Minimal Lateral Internal Sphincterotomy (LIS): Is It Enough to Cut Less Than the Conventional Tailored LIS?
Article information
Abstract
Purpose
Anal fissure is a common anorectal condition, yet its pathogenesis remains unclear. Lateral internal sphincterotomy (LIS) is the gold standard treatment for chronic anal fissures that do not respond to conservative treatment; however, it has a risk of anal incontinence. We believe that fibrosis of the internal anal sphincter is an important factor in the pathogenesis of chronic anal fissure. In this study, we describe the minimal LIS method, a minimally invasive method where only the fibrotic portion of the internal anal sphincter is cut. We also describe the outcomes of this method.
Methods
We performed a retrospective review of 468 patients (270 male and 198 female) who underwent minimal LIS for chronic anal fissure in 2017 at Seoul Song Do Hospital. We analyzed the patients’ clinical characteristics, manometry data, complications, and outcomes of minimal LIS. The outcomes of the surgery were assessed via questionnaires during the postoperative outpatient visits, beginning 2 weeks postoperatively.
Results
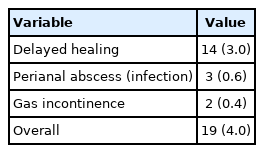
The overall complication rate was 4.0% (19 patients). Delayed healing occurred in 14 patients (3.0%), perianal abscess was present in 3 patients (0.6%), and gas incontinence occurred in 2 patients (0.4%). All complications were improved with conservative treatment. Recurrence, defined as the recurrence of anal fissure more than 4 weeks after healing, was present in 6 patients (1.3%).
Conclusion
Minimal LIS is a safe and effective treatment option for patients with chronic anal fissure. Postoperative complications, especially incontinence and recurrence, are rare.
INTRODUCTION
An anal fissure is a common anorectal disease involving approximately 10% of all proctological patients [1]. It is characterized by bleeding and painful longitudinal tears in the squamous epithelium of the anal canal from the dentate line extending distally to the anal verge [2]. The pathogenesis and etiology of anal fissure remain unclear. Anal sphincter hypertonia, fibrosis, local trauma, and ischemia have been proposed as causes of anal fissure, though this has not yet been clarified [3].
Lateral internal sphincterotomy (LIS) is regarded as the gold standard and first-line surgical treatment for chronic anal fissures that do not respond to conservative treatment [4]. However, the risk of postoperative morbidity, including anal incontinence, is reported to be as high as 47.6% [5]. Modified surgical techniques such as partial LIS and tailored LIS have been suggested as better methods that can minimize anal sphincter injury and can reduce complications, including incontinence. Currently, the patient’s quality of life (QOL) has become one of the most important aspects in healthcare. When choosing the optimal treatment method, it is important to consider the risk of surgical complications that may have a critical impact on the patient’s QOL [6]. At our institution, we have been attempting to modify conventional techniques and develop new methods to minimize damage to the anal sphincter caused by the surgical procedure of LIS.
We believe that fibrosis of the internal anal sphincter plays a significant role in the pathogenesis of chronic anal fissure [7]. To minimize anal sphincter injury, we perform minimal LIS, a minimally invasive technique specifically tailored to each patient. Compared with the conventional tailored LIS that requires an incision to the internal anal sphincter to the depth of the epithelial tear, our minimal LIS method requires an incision only to the fibrotic band. The fibrotic band is a portion of the internal anal sphincter inflicted by fibrosis, and it is more superficially located than the epithelial tear. Thus, minimal LIS is less invasive than conventional tailored LIS.
The aim of our study was to describe the minimal LIS method and assess its clinical feasibility and effectiveness for chronic anal fissure. In addition, we aimed to determine if minimal LIS is safe to perform in patients without sphincter hypertonicity who are thought to be at a high risk of the postoperative complication of anal incontinence.
METHODS
This study was exempted from ethics approval and informed consent by the Institutional Review Board of the Seoul Song Do Hospital due to its retrospective nature (No. 2020-014).
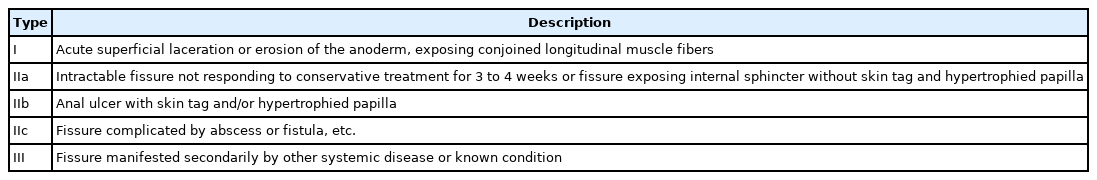
We performed a retrospective review of 468 patients with chronic anal fissure who underwent minimal LIS in 2017 at Seoul Song Do Hospital in Seoul, Korea. Our unique anal fissure classification system, the Song Do Classification of Anal Fissures (Table 1), was used to classify patients with chronic anal fissure. In contrast to the vague, time-based criteria of the conventional anal fissure classification system, our system also incorporates a definite anatomical change, the exposure of the internal anal sphincter. Only patients with chronic anal fissure who met the criteria of the Song Do Classification type II anal fissure were included in this study. All patients underwent clinical and physical evaluations, which included a digital rectal examination, an anoscope examination, a preoperative endoanal ultrasound, and an anorectal manometric evaluation. The preoperative endoanal ultrasound and anorectal manometric evaluation were performed 1 week preoperatively. We used the electronic medical records to review the patients’ demographics, comorbidities, fissure types, presenting symptoms, preoperative pain intensity (rated using the visual analogue scale [VAS]), number of hospitalized days, follow-up period, preoperative manometry data, and postoperative complications. Outpatient postoperative follow-up visits began at 2 weeks postoperatively and continued every 2 to 4 weeks thereafter until complete wound healing and full resolution of the symptoms were achieved. Postoperative complications were assessed via questionnaires during the postoperative visits. A water-perfused high-resolution anorectal manometry system (InSIGHT Ultima, Sandhill Scientific Inc., Highlands Ranch, CO, USA) was used to measure anorectal pressure. The normal range of mean maximum resting pressure (MRP) used in this study was 71 to 90 mmHg for male patients and 64 to 84 mmHg for female patients. This normal value was determined by measuring the MRP of 40 mmHg asymptomatic, healthy volunteers from our medical staff (20 male patients and 20 female patients, aged approximately 20– 60 years) during the installation of a high-resolution anorectal manometry system in 2010. Patients with chronic anal fissure without sphincter hypertonicity were defined as patients with normal or low mean MRP.
Statistical analysis
The Mann-Whitney test and chi-square test were used to compare the normal/low mean MRP and high mean MRP subgroups. The data were evaluated using Microsoft Excel (Microsoft Corp., Redmond, WA, USA) and R software version 4.02 (R Core Team, Auckland, New Zealand). P-values of < 0.05 were considered statistically significant.
Surgical procedure
All patients were admitted to the hospital on the day of surgery. A sodium phosphate enema was preoperatively administered for bowel preparation. Prophylactic antibiotics were not used, and preoperative site markings were not made. All procedures were conducted with the patient in the prone jackknife position under spinal anesthesia. The buttocks were laterally retracted using plasters. The anal canal was visualized using a Hill-Ferguson retractor or Sumikoshi retractor and a longitudinal incision approximately 5 mm in length was made in the anoderm to expose the intersphincteric space at the 3 o’clock direction. The fibrotic band was thoroughly palpated with the index finger, which remained inside the anal canal throughout the procedure. Only the fibrotic band was carefully cut with a blade or monopolar electrosurgery device, carefully avoiding damage to other tissues. The sphincter division did not exceed each patient’s apex of the epithelial tear. After incising the fibrotic band, a regular anoscope was introduced into the anal canal to verify that the anal canal size had been modified appropriately. The anoderm incision was not closed. If a large skin tag or papilla was present, it was removed to ensure proper drainage from the fissure and to promote healing (Fig. 1). During the first postoperative week, oral antibiotics (metronidazole 500 mg, 3 times daily), stool softeners (magnesium oxide 500 mg, twice daily), and analgesics (loxoprofen 60 mg, 3 times daily) were prescribed. Patients were encouraged to take sitz baths and avoid intense physical activities during the wound healing period.
RESULTS
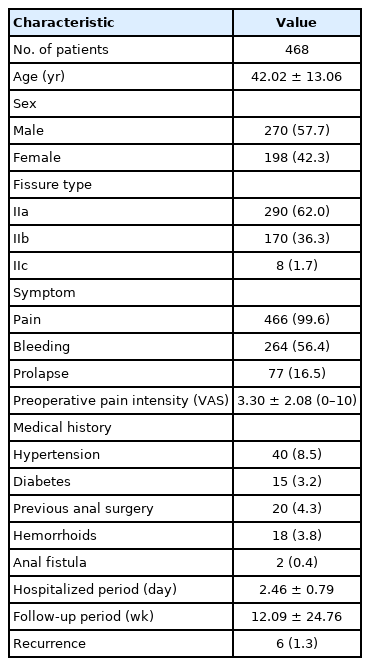
A total of 478 patients underwent minimal LIS in 2017 at our hospital. However, manometry data were missing for 10 patients, who were excluded from the study. As a result, the final analysis included 468 patients, including 270 male patients (57.7%; mean age, 43.1 years; range, 18–77 years) and 198 female patients (42.3%; mean age, 40.4 years; range, 19–80 years). When classified using the Song Do Classification of Anal Fissures, 290 patients (62.0%) had type IIa anal fissures, 170 (36.3%) had type IIb anal fissures, and 8 (1.7%) had type IIc anal fissures. The most common symptoms were pain (466 patients, 99.6%), bleeding (264 patients, 56.4%), and anal prolapse (77 patients, 16.5%). The VAS scores for the severity of pain ranged from 0 to 10, with a mean of 3.3. The surgical procedures were performed by 12 colorectal surgeons. Hypertension was observed in 40 patients (8.5%) and diabetes mellitus in 15 patients (3.2%). Twenty patients (4.3%) had a past history of anal surgery. The mean follow-up period after tailored LIS was 12.09±24.76 weeks (range, 0–132 weeks). Recurrence was present in 6 patients (1.3%) (Table 2).
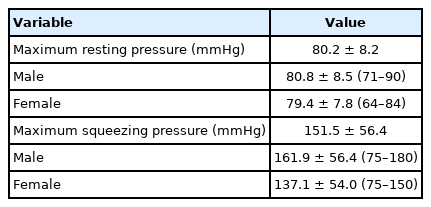
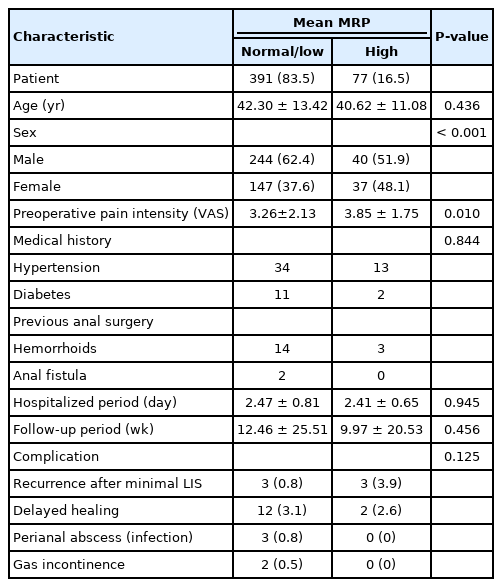
The preoperative mean MRP was 80.2±8.2 mmHg (80.8±8.5 mmHg in male patients and 79.4±7.8 mmHg in female patients). The number of patients with normal or low preoperative mean MRP (≤ 90 mmHg in male patients, ≤ 84 mmHg in female patients) was 391 (83.5%), and the number of patients with high preoperative mean MRP (> 90 mmHg in male patients, > 84 mmHg in female patients) was 77 (16.5%) (Table 3).
The overall complication rate after minimal LIS was 4.0% (19 patients). Delayed healing, defined as anal fissures that did not heal within 4 weeks after surgery, occurred in 14 patients (3.0%). Perianal abscess was present in 3 patients (0.6%), and gas incontinence occurred in 2 patients (0.4%) (Table 4). Perianal abscesses were treated with incision and drainage procedures as well as with antibiotics. Other complications, including gas incontinence, improved with conservative treatment. No patients complained of fecal incontinence, and all patients were successfully treated with no residual symptoms.
A subgroup analysis between the patients with a normal/low preoperative mean MRP and those with a high preoperative mean MRP revealed that there was no statistically significant difference in complications or outcome. Patient sex (P<0.001) and preoperative pain intensity (VAS) (P=0.010) were significantly different between the groups. The complications of perianal abscess and gas incontinence occurred only in patients in the normal/low preoperative MRP group (Table 5).
DISCUSSION
Most anal fissures are successfully treated with conservative treatment over the course of a few weeks. However, surgical treatment is required for chronic anal fissures that do not respond to conservative treatment [8]. There is currently no consensus regarding surgical indications in patients with anal fissure, and surgical treatment has the risk of anal incontinence [9]. Therefore, to lower the risk of anal incontinence, many surgical techniques have been proposed over the decades from manual anal dilation to anal sphincterotomy and anoplasty.
Conventional LIS is recognized as the surgical technique of choice due to its relatively simple procedure and high success rate of 94%. However, the complication risk rate for anal incontinence is reported at an average of 14% [10, 11]. Littlejohn and Newstead [12] proposed the tailored LIS method in 1997. This method aims to tailor the degree of sphincterotomy to the length of the individual fissure. Compared with the conventional LIS method, which divides the internal anal sphincter to the dentate line, tailored LIS preserves more of the internal anal sphincter. Littlejohn and Newstead [12] reported a 99.65% of success rate with complication rates of 1.4% for gas incontinence, 1% for minor staining and urgency, and 1.4% for recurrence in their initial study of 287 patients.
In this study, the outcomes of minimal LIS, which is a less invasive procedure than the conventional tailored LIS, were analyzed using data from 468 patients. We found that minimal LIS had a 96.0% complication-free success rate for fissure healing. The complication rate of 4.0% is relatively lower than 7% to 37% reported in previous studies using other methods [13]. In particular, the gas incontinence rate of 0.4%, and the recurrence rate of 1.3% are low. These successful results are thought to be due to minimal internal anal sphincter injuries, as a result of the minimal LIS method as well as careful surgical patient selection using the Song Do Classification of Anal Fissures system.
Minimal LIS aims to cut and release only the fibrotic band, as it is the fibrotic band that causes narrowing of the anal canal. We believe that the fibrotic band is the main factor that triggers the symptoms of chronic anal fissure and renders chronic anal fissure unresponsive to medical therapy [14]. Therefore, incising only the fibrotic band is sufficient for healing of the chronic anal fissure; sphincter division to the depth of the epithelial tear is not necessary. Due to the limitations of the conventional anal fissure classification system, we used our own unique Song Do Classification of Anal Fissures system. Using this system, we were able to select ideal patients for surgery using the minimal LIS method. The distinct characteristic of this classification system is that it is based on a definite anatomical change: the exposure of the internal anal sphincter. Exposure of the internal anal sphincter can induce inflammation, which leads to fibrosis [3]. Therefore, this classification system allows for the easy and precise identification of patients having chronic anal fissure with fibrosis who require surgery [15].
We used a water-perfused high-resolution anorectal manometry system to measure the anorectal manometry pressures of the patients. The normal mean MRP range used in this study was 71 to 90 mmHg in male patients and 64 to 84 mmHg in female patients. The study group had a mean MRP of 80.2 mmHg, which is within the normal range. Only 16.5% of the patients included in this study were considered to have a high mean MRP. This percentage is lower than expected as patients with chronic anal fissure are typically reported to have a high mean MRP [16]. However, this result is consistent with a previous study that reported that 52.1% of patients with chronic anal fissure had a normal mean MRP [17]. The sliding skin graft (SSG) technique that was first reported by Samson and Stewart [18] is generally recommended for patients with chronic anal fissure and hypotonicity. SSG is reported to have a lower risk of anal incontinence; however, it is more technically difficult than LIS and can lead to complications such as local infection, greater postoperative pain, and wound dehiscence [19, 20].
The subgroup analysis between the normal/low preoperative mean MRP group and the high preoperative mean MRP group revealed that there were no statistically significant differences in postoperative complications or outcomes. Therefore, we hypothesize that a more complicated SSG procedure is not always necessary for hypotonic patients with chronic anal fissure in the presence of a fibrotic band. The less difficult minimal LIS method is sufficient and safe for patients with chronic anal fissure, hypotonicity, and fibrotic band. We believe that the presence of a fibrotic band is an important indication for surgery, regardless of the anal sphincter tone.
Eisenhammer [21] first reported internal sphincterotomy and proposed that spasms of the internal anal sphincter and elevated anal sphincter pressure lead to the development of chronic anal fissure. However, the relatively low percentage (16.5%) of patients with chronic anal fissure with a high mean MRP in our study implies that the pathogenesis of chronic anal fissure may be related to factors other than hypertonia. We believe that the fibrotic band is important in the pathogenesis of chronic anal fissure. Our theory is supported by a previous study by Shafik [22] that reported that pathologic changes occurring in chronic anal fissure result in the epithelization and formation of the fibrotic band; thus, anorectal bandotomy is required for the treatment of chronic anal fissure.
This study has several limitations. First, this was a retrospective and single-center study. Second, due to the use of a unique classification system to determine the study group and the retrospective nature of the study, there is a possibility of selection bias. Other limitations include the lack of postoperative anorectal manometry data and comparison with other treatment methods and the fact that procedures were performed by multiple surgeons. Multi-center studies are needed to validate the outcomes of this study.
In conclusion, minimal LIS is a safe and effective treatment option for chronic anal fissure, even in patients without anal sphincter hypertonia. Postoperative complications, especially incontinence and recurrence, are rare.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.