Mechanical Bowel Preparation and Prophylactic Antibiotic Administration in Colorectal Surgery: A Survey of the Current Status in Korea
Article information
Abstract
Purpose
The usefulness of mechanical bowel preparation (MBP) in colon surgery was recently challenged by many multicenter clinical trials and meta-analyses. The objectives of this study were to investigate current national opinions about MBP and prophylactic antibiotics (PA) and to provide preliminary data for developing future Korean guidelines for MBP and PA administration in colorectal surgery.
Methods
A questionnaire was mailed to 129 colorectal specialists. The questionnaires addressed the characteristics of the hospital, the MBP methods, and the uses of oral and intravenous antibiotics.
Results
A total of 73 questionnaires (56.6%) were returned. First, in regard to MBP methods, most surgeons (97.3%) used MBP for a mean of 1.36 days. Most surgeons (98.6%) implemented whole bowel irrigation and used polyethylene glycol (83.3%). Oral antibiotic use was indicated in over half (52.1%) of the responses, the average number of preoperative doses was three, and the mean time of administration was 24.2 hours prior to the operation. Finally, the majority of responders stated that they used intravenous antibiotics (95.9%). The responses demonstrated that second-generation cephalosporin-based regimens were most commonly prescribed, and 75% of the surgeons administered these regimens until three days after the operation.
Conclusion
The results indicate that most surgeons used MBP and intravenous antibiotics and that half of them administered oral PA in colorectal surgery preparations. The study recommends that the current Korean guidelines should be adapted to adequately reflect the medical status in Korea, to consider the medical environment of the various hospitals, and to establish more accurate and relevant guidelines.
INTRODUCTION
Preoperative mechanical bowel preparation (MBP) using whole bowel irrigation with or without retrograde enema and prophylactic antibiotics (PA) has traditionally been the essential preparatory step to reduce postoperative infectious complications. This preparation could prevent postoperative infection caused by fecal contamination and bacterial translocation during colorectal surgery. However, MBP has been reported to cause physical and psychological discomfort, dehydration, and electrolyte imbalance, can prove to be difficult for glucose control in diabetes patients, and can present challenges that are associated with an additional period of admission and fasting. Recent meta-analysis reports indicate that preoperative MBP should be omitted in colon surgery because it does not actually reduce the infectious complications [1, 2]. Although many clinical trials and meta-analyses have cautioned about the potential complications of MBP, these recommendations have not been incorporated into clinical practices. This could be attributed to differences in the designs and the clinical environments of Western and Korean hospitals.
Most studies have compared the results on the basis of open surgery; however, there has been a recent increase in the performance of laparoscopic surgery [3] in Korea. Therefore, it is important to consider the optimal preparation of the bowels in laparoscopic surgery. Recently published clinical trials have not included rectal surgeries; therefore, omitting MBP for colorectal surgery procedures remains controversial. In addition, the inappropriate application of antibiotics can lead to bacterial resistance, which will further increase the overall medical costs. The clinical practice guidelines and recommendations that address PA are also confusing because they recommend oral PA, parenteral PA or both [4]. This is further confounded by the spectrum of variable antibiotics, such as monotherapy or combination therapies, that require consideration of aerobic and anaerobic bacterial spectral coverage. Unfortunately, there is no basic information on daily or routine colorectal surgical practices in Korea. Therefore, this study was designed to survey the current status of MBP and PA use in Korea and to compare the results with recent guideline recommendations and the meta-analysis results from several randomized trials to ultimately provide preliminary data for future development of Korean guidelines on MBP and PA in colorectal surgery.
METHODS
From August 2009 to February 2010, survey questionnaires were developed at the Kyung Hee University Hospital at Gangdong (Appendix) and mailed to specialists who were listed in the membership directories of the Korean Society of Coloproctology. The survey targeted 112 colorectal specialists at 68 university hospitals and 17 specialists at eight colorectal specialty hospitals. The questionnaire consisted of 24 total questions related to hospital characteristics (3 items), MBP procedures (10 items), oral antibiotic therapies (5 items), and intravenous antibiotic therapies (6 items). The surgeons were asked to share their opinions about the usefulness of MBP and PA and about their current practices in colorectal surgery. Statistical processing of data was performed with the SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA), using the Student t-test for continuous variables and the chi-square method for nominal variables. A P-value less than 0.05 was considered to be statistically significant.
RESULTS
Hospital characteristics
A total of 73 specialists (56.6%) replied to the questionnaires that were mailed to 129 surgical specialists who worked at 76 different hospitals. The survey included private practices in two hospitals (2.8%) and academic practices in the other hospitals, with 22 of the surveys (30.1%) being from secondary referral hospitals and 49 (67.1%) from tertiary referral hospitals. Sixty-two of the responders (84.9%) practiced at teaching hospitals. The average numbers of colorectal surgeries that were performed in 2008 among the individual surgeons that were surveyed were as follows: two surgeons performed less than 50 surgeries (2.7%), 15 surgeons performed 50-100 surgeries (20.5%), 27 surgeons performed 100-200 surgeries (37.0%), nine surgeons performed 200-300 surgeries (12.3%), and 20 surgeons performed more than 300 surgeries (27.4%). Thirty-seven of the specialists (50.7%) performed their surgeries in operation rooms that were equipped with laminar flow equipment with high-efficiency particulate air (HEPA)-filters. The study found that nasogastric tubes were not routinely inserted.
Based on responses from 42 specialists (57.5%), only six specialists (8.2%) selectively inserted nasogastric tubes in cases with an obstructed bowel or in cases of elective laparoscopic surgery.
Preoperative MBP
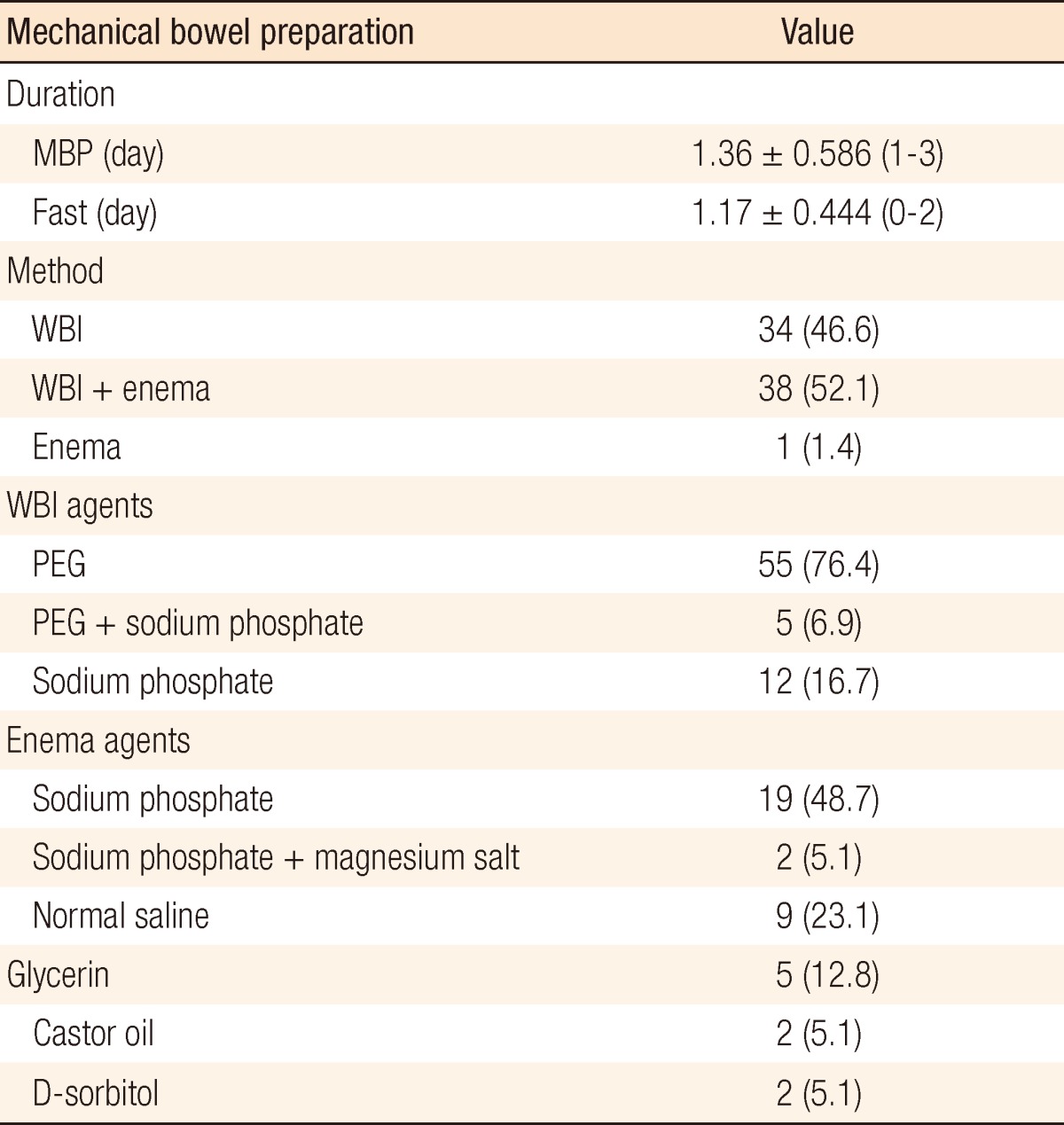
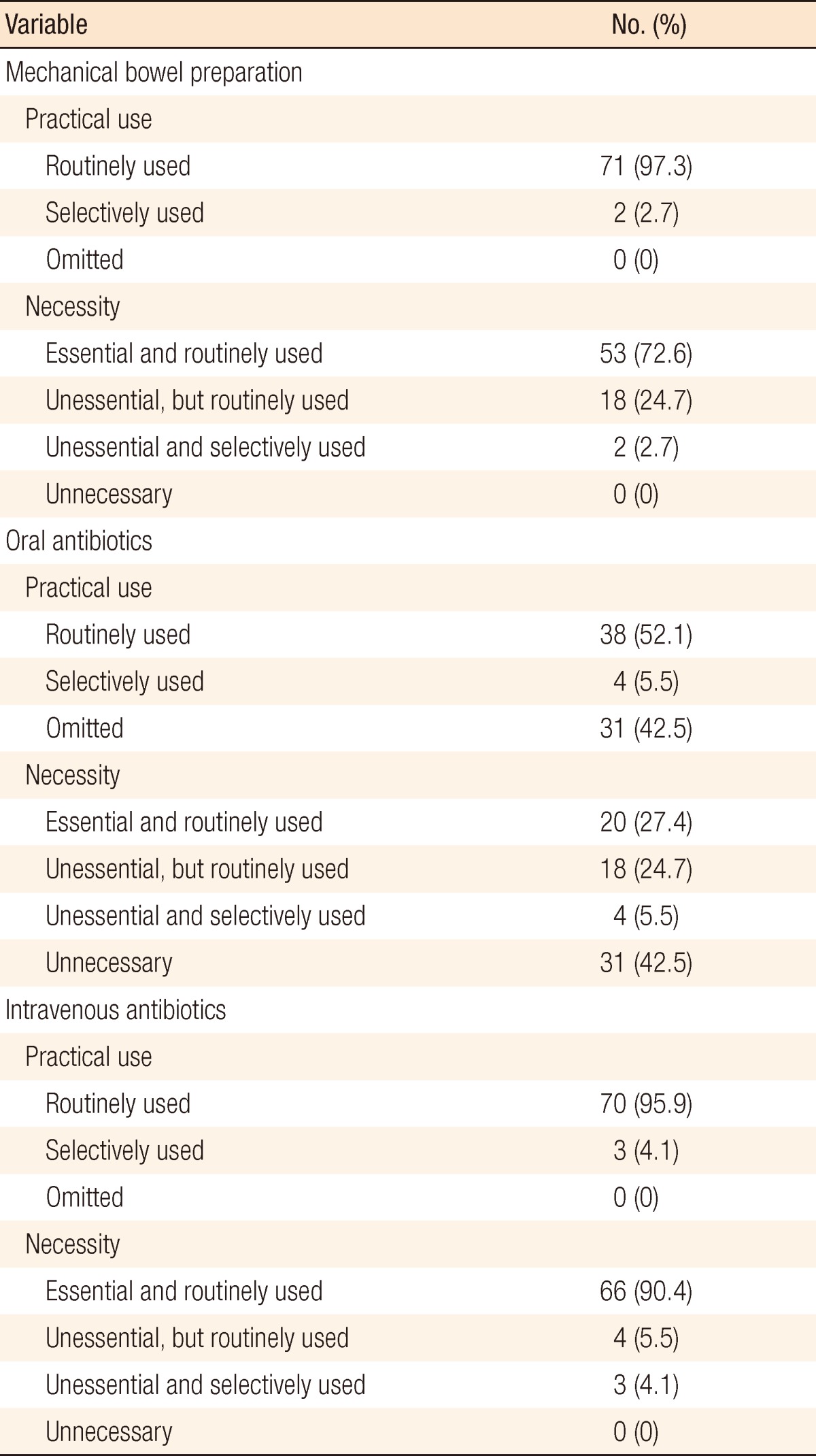
The majority of colorectal surgeons (97.3%) routinely performed preoperative MBP for elective colorectal surgery, and only two specialists selectively used MBP prior to a left colon and rectum surgery. However, the specialists indicated that they routinely used MBP, and 73% of the respondents agreed that MBP was a necessity (Table 1). The mean MBP duration was 1.4 days (±1.4 days; range, 1 to 3 days), and the mean duration of fasting was 1.2 days (± 0.4 days; range, 0 to 2 days). The MBP procedure included whole bowel irrigation and enema for 38 specialists (52.0%), whole bowel irrigation alone for 34 specialists (46.6%), and only retrograde enema for one respondent (1.4%). Polyethylene glycol (PEG) was used most frequently (83.3%) for the whole bowel irrigations, and of the responders, five specialists (6.9%) used sodium phosphate. In addition, sodium phosphate was most commonly used for retrograde enema cases (53.8%), and normal saline was used in 23.1% of the procedures (Table 2).
Practical use and necessity of mechanical bowel preparation, oral antibiotics, and intravenous antibiotics
Oral antibiotics
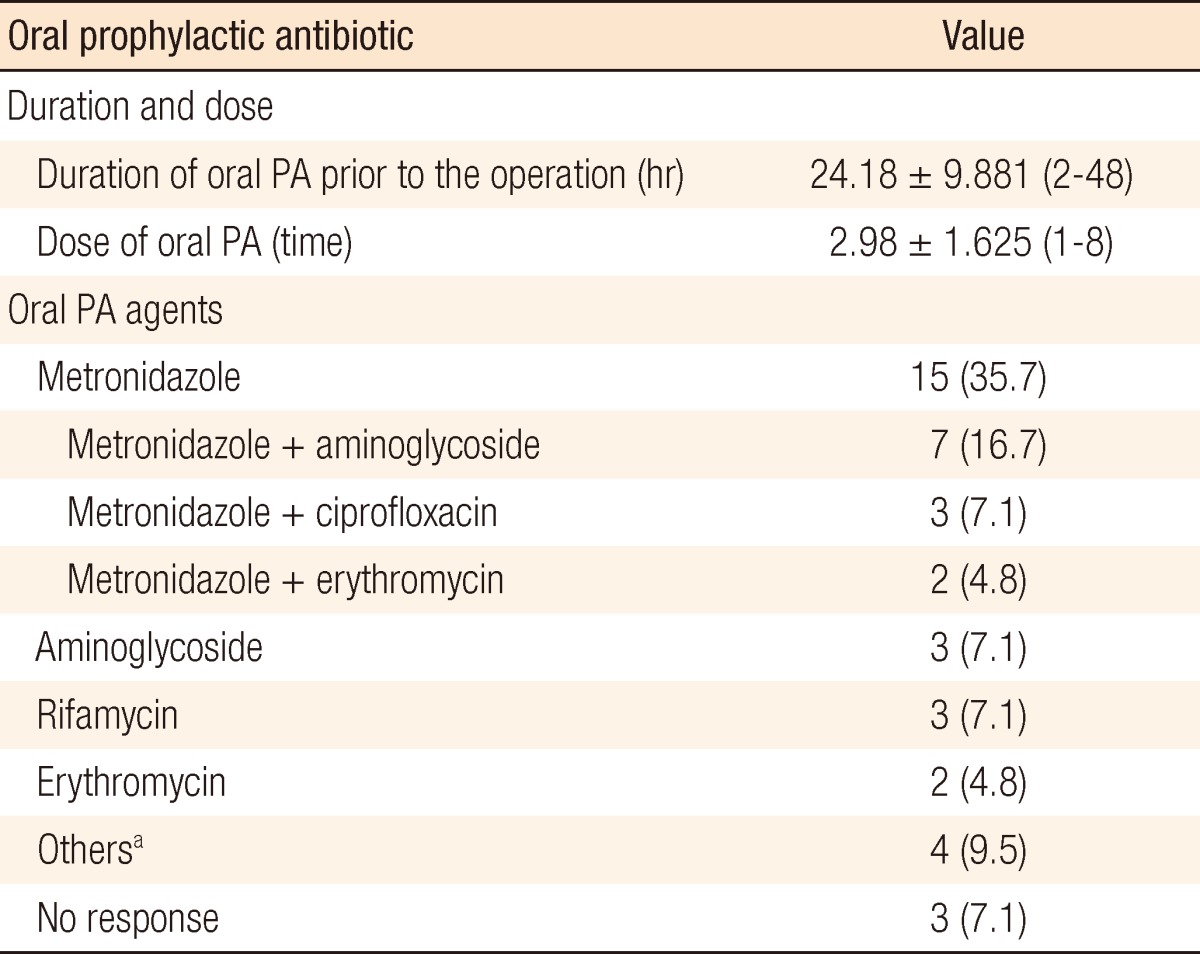
The survey indicated that 38 specialists (52.1%) routinely administered oral antibiotics, and only 20 of these specialists (27.4%) agreed that oral antibiotic prophylaxis (AP) was a necessity (Table 1). Four surgeons (5.5%) selectively used oral antibiotics when left colon or rectal surgery was planned and when they anticipated a poor MBP. The mean preoperative duration was 24.2 hours, and the mean number of oral antibiotic doses was three. A metronidazole-based regimen was the most frequently reported oral antimicrobial prophylaxis (n = 29, 69.0%) (Table 3).
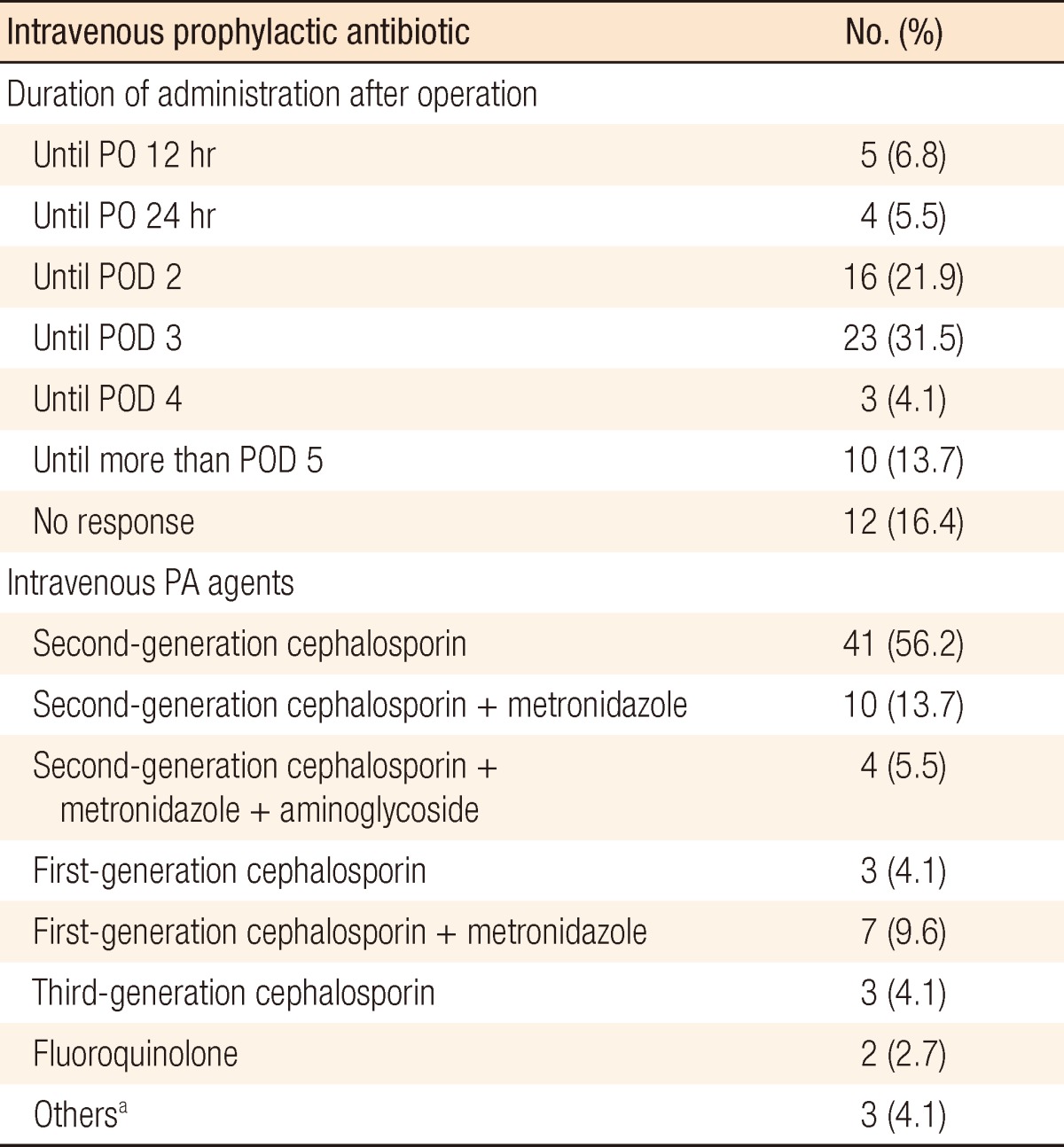
Intravenous AP
Most of the surgeons used intravenous PA in colorectal surgery (n = 70, 95.9%), and three surgeons (4.1%) selectively used intravenous PA in left colon and rectal surgery. Sixty-six surgeons (90.4%) indicated that intravenous prophylaxis was necessary, but four surgeons (5.5%) questioned the necessity of intravenous PA although they indicated that they routinely administered intravenous antibiotics (Table 1). Second-generation cephalosporin-based regimens were the most commonly prescribed (n=55, 74.3%), and about 75% of the respondents used antibiotic therapies until three days after the operation (Table 4).
DISCUSSION
Surgical site infection accounts for 13.9% to 16.0% of all nosocomial infections [5]. Because of the possibility of fecal contamination, the heavy microbial burden, and the subsequently high risk of surgical site infection in colorectal surgery, patients are usually required to undergo prolonged fasting, a preoperative MBP, and antimicrobial prophylaxis. Bowel cleansing for colorectal surgery is typically composed of either a preoperative MBP using whole bowel irrigation with or without a retrograde enema, preoperative oral antibiotic administration against the colonic aerobic or anaerobic flora, or perioperative intravenous antibiotic administration [6].
A previous study proposed that preoperative MBPs could reduce the occurrence of intraperitoneal and wound infections, prevent anastomotic leakage that results from the passage of hard feces, and improve bowel manipulation [7]. However, MBP also causes adverse effects, such as dehydration or electrolyte imbalance, as well as general patient discomfort. Additionally, an incomplete bowel preparation can progress to bowel edema and induce liquid bowel contents, which can make it more difficult to manipulate the bowel during surgery. In addition, an MBP could prolong the duration of hospitalization and increase health-care related costs. Bucher et al. [8] demonstrated in a randomized trial that bowel wall alterations, such as loss of superficial mucus and epithelial cells and inflammatory changes such as lymphocyte and polymorphonuclear cell infiltration, were more prevalent after a preoperative MBP that used PEG.
Several prospective randomized trials investigated the necessity of MBP and reported that preoperative MBP was unnecessary or even harmful to the patient [9-13]. Furthermore, a meta-analysis by Slim et al. [1], which included prospective randomized trials, concluded that MBP using PEG should not be performed prior to elective colorectal surgery. The authors of another meta-analysis that analyzed the results of recently reported trials [14-20] concluded that all types of MBP should be abandoned before colonic surgery, but that the role of the MBP in rectal surgery remained to be evaluated [2]. Based on these studies, the Cochrane Database Systematic Review of 2009 announced that prophylactic MBP prior to colorectal surgery had not proven to be valuable [21].
PA had previously been administrated orally or intravenously in order to prevent surgical site infection in colorectal surgery patients. In the Cochrane Database Systematic Review of 2009, a meta-analysis demonstrated that PA significantly reduced postoperative wound infection and that aerobic microbial coverage and additional anaerobic microbial coverage significantly improved the rates of wound infection, although long-term prophylaxis was not found to be beneficial for reducing wound infection rates [22]. The guidelines from the Surgical Infection Prevention Guideline Writers Workgroup [23] and the Hospital Infections Control Practices Advisory Committee [24] in the United States (US) recommend the following courses of action: 1) nonabsorbable oral antibiotics should be administrated in divided doses that are initiated no more than 18 to 24 hours before the operation, 2) intravenous antibiotics should begin when a bactericidal concentration in the serum and tissue is reached upon making the incision, 3) the therapeutic concentration should be maintained during and for a few hours after the operation, and 4) intravenous antibiotics should be discontinued within 24 hours following the operation.
However, as this survey demonstrated, in practice, many surgeons actually administer intravenous antibiotics for several days after an operation because of the fear of fecal contamination, and these routine medical practices may cause problems such as the emergence of resistant bacteria and increasing healthcare-related costs. In this study, only 14.8% of the specialists answered that IV antibiotics were discontinued within 24 hours after the operation. In addition, in 2007, the Korean Society of Coloproctology recommended that combination regimens of first-generation antibiotics such as cephalosporin and metronidazole or single regimens of second- or third-generation cephalosporin or the addition of metronidazole should be administered and discontinued within five days after elective colorectal surgery [25]. However, this recommendation was not based on the results of clinical trials, but instead on the consensus of practicing surgeons. Therefore, new guidelines based on clinical trials that analyze the combinations and the duration of PA and that reflect Korean medical environments are necessary. Due to the high cost of medical devices and medical supplies, the majority of Korean hospitals use reusable instruments and drapes. In addition, the operating-room environment generally does not meet all of the recommendations; for example, only 50% of the operating rooms are equipped with laminar flow and HEPA filters. These medical environments may contribute to the administration of and the recommendation for prolonged use of intravenous PA.
The intravenous antibiotic combinations were also variable, based on the responses to the survey. Although the US Food and Drug Administration approved second-generation cephalosporin monotherapy or a combination of first-generation cephalosporin with metronidazole or ampicillin-sulbactam for AP in colorectal surgery, current practices in Korea indicate that different combinations of antibiotics are being administered. About one-third of the colorectal specialists use their own prescriptions, such as third-generation cephalosporin and fluoroquinolone treatment. A recently published study by Jeong et al. [26] reported that second-generation cephalosporin alone was as effective as a triple regimen composed of first-generation cephalosporin, metronidazole, and aminoglycoside for elective colorectal cancer surgery prophylaxis.
This study was conducted to survey the current applications of MPB procedures and AP for Korean colorectal surgery patients and to provide basic information for the development of revised Korean guidelines for AP and MBP in elective colorectal surgery. Our results suggest that individual MBP practice and AP are not based on the current guidelines or on the level of the infection-preventing system at each hospital, but are instead based on the customary principle of each institute or the preferences of the specialists.
A survey of 1,295 members of the American Society of Colon and Rectal Surgeon in the United States in 2003 indicated that most respondents routinely used MBP (99%) and intravenous antibiotics (98%) in colorectal surgery [27]. These results are comparable to the results of the present study. However, oral antibiotics were routinely administered in 75% of the responses and were omitted in 13% of the responses, which showed a higher utilization of these techniques in the US than in Korea. In regard to the recommendation of bowel cleansing, 90% of the respondents agreed that the MBP procedure was essential, and 49% agreed that oral antibiotics were a necessity. These responses indicate a higher level of awareness in the US than in Korea. However, these results were reported prior to a recent meta-analysis of several clinical trials; therefore, a direct comparison between the two studies would be inappropriate.
Preparation for elective colorectal surgery can be challenging, and it may be difficult for a physician to determine the appropriate level of processing for bowel preparation or the best treatment to reduce surgical site infections while minimizing patient discomfort. Therefore, when creating guidelines for surgical and postoperative procedures, it is important to consider the specific medical and surgical environments that are available to the medical communities throughout Korea. In addition, national guidelines should not be based on medical practices or the results of studies from Western countries, where the medical and surgical environments may be different. This study recommends that future guidelines should be designed based on a consideration of the healthcare environments and the diverse medical institutes in Korea. The results of this study can be used as preliminary data for the development of future Korean guidelines that address the administration of PA and the use of MBP procedures for elective colorectal surgery.
In conclusion, the results of our survey indicate that the majority of colorectal specialists use MPB for preoperative bowel cleansing and administer prophylactic intravenous antibiotics to their patients. Half of the specialists also administer oral antibiotics for colorectal surgery cases. This survey reflects the current practices of colorectal specialists in Korea. From this first national survey, we found distinct differences among Korean surgeons between their preferred bowel preparation method and the duration of PA administration and the guidelines recommended in the literature. If Korean guidelines are to be established for bowel preparation and use of PA, further prospective, randomized trials should be conducted in Korea.
ACKNOWLEDGMENTS
This work was supported by the Korean Academy of Medical Sciences (Investigation of Medical Statistics) in 2009.
Notes
This article was presented at the 62nd Annual Congress of the Korean Surgical Society in 2010.
No potential conflict of interest relevant to this article was reported.
Appendices
Appendix
Mechanical bowel preparation and prophylactic antibiotics questionnaire