- Search
|
|
See commentary "The Impact of PatientŌĆÖs Pain and Fatigue on the Discharge Decision After Laparoscopic Surgery for Colorectal Cancer" in Volume 35 on page 158.
Abstract
Purpose
Hospital stays after laparoscopic surgery for colorectal cancer tend to be much shorter than those after conventional open surgery. Many factors, including surgical outcomes and complications, are associated with patient discharge planning. However, few studies have analyzed the impact of patient subjective discomfort (including pain and fatigue) on the decision to discharge after surgery. Therefore, the purpose of this study was to determine how patient pain and fatigue play a role in the decision to discharge after laparoscopic surgery for colorectal cancer.
Methods
Between March 2014 and February 2015, we conducted a questionnaire survey of 91 patients who underwent laparoscopic surgery for colorectal cancer to estimate the expectation criteria for discharge and patient subjective discomfort at that time. Patients were divided into the following 2 groups: group A, those who complied with the medical professionalŌĆÖs decision to discharge; and group B, those who refused discharge despite the medical professionalŌĆÖs decision. The participantsŌĆÖ subjective factors were analyzed.
Results
Preoperatively, 78 of 91 patients (85.7%) identified activity level, amount of food (tolerance), and bowel movements as important factors that should be considered in the decision to discharge a patient postoperatively. Postoperatively, 17 patients (18.7%) refused discharge despite a discharge recommendation. Subjective pain and fatigue were significantly different in linear-by-linear association between the group of patients who agreed to be discharge and those who disagreed. Despite this difference, there was no significant difference in mean length of hospital stay between the 2 groups.
Many randomized controlled trials have demonstrated that laparoscopic colorectal surgery produces better short-term outcomes, including less postoperative pain, faster recovery, shorter hospital stays, and earlier return to social activity, than does conventional open surgery [1-5]. In recent years, in addition to minimally invasive surgery, many efforts have been made to achieve faster recovery and return to society through organized postoperative management programs such as clinical pathway (CP) and enhanced recovery after surgery (ERAS) [6]. CP and ERAS are treatment programs that seek to improve prognosis through treatment standardization that is centered on evidence, while reducing the difference between baseline and actual clinical treatment [7]. Practically, CP or ERAS can decrease the length of hospital stay and overall medical expense through early postoperative oral ingestion, decreased postoperative stress and inflammatory responses, increased recovery rates, and decreased complications [8]. However, if a patientŌĆÖs compliance with this program is low, the expected effect may not be obtained. Many factors influence compliance with this postoperative care program, but surgical factors are the most significant [9-11]. Other factors, including patient education, counseling, and socioeconomic status, which have not been studied extensively, may also affect compliance [12, 13]. In addition to these objective factors, patient subjective symptoms may be related to compliance and decisions regarding discharge.
The purpose of this study was to estimate patientsŌĆÖ expectation criteria for discharge after laparoscopic surgery for colorectal cancer. We used a questionnaire to investigate the subjective factors that might affect patient satisfaction and decisions regarding discharge postoperatively.
Between March 2014 and February 2015, written informed consent was obtained from all participating patients who underwent laparoscopic colorectal cancer surgery at Incheon St. MaryŌĆÖs Hospital. This study was approved by Institutional Review Board (IRB) of Incheon St. MaryŌĆÖs Hospital (OC14QISI0007).
After consent was obtained, a 3-part questionnaire was completed by these patients. Part 1 of the questionnaire addressed patient demographics of sex, age, educational level, marital status, presence of a cohabitant, religion, occupation, income level, house structure, existence of private insurance, and presence of caregiver after discharge. Part 2 addressed patientsŌĆÖ expectation criteria for discharge, as follows: amount of food, number of bowel movements until discharge, degree of pain, degree of activity, and self-efficiency. Part 3 focused on the degree of subjective discomfort at the time of discharge, as follows: amounts of food, nausea, or vomiting; discomfort due to changes in bowel habits; pain; effects on activities of daily living; degree of gait; need for caregiver; and fatigue. The patients were asked to complete parts 1 and 2 of the questionnaire preoperatively, while part 3 was administered after the decision regarding discharge. Patient satisfaction and discomfort were assessed using a Likert scale of strongly disagree, disagree, neutral, agree, or strongly agree.
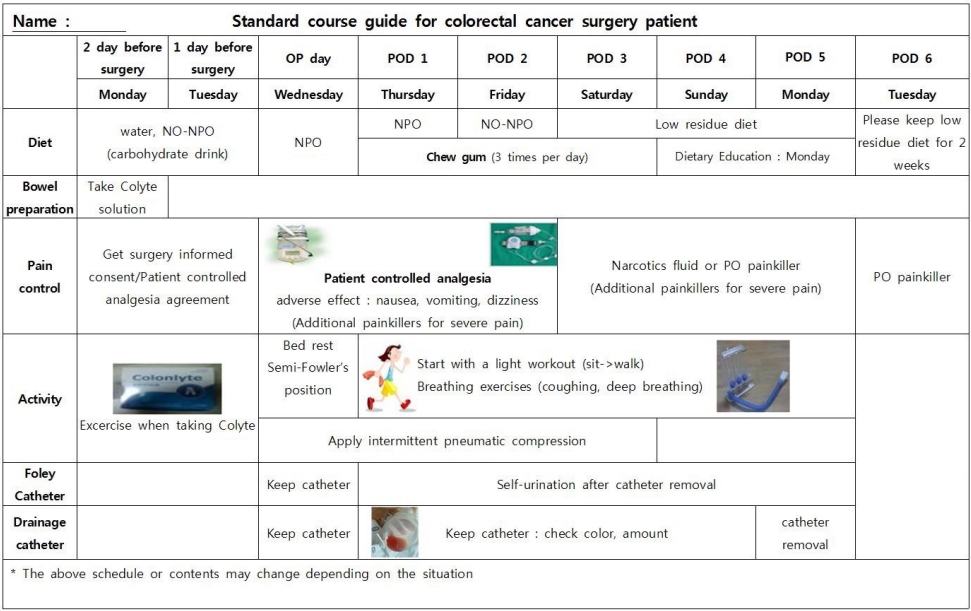
Before surgery, medical professionals explained the overall treatment plan and timetable to patients. A diagram of the treatment plan and timetable was attached to the patientŌĆÖs bed to help the patient and their caregivers understand the recovery process after surgery (Fig. 1).
Mechanical bowel preparation was performed using Colyte (Colyte-F powder, Tae Joon Pharm., Seoul, Korea) 2 days before surgery. Water and carbohydrate drinks (No-NPO, Newcare, Daesang Wellife, Seoul, Korea) were allowed until two hours before surgery.
A nasogastric tube was not inserted. A urinary catheter was inserted soon after general anesthesia was induced and was removed one day after surgery. Patients were allowed to drink water and eat a soft diet starting on the first postoperative day after colon surgery and on the third postoperative day after rectal surgery. The drain was removed 3ŌĆō5 days after surgery depending on medical situation. The Department of Nutrition provided patents with dietary education during hospitalization. If there were no (suspected) surgical complications and the physical examination and laboratory tests were stable postoperatively, discharge was recommended.
The patients were divided into the following 2 groups: (1) group A, those who complied with the medical professionalŌĆÖs decision to discharge; and (2) group B, those who refused discharge despite the medical professionalŌĆÖs decision. The factors affecting patient discharge were analyzed.
Statistical analysis was performed using independent t-test, chi-square test, and linear by linear association. Statistical significance was considered at a P-value <0.05.
A total of 91 patients completed the questionnaire during the study period. Their mean age was 60.1 years. The male to female ratio was 1.27:1. Fifty-three cases (58.2%) were colon cancer, while 38 (41.7%) were rectal cancer. The mean length of postoperative hospital stay was 6.8 days. Twenty-five patients (27.5%) did not have a spouse, and 16 patients (17.6%) lived alone. Twenty-one patients (23.1%) did not have a caregiver after discharge. Although the government medical insurance covers the entire Korean population, 44 patients (48.4%) also had private medical insurance (Table 1).
In part 2 of the preoperative questionnaire, 16 patients (17.6%) answered that expected to be discharged when they could eat more than 2/3 of a meal. In contrast, 35 patients (38.5%) replied that the amount of food would not affect the discharge decision. With regard to bowel activity, 54 patients (59.4%) preferred to have one or more postoperative bowel movements before discharge, while 19 patients (20.9%) did not consider this an important factor for discharge. In terms of pain, 52 patients (57.1%) wanted visual analogue scale (VAS) score <2, while 22 (24.2%) wanted VAS score <4 prior to discharge. Finally, 9 patients (9.9%) answered that degree of pain would not affect their discharge decision. Twenty-seven patients (30%) answered that they expected to be discharged when they assumed full activity, while 46 patients (50.5%) considered partial activity sufficient for discharge (Table 2). Overall, preoperatively, patients considered activity, amount of food intake, and bowel movements to be the most important factors influencing discharge decisions. In contrast, they considered pain, ability to pay, and presence of caregivers to be relatively less important (Fig. 2).
The mean hospital stay after surgery was 6.8 days. When discharge was recommended by medical professionals, 17 patients (18.7%) refused for the following reasons: subjective abdominal pain or discomfort (9 cases); absence of a caregiver at home (3 cases); a long distance between the hospital and home (4 cases); and voiding discomfort (1 case). We divided patients into 2 groups, which were comparable with regard to baseline characteristics (Table 3). Postoperative complications occurred in 16 patients (17.4%), including 12 cases in group A and 4 cases in group B. There was no significant difference in complication rate between the 2 groups. Group A had 1 case of bleeding, 4 cases of ileus, 3 cases of urinary retention, 3 cases of anastomotic leakage, and 1 case of bowel evisceration. The case of bleeding was controlled with endoscopy. The 2 cases of anastomotic leakage and 1 case of bowel evisceration required a second surgery. The other complications were treated conservatively. Group B had 1 case of bleeding, 2 cases of urinary retention, and 1 case of ileus, all of which were treated conservatively. According to the Clavien-Dindo classification, group A had 3 cases of grade I, 5 cases of grade II, and 4 cases of grade III, while group B had 2 cases of grade I and 2 cases of grade II. There were no significant differences between the 2 groups with regard to patient age, sex, cancer location, tumor size, pathologic outcomes, or postoperative diet. Intraoperative blood loss was significantly larger in group B than in group A (60.4 mL vs. 92.1 mL, P = 0.003) There was no significant difference in length of hospital stay between the 2 groups (6.68 days vs. 7.35 days, P = 0.316). There were also no significant differences in readmission rates between the 2 groups (6.8% vs. 11.8%, P = 0.611). The reasons for readmission in group A were 2 cases of poor oral intake, 2 cases of ileus, and 1 case of anastomotic leakage. The reasons for readmission in group B were 1 case of diarrhea and 1 case of anal pain (Table 4).
Postoperatively (based on questionnaire part 3), there were no significant differences between the groups with regard to patient diet satisfaction, subjective gastrointestinal symptoms, or subjective activities of daily living. However, when a linear-versus-linear association was compared, there were significant differences between the group with regard to subjective pain (P = 0.040), ability to walk for a prolonged period (P = 0.005), and presence of fatigue (P = 0.031) (Table 5).
The combination of minimally invasive surgery and well-organized postoperative management program is important to reduce hospital stay [3, 4, 14]. Many medical institutions have applied ERAS or CP in practice to enhance patient recovery and shorten hospital stay after laparoscopic surgery [14, 15]. Good compliance, which may be influenced by subjective patient factors, is essential to obtain excellent clinical outcomes with ERAS or CP. However, there is a little research to substantiate this hypothesis. Therefore, studies that address the effect of subjective patient factors on compliance (with ERAS or CP) are needed to improve patient satisfaction and postoperative management.
In this study, we used the Likert scale in a questionnaire to estimate subjective needs, expectations, and patient satisfaction. The Likert scale has been used in many previous studies and produces comparable results to those of the VAS scale and patient status measurements [16].
We also investigated patient preoperative needs. Although preoperative counseling is thought to reduce hospital length of stay [17], this had never been demonstrated with regard to patient indication for discharge. Therefore, we estimated patientsŌĆÖ expectation criteria for discharge, including the amount of food intake, number of bowel movements, pain level, and activity level. We evaluated for a relationship between socioeconomic status and discharge decision. Previous studies suggested that higher income is associated with shorter hospital length of stay and higher patient satisfaction [18, 19]. In contrast, we found that those with higher income tended to have a higher rejection rate, although the difference was not statistically significant. Other socioeconomic status factors were not significantly different between the groups. We found that patients considered amount of food, bowel movements and their degree of activity to be important factors for discharge. In contrast, the presence of a caregiver, their ability to pay, and pain level were not significant factors for discharge.
Seventeen patients (18.7%) in this study refused the medical professionŌĆÖs discharge recommendation. Patients who refused this recommendation had significant differences in subjective pain and fatigue compared to those who accepted the medical professionŌĆÖs discharge recommendation. Practically, there were no objective complications or abnormalities in laboratory findings of patients in group B. Therefore, both objective medical findings and subjective patient symptoms are essential with regard to timing of discharge after surgery. Many studies have not only investigated the relationship between pain control and number of hospital days after surgery, but also have described several methods to reduce postoperative pain [20, 21]. However, the majority of these prior studies only estimated objective values with regard to pain, including amount of analgesics used, VAS score, and inflammatory response [22]. In contrast, medical professionals typically consider both objective and subjective patient findings before making a decision to discharge.
In this study, despite no objective medical abnormalities (including VAS, laboratory findings, and complications), some patients were still uncomfortable or experienced fatigue and therefore declined to be discharged. Postoperative fatigue is considered an important complication after surgery. The risk of postoperative fatigue is higher in patients who are elderly, have low nutritional status, or who have undergone gastrectomy. Laparoscopic surgery may reduce the incidence of postoperative fatigue [23]. Factors that may cause fatigue after surgery should be well estimated and managed. Fatigue is a subjective factor that may be overlooked. Therefore, care should be taken.
There were 17 people in the study who refused to be discharged despite the absence of any postoperative complications. However, discharge was recommended based on objective medical values, without considering subjective patient symptoms. However, this strategy did not meet the patientsŌĆÖ expectation criteria for discharge.
In general, factors that influence length of hospital stay after surgery include surgical factors such as surgical complications and objective factors such as age, American Society of Anesthesiologists physical status classification grade, and patient frailty [9, 10, 24, 25]. We found that intraoperative blood loss was lower in group A than it was in group B, but no patient required blood transfusion. We also demonstrated that subjective factors, such as patient pain and fatigue at time of discharge were important. Hospital length of stay was slightly longer in group B than in group A, although the difference was not statistically significant. There was significant difference in intraoperative blood loss between the groups. However, there was no serious bleeding that required blood transfusion, which seemed to prevent an influence on length of hospital stay. This finding may be explained by our typical education of the patient about his/her objective findings so that he/she understands the rationale for discharge. We also delayed discharge if complications occurred or if there was an objective abnormality. There was no significant difference in hospital length of stay between the 2 groups.
This study has several limitations. First, it was a single-center experience with a small sample size. Therefore, the study was unable to accurately measure a patientŌĆÖs subjective symptoms. Therefore, a larger, multicenter study is needed to substantiate our findings.
In conclusion, preoperatively, patients considered presence of a bowel movement, amount of food tolerated, and activity level as the most important factors to determine discharge. Patients who refused discharge were more likely to have subjective pain and fatigue than were those who accepted plans for discharge. Therefore, decisions regarding discharge must not only consider the objective medical factors, but also subjective patient factors.
Fig.┬Ā1.
Treatment plan and timetable. OP, operation; POD, postoperative day; NPO, none per-oral; PO, per-oral.
Table┬Ā1.
Baseline patient characteristics
Table┬Ā2.
Patient preferences at discharge
Table┬Ā3.
Baseline characteristics by group
Table┬Ā4.
Characteristics of the groups by decision regarding discharge
Values are presented as mean ┬▒ standard deviation, number (%), or mean (range).
Group A, patients who complied with the medical professionalŌĆÖs decision to discharge; group B, patients who refused discharge despite the medical professionalŌĆÖs decision; ASA PS, American Society of Anesthesiologists physical status.
Table┬Ā5.
Subjective discomfort by group
REFERENCES
1. Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 2014;15:767ŌĆō74.


2. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718ŌĆō26.


3. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 2005;6:477ŌĆō84.


4. Laparoscopically assisted colectomy is as safe and effective as open colectomy in people with colon cancer Abstracted from: Nelson H, Sargent D, Wieand HS, et al; for the Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050-2059. Cancer Treat Rev 2004;30:707ŌĆō9.


5. van der Pas MH, Haglind E, Cuesta MA, F├╝rst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 2013;14:210ŌĆō8.


6. Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(┬«)) Society recommendations. World J Surg 2013;37:259ŌĆō84.



7. Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, et al. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 2005;24:466ŌĆō77.


8. King PM, Blazeby JM, Ewings P, Longman RJ, Kipling RM, Franks PJ, et al. The influence of an enhanced recovery programme on clinical outcomes, costs and quality of life after surgery for colorectal cancer. Colorectal Dis 2006;8:506ŌĆō13.


9. Keller DS, Bankwitz B, Nobel T, Delaney CP. Using frailty to predict who will fail early discharge after laparoscopic colorectal surgery with an established recovery pathway. Dis Colon Rectum 2014;57:337ŌĆō42.


10. Boulind CE, Yeo M, Burkill C, Witt A, James E, Ewings P, et al. Factors predicting deviation from an enhanced recovery programme and delayed discharge after laparoscopic colorectal surgery. Colorectal Dis 2012;14:e103ŌĆō10.


11. Oh HK, Ihn MH, Son IT, Park JT, Lee J, Kim DW, et al. Factors associated with failure of enhanced recovery programs after laparoscopic colon cancer surgery: a single-center retrospective study. Surg Endosc 2016;30:1086ŌĆō93.



12. Khan S, Wilson T, Ahmed J, Owais A, MacFie J. Quality of life and patient satisfaction with enhanced recovery protocols. Colorectal Dis 2010;12:1175ŌĆō82.


13. Alawadi ZM, Leal I, Phatak UR, Flores-Gonzalez JR, Holihan JL, Karanjawala BE, et al. Facilitators and barriers of implementing enhanced recovery in colorectal surgery at a safety net hospital: a provider and patient perspective. Surgery 2016;159:700ŌĆō12.


14. Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 2014;38:1531ŌĆō41.



15. Rossi G, Vaccarezza H, Vaccaro CA, Mentz RE, Im V, Alvarez A, et al. Two-day hospital stay after laparoscopic colorectal surgery under an enhanced recovery after surgery (ERAS) pathway. World J Surg 2013;37:2483ŌĆō9.




16. Guyatt GH, Townsend M, Berman LB, Keller JL. A comparison of Likert and visual analogue scales for measuring change in function. J Chronic Dis 1987;40:1129ŌĆō33.


17. Forsmo HM, Pfeffer F, Rasdal A, ├śstgaard G, Mohn AC, K├Črner H, et al. Compliance with enhanced recovery after surgery criteria and preoperative and postoperative counselling reduces length of hospital stay in colorectal surgery: results of a randomized controlled trial. Colorectal Dis 2016;18:603ŌĆō11.


18. Stock GN, McDermott C, McDermott M. The effects of capital and human resource investments on hospital performance. Hosp Top 2014;92:14ŌĆō9.


19. Poole L, Leigh E, Kidd T, Ronaldson A, Jahangiri M, Steptoe A. The combined association of depression and socioeconomic status with length of post-operative hospital stay following coronary artery bypass graft surgery: data from a prospective cohort study. J Psychosom Res 2014;76:34ŌĆō40.



20. Sarin A, Litonius ES, Naidu R, Yost CS, Varma MG, Chen LL. Successful implementation of an Enhanced Recovery After Surgery program shortens length of stay and improves postoperative pain, and bowel and bladder function after colorectal surgery. BMC Anesthesiol 2016;16:55.



21. Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 2012;55:1183ŌĆō94.


22. Aljabi Y, El-Shawarby A, Cawley DT, Aherne T. Effect of epidural methylprednisolone on post-operative pain and length of hospital stay in patients undergoing lumbar microdiscectomy. Surgeon 2015;13:245ŌĆō9.


23. Yu J, Zhuang CL, Shao SJ, Liu S, Chen WZ, Chen BC, et al. Risk factors for postoperative fatigue after gastrointestinal surgery. J Surg Res 2015;194:114ŌĆō9.


-
METRICS

- Related articles in ACP
-
Reconsideration of the Safety of Laparoscopic Rectal Surgery for Cancer2019 October;35(5)








