Early Postoperative Anastomotic Obstruction Due to an Intraluminal Blood Clot After Laparoscopic Anterior Resection: A Case Report
Article information
Abstract
Early postoperative anastomotic obstruction after colorectal surgery rarely develops. Herein, we present a case of a 50-year-old healthy woman who had an early postoperative anastomotic obstruction which was revealed caused by a blood clot and successfully managed by endoscopic approach. The patient was discharged after laparoscopic anterior resection and visited the emergency department one day after because of abdominal pain. Computed tomography showed that the anastomosis site was obstructed with low-density material. Intraoperative endoscopy was performed under general anesthesia and blood clot filling the lumen were identified. As the scope was advanced to the blood clot with air inflation, the blood clot was evacuated. The anastomosis site could be obstructed by blot clot with mucous debris albeit it is a rare condition. An endoscopic approach seems to be the first option in the diagnosis and treatment of postoperative obstruction at the anastomosis site and it could prevent unnecessary laparotomy.
INTRODUCTION
Colorectal surgery has approximately 35% risk of postoperative morbidities. Among the morbidities, significant postoperative bleeding occurs in approximately 4.5% of colorectal surgeries [1]. However, a mild bleeding often occurs when gastrointestinal anastomosis is performed, but most of these are self-limiting. This blood with small blood clots is often defecated with the first bowel movement.
Meanwhile, the incidence of early postoperative small bowel obstructions is 9.5% [2]. However, postoperative obstruction at the anastomosis site has been rarely reported [3]. Although several small bowel obstructions due to large blood clots have been reported after small intestinal anastomosis [4-10], to the best of our knowledge, there are no reports on colonic obstruction at the anastomosis site due to large blood clots.
We encountered a patient who developed this rare complication and was managed by colonoscopic evacuation and herein present her case. This study was approved by the Institutional Review Board of Asan Medical Center (No. 2020-0266), and the informed consent was obtained.
CASE REPORT
A 50-year old healthy woman underwent colonoscopy at a local clinic, and an approximately 15-mm tumor at the sigmoid colon was identified. Endoscopic submucosal dissection was performed. The tumor pathologically invaded the submucosa (3 mm from the muscularis mucosae) and involved a deep resection margin. Thus, the patient was referred to our institution for radical resection. The patient has no underlying disease. The past medical history was also not remarkable, and there was no history of previous abdominal surgery. The preoperative laboratory test results were all within normal limits, including coagulation profiles.
Laparoscopic anterior resection was planned. Mechanical bowel preparation was performed preoperatively using sodium picosulfate with magnesium citrate (Picosolution, Pharmbio Korea, Seoul, Korea) and oral antibiotics (metronidazole 500 mg, ciprofloxacin 500 mg). On the day of surgery, the patient had menstruation. During the surgery, the inferior mesenteric artery was ligated near the origin after mobilization of the colon. The distal bowel was transected with a linear stapler (Signia Tri-Staple with 60-mm purple cartilage, Medtronic, Dublin, Ireland). An end-to-end anastomosis was made using double stapling technique with 28-mm circular stapler (AutoSuture CEEA, Covidien, Dublin, Ireland). The anastomosis site was adequately made without tension and twisting of the mesentery. The air-leak test was performed, which showed a negative result. The surgery was completed without any unexpected events. After the surgery, the patient recovered well without postoperative complications. The routine abdominal radiography was performed on postoperative day (POD) 3, which showed colonic gas pattern (Fig. 1A). Thus, the patient was discharged on POD 4, although the flatus and defecation were not identified because the flatus passage was expected soon.
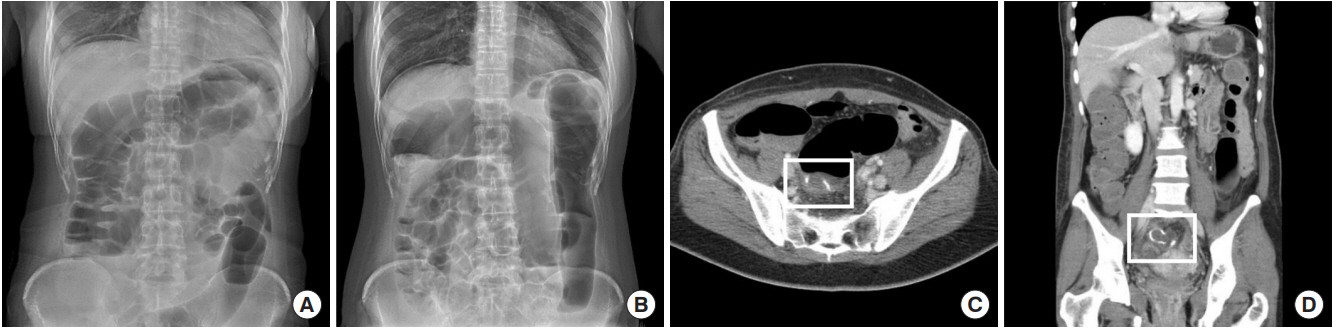
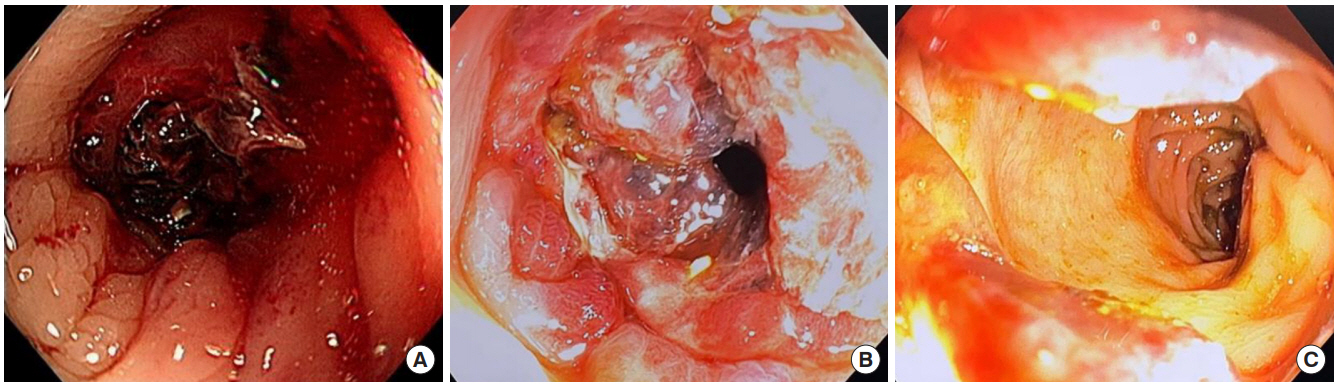
(A) Simple abdominal X-ray findings at postoperative day 3. (B–D) Simple abdominal X-ray and computed tomography findings of anastomotic obstruction caused by intraluminal blood clot obtained at the emergency department.
After 1 day, the patient visited the emergency department due to abdominal pain. The patient stated that an approximately 5-cm blood clot had passed after using suppository (Dulcolax, Boehringer Ingelheim, Ingelheim, Germany). Simple abdominal radiography revealed dilatation of the colon, and computed tomography revealed obstruction of the anastomosis site with low-density material and dilation of the upstream colon. The stapled anastomosis ring was intact, and there was no evidence of inflammation around the anastomosis (Fig. 1B–D). The laboratory test results were normal. A nasogastric tube was inserted, and conservative treatment was initiated. The symptom persisted, and sigmoidoscopy was performed the following day. Blood clot filling the lumen and edematous bowel was identified (Fig. 2A). The physician who performed sigmoidoscopy could not remove the blood clot because of concerns on anastomotic disruption and completion of the examination. Following the sigmoidoscopy, the patient was transferred to the operating room. Before undergoing laparotomy, the surgeon performed intraoperative endoscopy under general anesthesia. As the scope was advanced to the blood clot with air inflation, the blood clot was evacuated, and scope could pass the anastomosis (Fig. 2B, C). Thus, laparotomy was canceled, and the patient was returned to the ward. After intraoperative endoscopy, several flatus and stool were passed, and no bleeding was identified. The patient was discharged the following day without discomfort. After 10 days, the patient visited the outpatient clinic for routine follow-up and had no abdominal symptoms.
DISCUSSION
After colorectal surgery, some hemorrhages may occur at the anastomosis site, and most of these cease within 24 hours. Moreover, patients often show small amount of blood clots in the stool with the first postoperative bowel movement. Approximately 9.6% of hemorrhages were found at the anastomosis site on intraoperative colonoscopy, which was performed after anastomosis [11]. Nevertheless, sometimes, hemorrhage continues. Meanwhile, early postoperative obstruction (obstruction that develops within 30 days) develops in up to 10% of patients after colorectal surgery. Furthermore, some patients needed reoperation, and most cases can be managed with conservative treatment [2]. However, almost all postoperative obstructions develop in the small bowel. Postoperative colonic obstruction rarely develops [3].
Nevertheless, postoperative bowel obstruction caused by blood clot is a rare event. There are a few published cases of postoperative small bowel obstruction caused by intraluminal blood clot after Roux-en-Y gastric bypass [4-9] and hepaticojejunostomy [10]. However, postoperative colonic obstruction caused by intraluminal blood clot is very rare. This may be because the small bowel has smaller diameter and lower degree of distensibility.
Interestingly, all patients whose small bowels were obstructed by intraluminal blood clot after small intestinal surgery were female [4-10], and the patient in this case was also female. Men have higher risk of cardiovascular diseases, and it seems that sex hormones are associated with the development of cardiovascular diseases [12]. The sex difference seems to have an influence on hemostatic function, and it seems to be the cause of different risks of cardiovascular disease. Platelet reactivity seems different between men and women. The platelet in women is less reactive and less prothrombotic [12, 13]. Lawrence et al. [13] found that the platelet in women has 22% lower adherence ability to human arterial subendothelium (P < 0.001). Moreover, the bleeding time is slightly shorter in women (4.8± 0.3 minutes vs. 5.7± 0.4 minutes, P= 0.118). The authors concluded that blood in men has higher primary hemostatic activity. Additionally, the blood in premenopausal women has less prothrombotic activity than postmenopausal women [12]. Indeed, the 10 patients who developed small bowel obstruction by intraluminal blood clot after gastric bypass had young age, and their mean age was 39.2 years (range, 27 to 53 years) [4-9].
In contrast, menstruation is another suspected cause of formation of blood clot in this patient. Menstruation seems to affect hemostatic function. A systematic review focused the variation of some hemostatic factors affected by the menstrual cycle [14]. They demonstrated that the hemostatic variables, such as von Willebrand factor, factor VIII, and platelet function, fall at the lowest levels during the menstrual and early follicular phases.
Unlike small bowel obstruction, obstruction at the anastomosis site needs immediate management because it could lead to anastomosis leakage and perforation. In small bowel anastomosis, an endoscopic approach is usually difficult and most obstructions with intraluminal hematoma were managed with reoperation [4, 6-10]. However, the anastomosis site at the large bowel could be easily accessed with the endoscopic approach. Indeed, endoscopic management is a useful and feasible option for postoperative bleeding. Among the patients with postoperative anastomotic bleeding, 85% of patients were successfully managed with nonoperative treatment [15]. Although there is a concern about anastomotic damage by performing endoscopy in early the postoperative period, intraoperative endoscopy immediately after anastomosis was a safe method to assess the anastomosis site [11] and endoscopy seems to be performed safely during the early postoperative period. A case of early postoperative anastomotic obstruction caused by edema was also successfully and safely managed with endoscopic treatment [3]. The patient in this case was also managed with the endoscopic approach and could avoid unnecessary laparotomy.
Therefore, the anastomosis site could be obstructed by blood clot with mucous debris after stapled colorectal anastomosis albeit it is rare condition. Menstruation in premenopausal women could be a risk factor for formation of hematoma at the anastomosis site. The anastomosis site could be easily and safely approached with endoscopy. The endoscopic approach seems to be the first option in the diagnosis and treatment of postoperative obstruction at the anastomosis site and could prevent unnecessary laparotomy.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.