (90.7%), a mucinous carcinoma in 4 cases (7.4%), and a signet ring cell carcinoma in 1 case (1.9%). An adenocarcinoma was the most prevalent. Among adenocarcinomas, a moderately differentiated adenocarcinoma was found in 30 cases (55.5%), and it was the most prevalent.
In the 54 patients who underwent a multivisceral resection, in regard to the organs removed, the small intestine was removed in 13 cases (24%), which was the most prevalent, followed in order by the ovary and the bladder (Table 2). In cases showing actual cancer infiltration, the small intestine was most frequently resected in combination. In 45 cases, a multivisceral resection including one organ other than the primary lesion was performed, and in 11 cases, a multivisceral resection including more than two organs other than the primary lesion was performed.
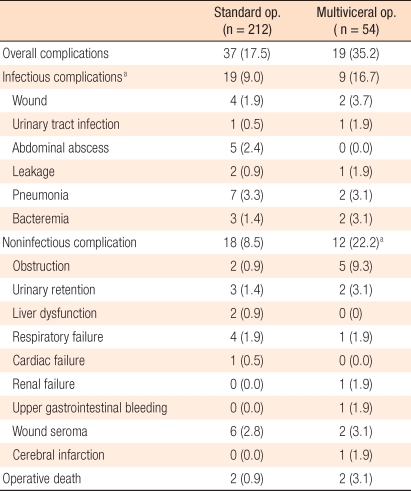
In cases that underwent a standard procedure, postoperative complications developed in 37 patients (17.5%), 40 events, and in cases that underwent a multivisceral resection, they developed in 19 patients (35.2%), 21 events (Table 3). When the complications were divided into infectious complications and non-infectious complications, a trend was that both infectious and non-infectious complications occurred approximately 2 times more frequently in the patient group that had undergone a multivisceral resection, and the difference was statistically significant (17.5% vs. 35.2%, P < 0.001). Two postoperative deaths occurred in each group. In the group that underwent a standard procedure, one patient died of postoperative pneumonia and the other died of the leakage at the anastomosis site. In the group that underwent a multivisceral resection, one patient died of respiratory failure due to severe pleural effusion caused by renal failure and the other died of sepsis caused by a peritoneal abscess that developed due to the rupture of the tumors during surgery.
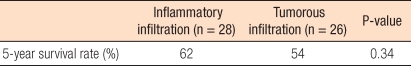
In the group that underwent a standard procedure, the 5-year survival rate of stage II patients was 68%, and that of stage III patients was 56%. In the group that underwent a multivisceral resection, the 5-year survival rate of stage II patients was 64%, and that of stage III patients was 52%. In both groups, as the disease stage advanced, survival rates decreased (Table 4). In addition, the 5-year survival rate of the group that underwent a standard procedure was 61%, and that of the group that underwent a multivisceral resection was 58%, but the difference in survival rates was statistically not significant. In the group that underwent a multivisceral resection, the 5-year survival rate for patients who developed adhesion caused by simple inflammatory reactions was 62%, and the 5-year survival rate of patients with adhesion caused by actual tumor infiltration was 54%, but no statistically significant difference was shown (Table 5).
A multivisceral resection is defined as a surgical method resecting organs or structures adhering to the primary cancer en-bloc [4]. It has been reported that in colorectal cancer patients, cases in which local tumor invasion to adjacent organs or structures is suspected and in which a multivisceral resection is, thus, performed account for 7-16% of all cases [4, 6, 7, 16]. In our cases, similarly, the ratio of patients undergoing a multivisceral resection was 54 of the 356 patients (15.2%) who underwent surgery for colorectal cancer, which is comparable to the ratios reported by other studies.
Whether the adhesion to adjacent organs was caused by direct invasion by the tumor or as a result of a simple inflammatory reaction could not be determined by using macroscopic examination only, but it could be determined based on pathohistological findings after surgery. Among cases with adhesion of tumors to adjacent organs, 50-85% have been reported to be caused by actual cancer cell infiltration [4, 8-10, 12, 16]. In our cases, 26 of 54 patients (48%) had adhesion due to direct tumor infiltration, and the remaining 28 (52%) had adhesion was caused by a simple inflammatory reaction. Thus, many studies have reported that in cases when operative findings show suspected tumor infiltration, a radical resection, an en-bloc resection including adjacent organs
and structures, achieved a good treatment outcome [3-14].
When invasion of tumors to adjacent organs is suspected, the separation of the adhered organs from the tumors has been reported to induce dissemination of tumor cells, thus elevating the local recurrence rate. When tumors rupture during surgery performed to separating the tumors from adjacent organs, the 5-year survival rate is merely 17%, but that of the en-bloc resection group is 49%, so a noticeably poorer treatment outcome was achieved in the former [4, 9].
Izbicki et al. [13] reported studies conducted on 220 T3 and T4 colorectal cancer patients thought to have local tumor infiltration; a multivisceral resection was performed in 83 cases. Among those 83 cases, in 38 cases, tumor infiltration was suspected macroscopically; however, after final pathologic tests, inflammatory adhesion, not cancer invasion, was found. They stated that the median survival times of the group that underwent a standard procedure and the group that underwent a multivisceral resection were 45 months and 44 months, respectively, and that no differences in postoperative morbidity or mortality of the two resection groups were detected. Hence, for cases in which tumor infiltration is suspected, an aggressive multivisceral resection is required. In our cases, if high-risk surgery to perform an en-bloc resection or a highly technically difficult operation, for example, cases with adhesion to the pancreas or intrapelvic organs was not performed, an aggressive multivisceral resection was performed.
Lehnert et al. [4] analyzed 201 patients that underwent a multivisceral resection because of invasion of tumors to adjacent organs. The location of the primary tumor was the sigmoid colon in 65 cases (32%), the rectum in 62 cases (31%), and the right large intestine in 34 cases (18%). In our cases, the rectum was the site in 57.4% of the cases, the right large intestine in 22.2%, and the sigmoid colon in 11.1%. The most prevalent organ was different from our study, but this is thought to be due to the fact that in upper rectal cancer cases, it is difficult to distinguish the organs from the sigmoid colon. However, the three organs where tumors developed most frequently were identical. Thus, for tumors that develop in the rectum, the incidence of invasion of malignant tumors to organs adjacent to the tumors has been shown to be high for tumors that develop in the right intestine and the sigmoid colon. Concerning adjacent organs to which tumors frequently adhere, Lehnert et al. [4] reported that in colorectal cancer cases, the organs were the large intestine and the bladder, and that in rectal cancer cases, they were, in order, the small intestine, the uterus, and the bladder. Gebhardt et al. [11] reported that the organs resected in combination were, in order, the small intestine, the bladder, and the female reproductive system. In our cases, the order was also the small intestine, the bladder, and the female reproductive system.
In the decision to use a multivisceral resection including adjacent organs, a fact that should be considered first is the increased morbidity and mortality after surgery. The incidence of complications after a multivisceral resection is reported to be from 11% to 44%, with an average of approximately 31% [4, 11-13, 17-19]. In regard to mortality, Gebhardt et al. [11] reported mortality in more than 3.6% of 173 patients. Cho et al. [3] reported that, among 36 patients, 1 patient died. In our cases, among 54 patients who underwent a multivisceral resection, 1 patient died. Among the 212 patients that underwent a standard procedure, 2 patients died.
Gebhardt et al. [11] reported that in colorectal cancer patients who underwent a multivisceral resection, the incidence of postoperative complications was 11.4%, and that of mortality was 3.6%, which were comparable to the rates of postoperative complications and mortality for our patient group that underwent a standard procedure (11.5% and 3.4%). Nakafusa et al. [19] investigated 323 pT3-pT4 colorectal cancer patients. A multivisceral resection was performed in 53 cases (16.4%), and among them, cancer infiltration was detected in 28 cases (52.8%). The incidences of postoperative complications in the group that underwent a standard procedure and the group that underwent a multivisceral resection were 17.8% and 49.1%, respectively, and the incidences of infectious complications (11.1% vs. 32.1%) and the incidences of noninfectious complications (8.9% vs. 20.8%) were higher in the group that underwent a multivisceral resection. Lepape et al. [14] reported that in 41 colorectal cancer patients who underwent a multivisceral resection, the incidences of postoperative complications and mortality weres 30.9% and 12.5%, respectively. In our study, in cases that underwent a multivisceral resection, 19 developed postoperative complications (35.2%), and 2 died (3.7%), results comparable to other studies.
Gebhardt et al. [11] reported that the effectiveness of a multivisceral resection is reflected in the survival rate. In the group that underwent a standard procedure and the group that underwent a multivisceral resection, the 5-year survival rates were examined for each stage, and the observed 5-year survival rates were as follows: stage II, 60% vs. 58%; stage III, 41% vs. 43%. Thus, for the same stage, no significant differences between the two surgery groups were shown. In addition, in the multivisceral resection group, the 5-year survival rates of pT3 patients with adhesion due to a simple inflammatory reaction and of pT4 patients with adhesion due to actual cancer infiltration weres 64% and 44%, respectively, which was comparable to our study. In the results reported by Lehnert et al. [4] the 5-year survival rates of stage II patients in the group that underwent a standard procedure and in the group that underwent a multivisceral resection were 66% and 63%, respectively, and those of stage III patients were 45% and 38%. In a recent study conducted on a large number of patients, the 5-year survival rate after a multivisceral resection was been reported to be approximately 51% [4, 10, 11], which is similar to the result in our study. However, in the study reported by Nakafusa et al. [19], the 5-year survival rates of the group that underwent a standard procedure and of the group that underwent a multivisceral resection were 79.5% and 76.6%, respectively, which are different from our study. This is thought to be due to the difference in the selection of patients, which excluded emergency surgery patients, the difference of stage at the time of surgery, etc.
In several studies, the effectiveness of a multivisceral resection has also been reported to be reflected in the rate of local recurrence and the disease-free survival rate. Croner et al. [20] reported that in 174 multivisceral resection patients, en-bloc resection of cancer could be performed in 162 patients (93.1%), that the local recurrence rate after surgery was 6.5%, and that the presence or absence of lymph node metastasis and the dissemination of cancer cells during surgery were major factors exerting effects. Nakafusa et al. [19] reported that the 5-year disease-free survival rate after surgery for the group that underwent a standard procedure (72.9%) was not greatly different from that of the group that underwent a multivisceral resection (66.8%). When prognostic factors were analyzed by using a multivariate analysis, tumor size, level of infiltration, volume of blood loss during surgery, operation time, and whether or not transfusion had been performed were found to be major prognostic factors. In our study, the number of subjects was small, and the follow-up observation period was short, so it was difficult to perform the follow-up observation. Thus, a multivariate analysis for the local recurrence rate and the disease-free survival rate could not be performed. However, in locally advanced colorectal cancer cases, 48% involved actual cancer infiltration, complications, although mild in most cases, were increased after a multivisceral resection, and the 5-year survival rate was not significantly different from that for a standard procedure. Thus, good outcomes may be obtained by performing a multivisceral resection aggressively.
For the treatment of locally advanced colorectal cancer that has invaded adjacent organs, radical surgery using a multivisceral resection has the disadvantage of increased postoperative complications, but the 5-year survival rate is comparable to that for the standard procedure. Therefore, except for patients with high risk, an aggressive multivisceral resection may increase the possibility of long-term survival after surgery.
References
1. Ministry for Health, Welfare and Family Affarirs. Annual report of cancer incidence (2007), cancer prevalence (2007), and survival (1993-2007) in Korea. 2009.Seoul: Ministry for Health, Welfare and Family Affairs.
2. Lee CR, Kim YW, Kim NK, Hur H, Min BS, Lee KY, et al. The influence of age on survival and recurrence after a curative surgical resection for colon cancer patients. J Korean Soc Coloproctol 2009;25:401ŌĆō409.

3. Cho SW, Lee RA, Chung SS, Kim KH. Concomitant adjacent organ resection in locally advanced colon cancer. J Korean Soc Coloproctol 2009;25:94ŌĆō99.

4. Lehnert T, Methner M, Pollok A, Schaible A, Hinz U, Herfarth C. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg 2002;235:217ŌĆō225. PMID: 11807361.



5. Nelson H, Petrelli N, Carlin A, Couture J, Fleshman J, Guillem J, et al. Guidelines 2000 for colon and rectal cancer surgery. J Natl Cancer Inst 2001;93:583ŌĆō596. PMID: 11309435.


6. Staniunas RJ, Schoetz DJ Jr. Extended resection for carcinoma of colon and rectum. Surg Clin North Am 1993;73:117ŌĆō129. PMID: 8426992.


7. Sugarbaker PH, Corlew S. Influence of surgical techniques on survival in patients with colorectal cancer. Dis Colon Rectum 1982;25:545ŌĆō557. PMID: 6749455.


8. Eisenberg SB, Kraybill WG, Lopez MJ. Long-term results of surgical resection of locally advanced colorectal carcinoma. Surgery 1990;108:779ŌĆō785. PMID: 2218891.

9. Gall FP, Tonak J, Altendorf A. Multivisceral resections in colorectal cancer. Dis Colon Rectum 1987;30:337ŌĆō341. PMID: 3568922.


10. Heslov SF, Frost DB. Extended resection for primary colorectal carcinoma involving adjacent organs or structures. Cancer 1988;62:1637ŌĆō1640. PMID: 3167778.


11. Gebhardt C, Meyer W, Ruckriegel S, Meier U. Multivisceral resection of advanced colorectal carcinoma. Langenbecks Arch Surg 1999;384:194ŌĆō199. PMID: 10328174.


12. Sokmen S, Terzi C, Unek T, Alanyali H, Fuzun M. Multivisceral resections for primary advanced rectal cancer. Int J Colorectal Dis 1999;14:282ŌĆō285. PMID: 10663895.


13. Izbicki JR, Hosch SB, Knoefel WT, Passlick B, Bloechle C, Broelsch CE. Extended resections are beneficial for patients with locally advanced colorectal cancer. Dis Colon Rectum 1995;38:1251ŌĆō1256. PMID: 7497835.


14. Lepape A. Prevention of nosocomial infections in ICU. What is really effective? Med Arh 2003;57(4 Suppl 1): 15ŌĆō18. PMID: 15017857.
15. In: Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. editors. AJCC cancer staging manual. 2009.7th ed. New York: Springer.
16. Kruschewski M, Pohlen U, Hotz HG, Ritz JP, Kroesen AJ, Buhr HJ. Results of multivisceral resection of primary colorectal cancer. Zentralbl Chir 2006;131:217ŌĆō222. PMID: 16739062.



17. Luna-Perez P, Rodriguez-Ramirez SE, De la Barrera MG, Zeferino M, Labastida S. Multivisceral resection for colon cancer. J Surg Oncol 2002;80:100ŌĆō104. PMID: 12173378.


18. Eisenberg SB, Kraybill WG, Lopez MJ. Long-term results of surgical resection of locally advanced colorectal carcinoma. Surgery 1990;108:779ŌĆō785. PMID: 2218891.

19. Nakafusa Y, Tanaka T, Tanaka M, Kitajima Y, Sato S, Miyazaki K. Comparison of multivisceral resection and standard operation for locally advanced colorectal cancer: analysis of prognostic factors for short-term and long-term outcome. Dis Colon Rectum 2004;47:2055ŌĆō2063. PMID: 15657654.


20. Croner RS, Merkel S, Papadopoulos T, Schellerer V, Hohenberger W, Goehl J. Multivisceral resection for colon carcinoma. Dis Colon Rectum 2009;52:1381ŌĆō1386. PMID: 19617748.


- TOOLS
-
METRICS

- Related articles in ACP
-
Advances in surgery for locally advanced rectal cancer2022 August;38(4)