INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of cancer-related death in Korea. The incidence of CRC is currently rising with increasing age. The median age at diagnosis of CRC is 67 years, with one-third of patients older than 75 years [
1]. As the population continues to grow older, the incidence of colon cancer in octogenarian and nonagenarians is expected to increase [
2]. Therefore, these far-elderly patients are expected to comprise a substantial proportion of CRC patients.
Until now, evidence establishing the impact of age of onset of CRC on tumor behavior is conflicting. Previous studies have suggested that survival rates for older patients with CRC may be worse than that for younger patients [
3-
6]. These studies have suggested that the poorer outcomes for older patients may be related to higher rates of morbidity, mortality, and hospital readmission after surgery [
7]. However, other studies have indicated similar survival rates for both older and younger patients with CRC who have undergone curative surgery [
3]. Moreover, octogenarian and nonagenarian patients have been excluded in a number of clinical trials [
8,
9]. Hutchins et al. [
10] reported that only 14% of elderly CRC patients (aged > 70 years) enrolled in clinical trials.
As the disease burden of CRC in elderly patients continues to rise, a more comprehensive understanding of the impact of increasing age on clinical and pathological parameters is essential. Therefore, we examined patients older than 80 years according to their clinical and pathological characteristics including survival rates to fully understand the increasing population of elderly patients with CRC.
METHODS
This study was a retrospective, single-center cohort study. The study population included consecutive patients with CRC who were 60 years old or older at diagnosis, who had undergone curative resection for primary CRC between 2009 and 2014 at Ajou University Hospital (Suwon, Korea). For the patients with stageIV CRC, additional local treatment such as surgical resection or radiofrequency ablation for metastatic lesion was recommended. As a large number of elderly patients with rectal cancer did not receive neoadjuvant chemoradiation, patients with middle-to-low rectal cancers were excluded from the study. The patients were divided into 2 groups: elderly (aged > 80 years, n= 133), and controls (aged 60 to 79 years, n= 596). Medical records of all the patients were retrieved from the database of Ajou University Colon Cancer Center and were reviewed with regard to patients’ demographics, risk factors for the prognosis of CRC, Clinicopathological parameters, treatment given, complications, and survival rates. The data between the 2 groups were compared.
This retrospective study protocol was approved by the Institutional Review Board of Ajou University Hospital (No. AJIRB-MED-MDB-19-447) and written informed consents were waived.
Statistical analysis
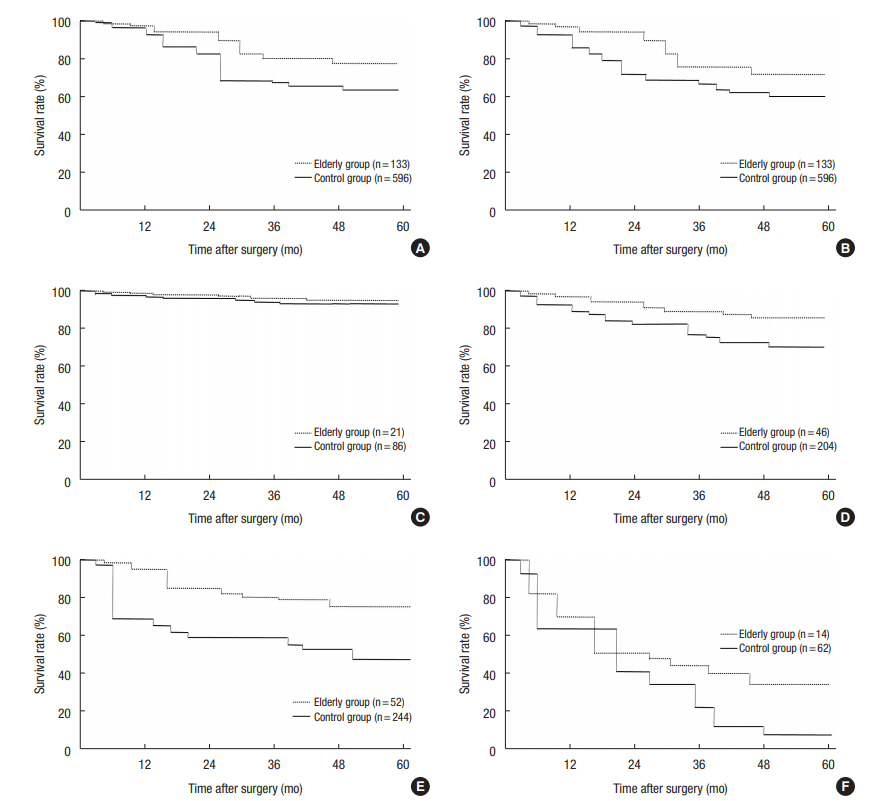
Fischer exact test was used to analyze dichotomous variables and the chi-square test was used for variables with more than 2 categories. Statistical analysis was performed using SAS ver. 9.4 (SAS Institute, Cary, NC, USA). The overall survival (OS) rate was assessed by Kaplan-Meier survival analysis, with the log-rank test. Cancer-specific survival and disease-free survival (DFS) rates were assessed using the Cox proportional hazards model, with the Fine and Gray correction for non-cancer-related deaths as a competing risk. Cox proportional hazard models were also applied for multivariate analysis and hazard ratio (HR) estimation. Twosided P values less than 0.05 were considered statistically significant.
DISCUSSION
Average life expectancy in developed countries is reaching 90 years. Despite the growth of the elderly population, current literature does not describe the unique characteristics or clinical management of this subpopulation. Data regarding very elderly patients, such as nonagenarians, are even rarer. In this study, we observed that increasing age was generally associated with worse outcomes. Previous studies have suggested that the survival rates of elderly CRC patients may be worse than those of younger patients. The poorer outcomes in elderly patients were understood to be related to higher rates of morbidity and mortality, and repeated hospitalization after surgery [
7]. However, other studies have implied similar survival rates between elderly and younger patients [
3]. Irvin [
8] reported that after correction for the patient’s age, survival rates were similar between old and young patients. Therefore, it can be concluded that the age is a confounding factor for the prognosis of CRC. Patel et al. [
11] demonstrated that older age was associated with alterations in clinical and pathological characteristics and lower survival rates. They also suggested that colon cancer phenotype and the efficacy of colon cancer treatments might be dependent on the age. The results of these contradictory papers were the reason to perform this study.
A correlation between age at onset and tumor sidedness has been reported, albeit inconsistently [
11]. It is likely that there is a tendency for tumor location to shift from left to right with increasing age. The exact reason for this shift remains unclear. Conflicting results have been reported with regard to prognosis and tumor sidedness. A recent investigation from Mayo Clinic revealed that the prognosis of CRC is significantly related to tumor location; rectal cancer had the best outcome, followed by left side cancer, and right-sided cancer had the worst [
12]. Although it was a single-center study, more than 20,000 patients had been observed for 4 decades. In the present study, overall tumor sidedness was not a prominent predictive factor for colon cancer. However, the incidence of rectal cancer was significantly lower in octogenarian and nonagenarians. We suggest that the relative infrequency of rectal cancer might have contributed to the poor prognosis in elderly patients. In the present study, there was no difference in the incidence of MSI in the cancer tissue between elderly patients and the control group. As tumor sidedness was not different between the groups, this result was not unexpected. Some researchers from the Western hemisphere have reported that octogenarians have a clear predilection for right-sided colon cancers [
13-
15]. This finding might suggest a distinct pathogenesis of CRC among older patients, such as a higher rate of mismatch repair protein deficiency or its phenotype, high-frequency MSI tumors. We could not conclude whether the discrepancy between our results and those of others was because of ethnic differences or the limited number of study patients.
Studies regarding elderly CRC patients showed conflicting results in terms of treatment outcomes. Widdison et al. [
16] could not demonstrate a survival rate difference between elderly and younger patients, whereas Mulcahy et al. [
3] demonstrated better outcomes in elderly patients. Investigators including McMillan et al. [
17] showed poorer outcomes in elderly patients. Since the elderly patients had more comorbidities than the control group, the OS rate could be affected by associated diseases. Therefore, anlaysis of DFS is more appropriate in this kind of cohort study. Our results show that treatment outcomes in elderly patients were poorer in both the OS and DFS.
As the mainstay of curative CRC treatment remains surgical resection, poorer treatment outcomes in the elderly patients might be because of a less aggressive surgical approach. As shown in
Table 1, elderly patients in this study showed poorer general physical condition and more comorbidities than did the control group. It is probable that the approach in most patients with poor health may be less aggressive. Dutch researchers have reported a significantly low number of harvested lymph nodes in specimens from elderly patients [
18]. Numbers of harvested regional lymph nodes are considered a surrogate marker of radicality of surgery in CRC. In this study, however, the average numbers of harvested nodes were similar between the groups. Therefore, the surgical extents could not be an explanation for the poorer outcome in elderly patients. In addition to radical surgery, chemotherapy is also mainstay of treatment for metastatic CRC and standard adjuvant treatment for stage-III CRC. In concordance with previous studies, the majority of elderly patients in the present study were less likely to receive chemotherapy for both metastasis and adjuvant therapy [
10]. The chemotherapy omission rate in elderly patients was not clearly demonstrated. Landrum et al. [
19] reported that among patients who did not receive chemotherapy for stage-III CRC, 58% had declined chemotherapy. Patients older than 80 years have been excluded from almost all clinical trials regarding chemotherapy. In our study, only 13.4% of stage-III CRC and 14.2% of stage-IV CRC cases were treated with chemotherapy in the elderly patients [
20]. The exact reasons for the omission of chemotherapy were not explored in our study. Multiple reasons have been suggested to account for this phenomenon, including the presence of comorbidities, history of prior malignancies, lack of awareness regarding chemotherapy, and skepticism of the caregivers and the patient’s family regarding the ability of elderly patients to tolerate the therapy. However, this factor could be a possible explanation for a poorer outcome.
The outcome disparity between the elderly and the control group was also found in patients with stage-II CRC. Almost all patients in this stage did not receive adjuvant chemotherapy. The 5-year DFS of patients with stage-II CRC was 70.7% in the elderly, and 85.6% in the control group. Earlier studies suggested that elderly patients having multiple comorbidities, postoperative complications, and multiple readmissions might have higher survival rates [
7]. However, in our study, we found the 30-day mortality rates to be similar between the 2 groups and that the difference between OS and DFS was small. We conclude that poorer outcomes in elderly patients are not simply a result of patient comorbidities or postoperative complications, and that cancer possibly recurs because of differences in tumor characteristics.
Analysis of the prognostic factors failed to identify differences between the elderly and control groups. In both groups, cellular differentiation, lymphovascular invasion, preoperative CEA, and cancer stage proved to be the meaningful factors in univariate analysis. These results were similar to previously reported results. Multivariate analysis regarding the entire study population showed that pathologic stage and poor differentiation of tumor cell were the 2 strongest prognostic factors in both groups. Current retrospective study shows far-elderly patients with CRC tend to undergo standard treatment less frequently than the control group. And their OS and DFS were inferior compared to the control group. As the number of elderly patients with CRC continues to increase, our results provide a basis for further clinical and molecular biological investigations of elderly CRC patients.
Limitations of this study include the retrospective methodology that may have caused bias because of unknown or unrecorded confounders. As this is a single-center study, it is more vulnerable to such bias. In addition, the small number of patients enrolled with CRC treated at our center might not have been sufficient. As with other reports, the majority of patients with stage-III and stage-IV CRC were under-treated with chemotherapy. This might explain the bias. However, a surgical bias was not noted in this study. Previous studies have reported significantly lower numbers of retrieved lymph nodes examined and a decreased rate of lymph node positivity in elderly patients. These may have been the reason for conflicting results between cancer stages.