- Search
|
|
Abstract
Purpose
The management of a colonoscopic perforation (CP) varies from conservative to surgical. The objective of this study was to evaluate the outcomes between surgical and conservative treatment of patients with a CP.
Methods
From 2003 to 2016, the medical records of patients with CP were retrospectively reviewed. Patients were divided into 2 groups depending on whether they initially received conservative or surgical treatment.
Results
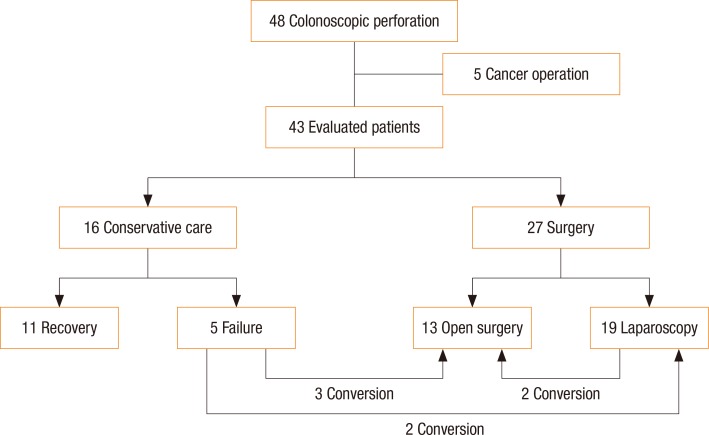
During the study period, a total of 48 patients with a CP were treated. Among them, 5 patients had underlying colorectal cancer and underwent emergency radical cancer surgery; these patients were excluded. The mean age of the remaining 43 patients was 64.5 years old, and the most common perforation site was the sigmoid colon (15 patients). The initial conservative care group included 16 patients, and the surgery group included 27 patients. In the conservative group, 5 patients required conversion to surgery (failure rate: 5 of 16 [31.3%]). Of the surgery group, laparoscopic surgery was performed on 19 patients and open surgery on 8 patients, including 2 conversion cases. Major postoperative complications developed in 11 patients (34.4%), and postoperative mortality developed in 4 patients (12.5%). The only predictor for poor prognosis after surgery was a high American Society of Anesthesiologists physical status classification.
Colonoscopy is the most useful examination in the diagnosis and treatment of colorectal diseases. With the recent increase in the prevalence of these diseases, this examination is being conducted more and more frequently to diagnose patients suspected of having lesions. In addition to the diagnosis for lesions, colonoscopy can even be applied to treatments such as biopsies, polypectomies, electrocautery, and endoscopic submucosal dissections. Currently, it is widely used for various purposes. Even though colonoscopy is relatively safe, its use may cause a variety of complications, such as hemorrhage or perforation. In terms of hemorrhage, the treatments are relatively clear. Generally, hemorrhage can be treated with electrocautery. In rare cases, surgical treatments are required. However, colonoscopic perforation (CP) is a serious complication that may cause death and occurs during a colonoscopic procedure at a rate of 0.01% to 0.3% [1,2,3,4,5].
Controversy surrounds the treatments for patients with a CP. Patients diagnosed with prominent peritonitis after physical examination should be immediately treated surgically. Otherwise, conservative treatment can be conducted. However, concerns arise with the use of conservative treatment because compared to early surgical treatments, more complications are likely to arise when this treatment fails [2,6]. In this context, the present study explored risk factors and complications based on the outcomes of surgical and conservative treatments of patients with a CP.
This study was retrospectively conducted for patients treated for a CP from January 2003 to August 2016 at the Department of Surgery, Chosun University Hospital, by using their medical records containing various clinical characteristics. Informed consents were not required based on the approval of the Institutional Review Board of Chosun University Hospital (approval number: 2017-09-020-003), after which the study began. We recruited a total of 48 patients treated for a CP. Among them, 5 patients with colon and rectal cancers, as well as a CP, were excluded. Finally, 43 patients were eligible for this study.
If a CP was suspected, we checked for the presence of free air in the abdominal cavity as determined by using simple x-ray scans, or we checked for information such as the presence and location of free air as determined by using computed tomography (CT) in cases of diagnostic difficulty. Patients who manifested prominent symptoms of generalized peritonitis, such as fever, the absence of bowel sounds, generalized abdominal tenderness, and rigidity, received early surgical treatment based on the judgment of the surgeons. On the other hand, conservative treatment was performed in relatively stable patients, despite their having been diagnosed with CP.
For conservative treatments, we performed empiric broad spectrum antibiotic administration (combined administration of second-generation cephalosporin and metronidazole), nil per os, and intravenous fluid therapy. After the symptoms of peritonitis had improved, bowel sounds had returned, and white blood cell count had normalized, the patients were started on a dietary regime. Antibiotics, including oral antibiotics, were administered until their symptoms improved. If worsening symptoms were observed in the conservative treatment group after treatment or if their symptoms did not improve within 2 to 3 days, we regarded conservative treatment to be a failure and converted it to surgical treatment.
Statistical data were analyzed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA). Univariate and multivariate analyses were conducted using the chi-square test and a multiple logistic regression analysis, respectively. Statistical significance was set at P values less than 0.05 for all analyses.
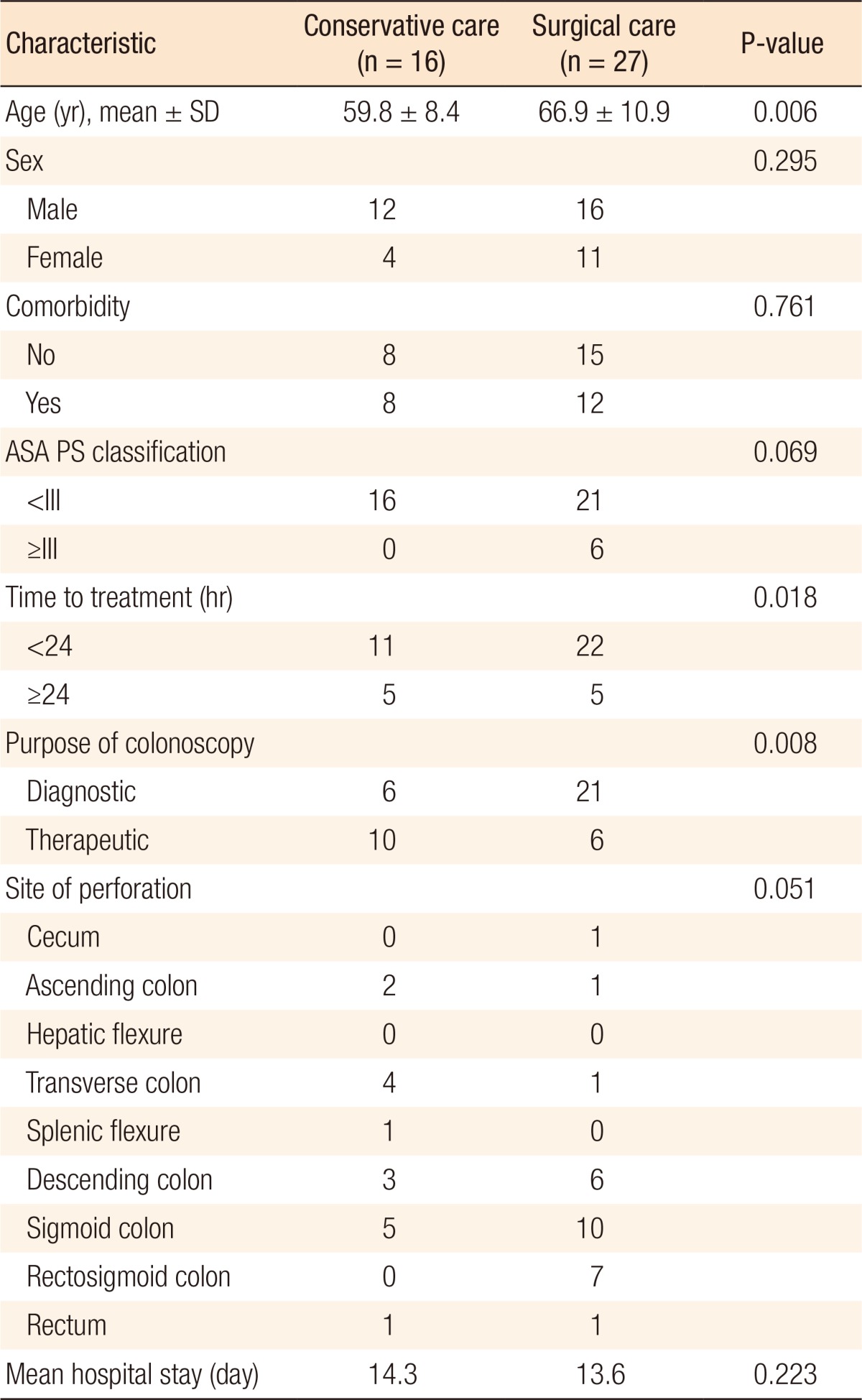
The characteristics of the patients and the outcomes of their treatment are shown in Table 1. The average patient age was 64.5 years of age. Patients in the conservative and the surgical treatment groups were aged 59.8 and 66.9 years on average, respectively. A significant difference in age was noted between the groups, with the patients in the conservative group being younger. The numbers of male and female patients were 12 and 4 persons in the conservative treatment group and 16 and 11 persons in the surgical treatment group, respectively. In terms of early treatment, 22 among 33 patients treated within 24 hours after the diagnosis of a CP received surgical treatment whereas 5 among 10 patients treated 24 hours or longer after the diagnosis received surgical treatment. A significant difference between the groups was the observation that operative treatment was used more frequently in cases of early diagnosis. The numbers of patients with CP undergoing diagnostic and therapeutic colonoscopy were 27 and 16 persons, respectively. Surgical treatment was conducted as early treatment in 77.8% of the patients in the diagnostic CP group and in 37.5% of the patients in the therapeutic CP group. A significant difference in relation to treatment choice was found between the groups. CPs occurred in the sigmoid colon (15 cases), followed by the descending colon and the rectosigmoid colon. The lengths of hospital stay were 14.3 and 13.6 days in the conservative and the surgical treatment groups, respectively.
Fig. 1 shows the distributions of patients according to the type of treatment. Conservative treatment was effective in 11 of 16 patients who received it as an early treatment. However, the other five did not improve and underwent surgical treatment. The treatment failure rate was 31.3%. The analysis for risk factors associated with the failure of conservative treatment showed no statistically significant risk factors (data not shown). Surgical treatment was performed in 27 patients by using a laparotomy or colonoscopy. Laparoscopy was done in 19 patients of the surgical treatment group, and 2 cases were converted to a laparotomy. A laparotomy was finally performed in a total of 13 patients, including 3 patients for whom conservative treatment had failed and 2 patients for whom colonoscopy was converted to a laparotomy.
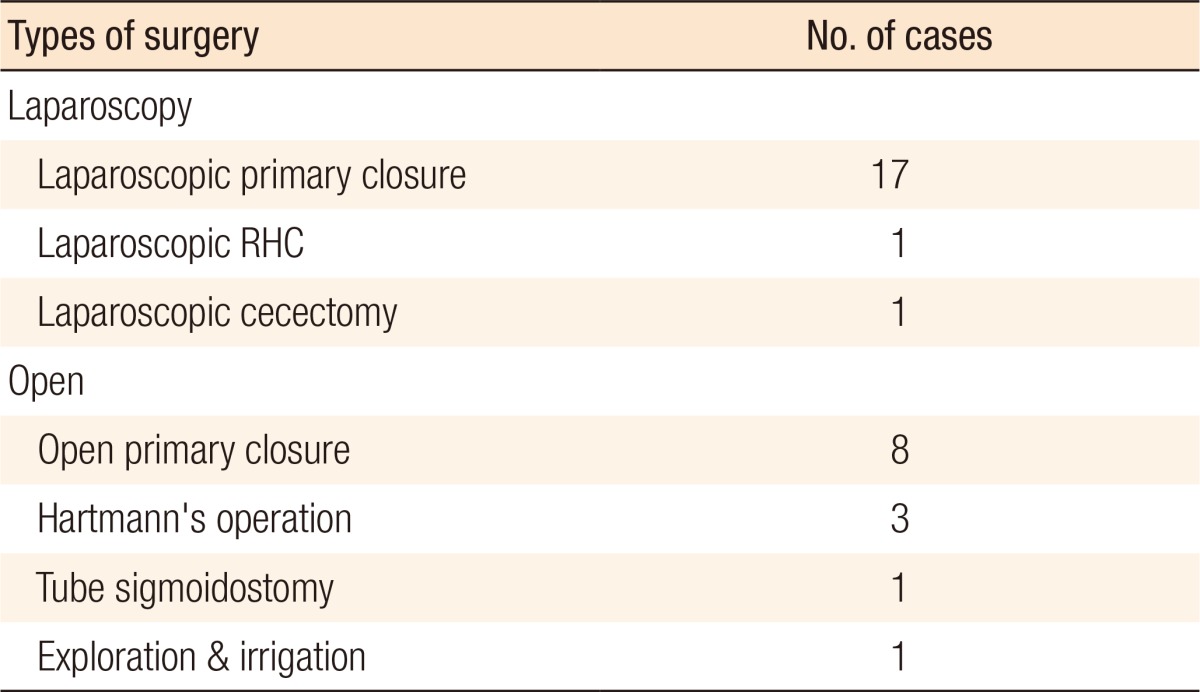
With regard to types of surgery, a laparoscopic primary closure (17 patients) was most frequently conducted, followed by open primary repair (8 patients) and Hartmann's operation (3 patients). If patients were diagnosed with a colorectal carcinoma as an underlying disease, they were treated with a radical resection. In addition, in one patient, the perforated sites had already been closed, so only a simple lavage was performed (Table 2).
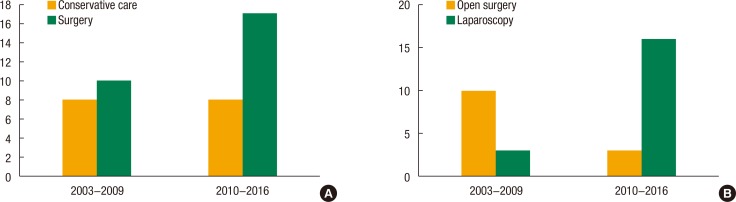
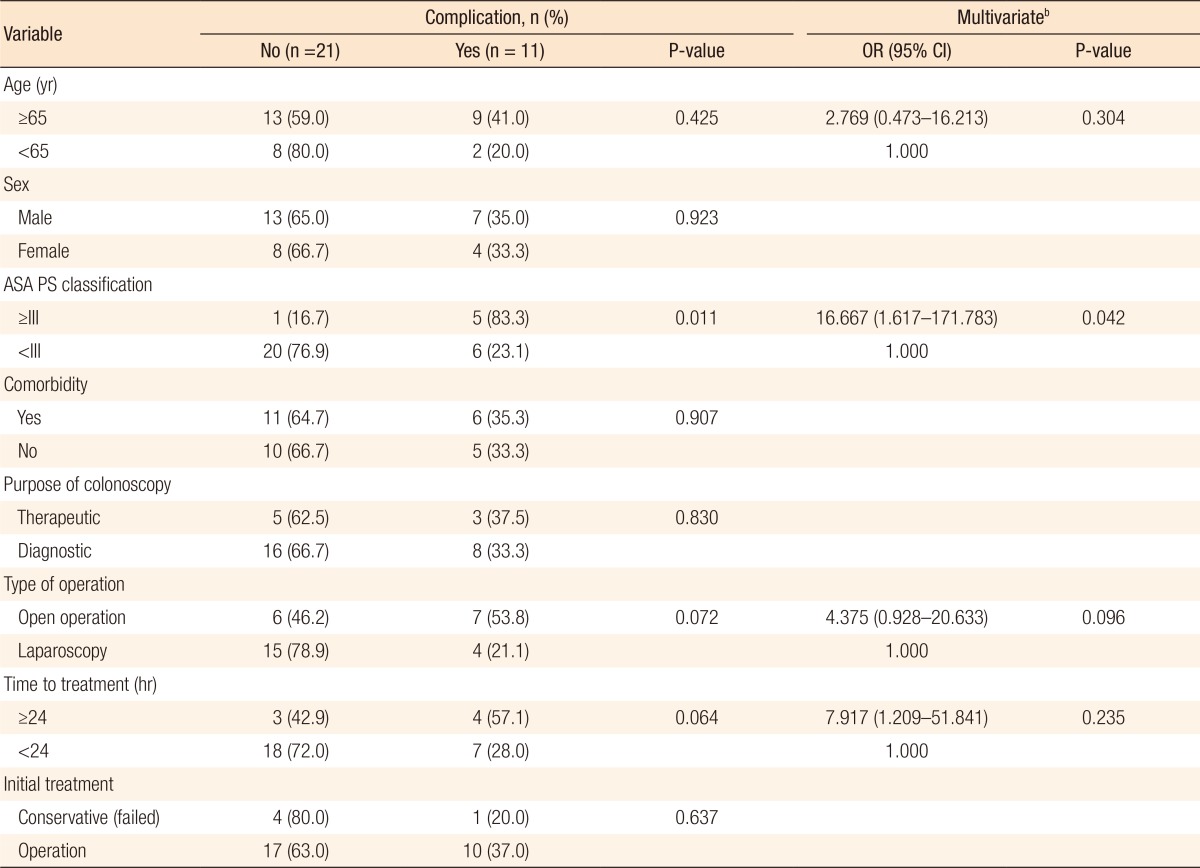
In our institution, since 2010, laparoscopic surgery has been actively conducted as a basic surgical tool for the treatment of patients with colorectal disease. Accordingly, we divided the study period into a first and a second half based on the years during which the treatment had been given, and we investigated the change in treatment methods. We found that, compared to the first half, surgical treatment was more common in the second half. Moreover, laparoscopic surgery was more frequently performed in the second half (Fig. 2).
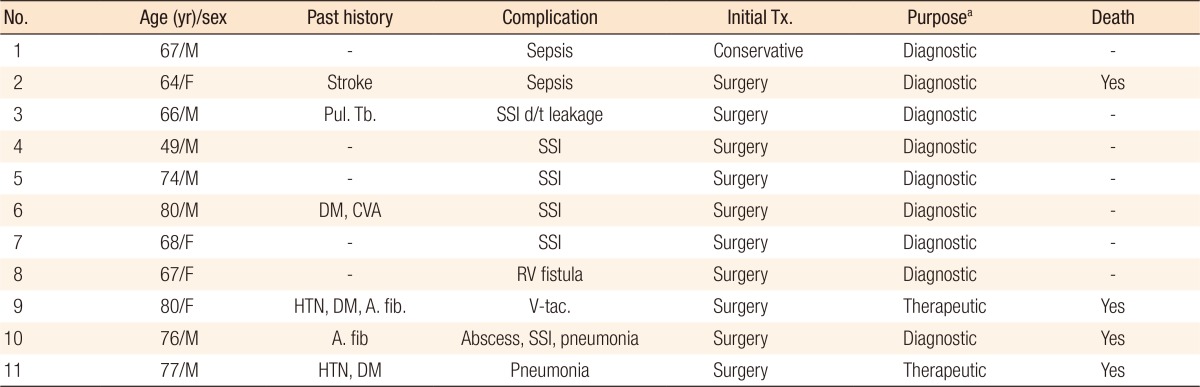
The clinical details for complications after surgery are shown in Table 3. High grade complications of more than grade III based on the Clavien-Dindo classification occurred in 11 of the 32 patients (34.4%) who received surgical treatment, including 27 patients who received surgical treatment in an early period and 5 patients who were converted to surgical treatment after the failure of conservative treatment. Surgical site infection (SSI) was the most common complication, followed by ileus and intra-abdominal abscess. The causes of treatment failure at the perforation site included leakage at suture sites (1 case) and a rectovaginal fistula (1 case). A total of 4 patients died. They were elderly patients aged 70 years or older or had underlying medical histories, such as hypertension, diabetes, cardiovascular diseases, and cerebral stroke. The causes of death included persistent sepsis (1 case), ventricular fibrillation (1 case), and pneumonia (2 cases).
The results of the risk factor analysis for poor prognosis in the surgery group are presented in Table 4. The 32 patients treated with surgery, including 5 patients for whom conservative treatment had failed, were divided into those with major complications or mortality (poor prognosis) and those with no complications. We analyzed clinical variables. No significant relationships were found between poor prognosis and the following variables related to CP: its mechanism, treatment time, and surgical methods. The American Society of Anesthesiologists (ASA) physical status classification was found to be the sole significant risk factor associated with poor prognosis in both the univariate and the multivariate analyses (odds ratio, 16.667; P = 0.042).
This study classified CP patients into conservative and surgical treatment groups and analyzed their treatment outcomes. Five out of the 16 patients who underwent conservative treatment were converted to surgical treatment; thus, the treatment failure rate was 31.3%. Similarly, the incidence of major complications was relatively high (34.4%) in the surgical treatment group.
Reports in the 1990s indicated that the incidence of colorectal perforation was 0.1% to 3%. According to other reports published since the 2000s, the incidence has decreased and is 0.01% to 0.3%. However, with the recent increased frequency of colonoscopy, CPs no longer occur infrequently [2,3,4,5]. Once a CP occurs, it is not easy to treat and can lead to complications or death in certain patients. Accordingly, emphasis should be placed on prevention. A therapeutic colonoscopy may cause a CP during a polypectomy, and proper treatment would be required. Kim et al. [7] showed that a common site for a CP was the sigmoid colon. Similarly, this study revealed that a CP predominantly occurred in the sigmoid colon (34.9%). Thus, colonoscopist should be very careful in the rectum and the sigmoid colon during insertion of the colonoscope. If a patient has an obstructive lesion, the doctor, for safety, should consider other alternative examinations rather than the laborious colonoscope insertion.
We can roughly consider conservative and surgical approaches to the treatment of patients with a CP. However, debate exists over which treatment should be selected. When surgical treatment is delayed, the operation may be difficult, and sometimes a staged operation may be necessary. Furthermore, such delays may cause serious complications or death. For these reasons, some argue for performing surgery immediately after diagnosis [6,7,8,9]. Contrary to this, some argue that because of the colonic preparation before a colonoscopy, the abdominal cavity is less contaminated in spite of the perforation, so conservative treatment may be sufficiently effective [2,10]. Surgical treatment includes simple sutures, a partial colectomy, and a colostomy and is determined depending on the perforation's size as identified in the operating room, the degree of inflammation around the perforated sites, and the degree of abdominal cavity contamination. In the past, an open laparotomy approach was often conducted as a surgical treatment for CP patients. Currently, the laparoscopic approach has high priority in terms of early recovery and cosmetics. The results of this study indicate that a laparotomy is more likely to cause complications, such as SSIs. Because laparoscopic surgery was actively introduced in the second half of the study period and was employed in most operations, the frequency SSIs tended to decrease.
Generally, conservative treatment can be conducted if the patient has a small perforation, is in good general condition, and shows only mild signs of peritonitis. Such treatment requires the rapid administration of broad spectrum antibiotics and intravenous fluid therapy. With such treatment, clinical symptoms have been reported to improve usually within 24 hours [10,11,12]. In the case of surgery due to the failure of conservative treatment, the current thinking is that patients will have to undergo extensive and very difficult surgery, and some may die. For patients undergoing conservative treatment, the surgeon should carefully monitor their conditions and consider surgical treatment if they show no improvement during or after conservative treatment. In this study, 5 of the patients who received conservative treatment were converted to surgery. Four among those 5 were converted within 2 to 4 days. With regard to types of surgery, a laparotomy was performed in 3 cases, laparoscopic surgery in 2 cases, and primary closure without colostomy in 4 cases. Importantly, in 1 case, the perforation recurred 1 month after successful conservative treatment, and surgical treatment was conducted. Thus, sufficient follow-up is required for patients who undergo conservative treatment due to the possibility of a recurrent perforation.
With regard to surgical treatment, primary closure was most commonly performed, followed by a right hemicolectomy, anterior resection, and Hartmann operation. In particular, with the accumulation of experience with CP treatment, mainly the laparoscopic approach has been conducted since 2010. Kim et al. [7] reported that the incidence of major complications increased at times longer than 24 hours after perforation. On the other hand, this study showed that primary closure had an excellent effect even at 2 days after perforation. Accordingly, we should decide on the surgical method by considering collectively the patient conditions, the perforation's size, the degree of colonic preparation, and underlying diseases, not simply by elapsed time after perforation [13].
An et al. [14] reported that the factors related to poor outcomes of CP treatment included old age (60 years or older), ASA physical status classification of grade III or more, and conversion to surgical treatment because of the failure of conservative treatment and that conservative treatment was more likely to fail for perforations with sizes of 15 mm or more. Iqbal et al. [15] reported that the incidence of complications after surgical treatment for CP was 36% in 165 patients and that the risk factors for complications included blunt injury, poor colonic preparation, corticosteroid use, and young age (less than 67 years). Another study showed that the incidences of complications and deaths after surgical treatment for CP were 48.7% and 25.6%, respectively, and that an ASA physical status classification grade III or more and antiplatelet drug use were associated with high mortality [16]. The present study indicated that risk factors related to poor prognosis included neither the cause of the perforation, the treatment method, nor the treatment time. Only the ASA physical status classification was found to be an independent significant risk factor for a poor prognosis.
Another study revealed that early diagnosis was important in treating patients with a CP and that endoscopic clipping as a conservative treatment showed good effects. However, endoscopic treatment should be performed just after the diagnosis of a perforation. If the perforation size is large, this treatment may be impossible, and the procedure indication may not be clear. In this regard, we should pay attention to CP treatment [17]. In cases of a delayed diagnosis after a CP, generally, treatment methods are determined with difficulty, and treatment outcomes may be poor. Thus, in such cases, surgical treatment is commonly recommended. Specifically, laparoscopic surgery is recommended more often than a laparotomy [18,19,20]. A study showed that a delay in the diagnosis of a CP of 24 hours or more is associated with complications and mortality [21]. However, our study revealed that delayed treatment for a CP was not a risk factor for poor prognosis, even after conversion to surgical treatment due to the failure of conservative treatment. Similarly, other studies revealed that a delayed diagnosis and treatment for CP did not increase complications and mortality. Accordingly, treatment outcomes after surgical treatment for CP vary widely. The risk factors for CP are also very different and vary from study to study. These results may be due to the fact that most studies were conducted in a single institution and/or involved small numbers of subjects. Therefore, if accurate analyses of treatment outcomes and prognostic factors are to be done, further studies involving multiple institutions and targeting more patients are needed.
This study has the following limitations: Endoscopic clipping, which is now commonly conducted as a conservative treatment for patients with a CP, was not included in this study, and this study was conducted at a single institution by using a retrospective analysis. Furthermore, for the analysis of the prognosis after surgery, a multivariate analysis was difficult to do because of the small numbers of subjects. Finally, the surgical treatment group was somewhat heterogeneous because patients who finally converted to surgical treatment due to the failure of conservative treatment were added to those who underwent surgery as an early treatment, leading to an increased risk of statistical deviations.
In conclusion, in terms of the treatment of patients with a CP, conservative treatment may be appropriate for stable patients, but the high risk of treatment failure should be considered. Surgically-treated patients in poor general condition should receive close attention to reduce the risk of major complications and mortality.
References
1. Na EJ, Kim KJ, Min YD. Safety of conservative treatment of colonoscopic perforation. J Korean Soc Coloproctol 2005;21:384ŌĆō389.
2. Ker TS, Wasserberg N, Beart RW Jr. Colonoscopic perforation and bleeding of the colon can be treated safely without surgery. Am Surg 2004;70:922ŌĆō924. PMID: 15529852.



3. Namgung H, Cho MK, Lee KH, Myung SJ, Yang SK, Yu CS, et al. Management of colonic perforation during colonoscopic procedure. Korean J Gastrointest Endosc 2005;30:188ŌĆō193.
4. Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol 2000;95:3418ŌĆō3422. PMID: 11151871.


5. Park HR, Baek SK, Bae OS, Park SD. Treatment of colon perforation associated with colonoscopy. J Korean Soc Coloproctol 2008;24:322ŌĆō328.

6. Gedebou TM, Wong RA, Rappaport WD, Jaffe P, Kahsai D, Hunter GC. Clinical presentation and management of iatrogenic colon perforations. Am J Surg 1996;172:454ŌĆō457. PMID: 8942543.


7. Kim HH, Kye BH, Kim HJ, Cho HM. Prompt management is most important for colonic perforation after colonoscopy. Ann Coloproctol 2014;30:228ŌĆō231. PMID: 25360430.



8. Farley DR, Bannon MP, Zietlow SP, Pemberton JH, Ilstrup DM, Larson DR. Management of colonoscopic perforations. Mayo Clin Proc 1997;72:729ŌĆō733. PMID: 9276600.


9. Cobb WS, Heniford BT, Sigmon LB, Hasan R, Simms C, Kercher KW, et al. Colonoscopic perforations: incidence, management, and outcomes. Am Surg 2004;70:750ŌĆō757. PMID: 15481289.



10. Christie JP, Marrazzo J 3rd. ŌĆ£Mini-perforationŌĆØ of the colon--not all postpolypectomy perforations require laparotomy. Dis Colon Rectum 1991;34:132ŌĆō135. PMID: 1993410.


11. Hall C, Dorricott NJ, Donovan IA, Neoptolemos JP. Colon perforation during colonoscopy: surgical versus conservative management. Br J Surg 1991;78:542ŌĆō544. PMID: 2059801.


12. Lo AY, Beaton HL. Selective management of colonoscopic perforations. J Am Coll Surg 1994;179:333ŌĆō337. PMID: 8069431.

13. Ko CW, Dominitz JA. Complications of colonoscopy: magnitude and management. Gastrointest Endosc Clin N Am 2010;20:659ŌĆō671. PMID: 20889070.


14. An SB, Shin DW, Kim JY, Park SG, Lee BH, Kim JW. Decision-making in the management of colonoscopic perforation: a multicentre retrospective study. Surg Endosc 2016;30:2914ŌĆō2921. PMID: 26487233.



15. Iqbal CW, Cullinane DC, Schiller HJ, Sawyer MD, Zietlow SP, Farley DR. Surgical management and outcomes of 165 colonoscopic perforations from a single institution. Arch Surg 2008;143:701ŌĆō706. PMID: 18645114.


16. Teoh AY, Poon CM, Lee JF, Leong HT, Ng SS, Sung JJ, et al. Outcomes and predictors of mortality and stoma formation in surgical management of colonoscopic perforations: a multicenter review. Arch Surg 2009;144:9ŌĆō13. PMID: 19153318.


17. Cho SB, Lee WS, Joo YE, Kim HR, Park SW, Park CH, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc 2012;26:473ŌĆō479. PMID: 21938583.


18. Shin DK, Shin SY, Park CY, Jin SM, Cho YH, Kim WH, et al. Optimal methods for the management of iatrogenic colonoscopic perforation. Clin Endosc 2016;49:282ŌĆō288. PMID: 26888410.




19. Park JY, Choi PW, Jung SM, Kim NH. The outcomes of management for colonoscopic perforation: a 12-year experience at a single institute. Ann Coloproctol 2016;32:175ŌĆō183. PMID: 27847788.



20. Hawkins AT, Sharp KW, Ford MM, Muldoon RL, Hopkins MB, Geiger TM. Management of colonoscopic perforations: A systematic review. Am J Surg 2017;8 26 [Epub]. pii:S0002-9610(17)30446-4PMID: 10.1016/j.amjsurg.2017.08.012..

21. La Torre M, Velluti F, Giuliani G, Di Giulio E, Ziparo V, La Torre F. Promptness of diagnosis is the main prognostic factor after colonoscopic perforation. Colorectal Dis 2012;14:e23ŌĆōe26. PMID: 21831176.


Fig.┬Ā2
Histograms by year for the types of management and the types of surgery. (A) Total patients were divided into conservative care and surgery. (B) The surgically treated groups were divided into open surgery and laparoscopy.