Pneumoretroperitoneum After Procedure for Prolapsed Hemorrhoid
Article information
Abstract
Procedure for prolapsed hemorrhoid (PPH) is well recognized alternative to the traditional hemorrhoidectomy, and is associated with reduced pain and earlier return to normal activity. Over the past decade, there have been reports of severe life-threatening complications after a PPH, although the incidence is very low. Rectal perforation due to staple-line dehiscence is one of the serious complications that can cause severe pelvic sepsis or a pneumoretroperitoneum. Here, the first Korean case of a pneumoretroperitoneum due to staple-line dehiscence is described.
INTRODUCTION
Hemorrhoids are common, and a significant proportion of patients with hemorrhoids experience symptoms such as bleeding, pain and prolapse. Procedure for prolapsed hemorrhoid (PPH) is a safe and effective technique that has been applied for the treatment of internal hemorrhoids, and it has had a high success and a low complication rate [1]. Complications after PPH, when they occur, are mostly minor and may include bleeding, staple-line stenosis, persistent pain, external hemorrhoid thrombosis, and/or urinary retention [1]. However, rare, but potentially life-threatening, complications like pelvic sepsis, massive bleeding and peritonitis have been reported [2, 3]. A case of rectal perforation with massive a pneumoretroperitoneum due to staple-line dehiscence after PPH is described. No case of a pneumoretroperitoneum after PPH has been reported before, to the best of our knowledge, in Korea.
CASE REPORT
A previously healthy 27-year-old female who had a grade-3 prolapsing hemorrhoid was treated with PPH at a local private hospital. She was discharged on the second postoperative day without any specific symptoms. She visited the Emergency Department of our institution on the evening of the discharge day due to a sudden onset of abdominal pain and fullness. Physical examination showed a diffuse abdominal tenderness, but the degree was not as severe as that seen in a typical case of peritonitis. On rectal digital examination, the staple line was noted at approximately 4 cm above the anal verge, and the defect was located at the right side of patient. There was no bleeding evidence in either the patient's history or on examination. Vital signs were stable except for a mild fever (37.5℃). The white blood cell count was 13 × 106/mL. A plain abdominal radiograph and a computed tomography (CT) scan showed extensive retroperitoneal gas (Figs. 1 and 2). Air bubbles were also found at the subcutaneous layer of the anterior abdominal wall on the CT scan. A laparoscopic evaluation was performed at 55 hours after the original surgery. Exploration of the peritoneal cavity and the retroperitoneal space revealed no necrosis, abscess or fecal material. The retro-rectal tissue, however, was markedly edematous and vascular. A closed suction drain was placed at the retroperitoneal space, and a loop sigmoid colostomy was created.
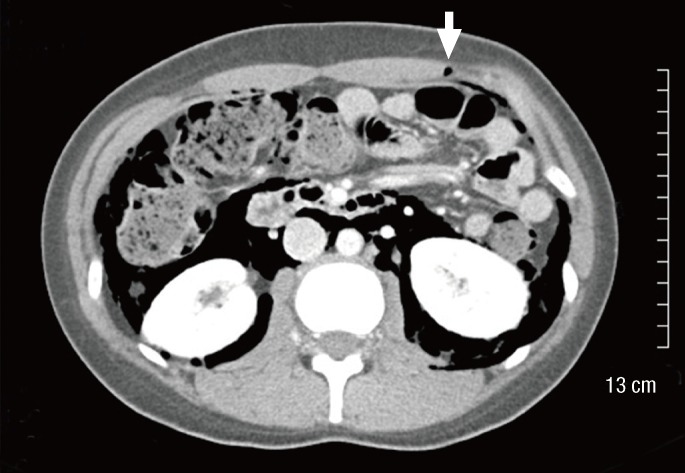
A computed tomographic image shows an extensive retroperitoneal gas. An air bobble is also seen in the anterior abdominal wall (arrow).
The rectal staple line was inspected after the abdominal procedure. Partial staple-line dehiscence, which was consistent with the preoperative digital examination, was noted at the right side of the patient (Fig. 3). The defect was closed with 4-0 vicryl after massive irrigation. An overstitching was done throughout the staple line to prevent possible future dehiscence. The postoperative course was uneventful, and oral feeding was resumed on the second postoperative day. At the 2-month follow-up, a gastrografin enema showed the absence of leaks, and the colostomy was closed. During follow-up, she has had no residual problems, including staple-line stenosis.
DISCUSSION
PPH was first proposed by Longo in 1993 [4] and has become increasingly popular over the past 10 years for the treatment of hemorrhoids. It is easy and quick to perform, and it has additional advantages, such as less postoperative pain and earlier return to normal activity. In addition it seems to respond to pathogenesis of the disease in that it interrupts the superior hemorrhoidal arterial supply and fixes the hemorrhoidal tissue in the anal canal.
Recently some studies have questioned the efficiency and the safety of PPH. Systemic reviews showed that the recurrence rate after PPH is higher than that after a manual hemorrhoidectomy [5, 6]. The Italian Society of Colo-Rectal surgery suggested strict application of PPH to only third-degree hemorrhoids [7]. For second-degree hemorrhoids, lesser invasive techniques, including rubber banding or Doppler, were recommended. For fourth-degree and thrombosed piles, most studies have reported high complication and recurrence rates after PPH [8, 9]. A survey showed a decreasing trend of PPH in Italy where the PPH was initiated [10].
PPH is by no means a risk-free procedure. The overall complication rate has been reported to be similar between PPH and conventional surgery [11, 12]. Apart from minor complications, which are equally reported after a manual hemorrhoidectomy, unusual and severe complications, e.g., rectal perforations, complete rectal obstructions, rectovaginal fistulae, have been reported following PPH [13]. Among them, rectal perforation is extremely rare. For example, an analysis of 25 randomized clinical trials including 1,918 procedures found no case of rectal perforation [1]. Ng et al. [14] reported the frequency of life-threatening septic complications resulting from rectal perforation to be less than 0.1 percent in their large scale series. However, rectal perforations may be underreported. Pescatori and Gagliardi [10] found that 38 cases of rectal perforation or staple-line dehiscence after PPH were listed on the U.S. Food and Drug Administration (FDA) website, but none of those cases had been reported in the scientific literature.
Rectal perforation is a potentially life-threatening complication that often requires a temporary or even permanent fecal diversion. Of the 38 patients listed on the FDA website as having a rectal perforation or staple-line dehiscence after PPH, 19 cases were severe enough to require an abdominal surgery, and 13 patients had a fecal diversion. Interestingly, the perforation sites were often found above the staple line [3, 13]. The possible causes are a peritoneal reflection being too low or a purse string suture being placed too high; thus, the peritoneal reflection appears to have been incorrectly incorporated into the purse-string suture. The patients with an enterocele or a prolapsed Douglas pouch due to a previous hysterectomy were regarded to be particularly vulnerable to these kinds of injuries.
The dehiscence of the staple line is a common cause of rectal perforation at PPH. In a recent review, four of the seven patients with severe pelvic sepsis also presented with anastomotic dehiscence [2]. A pneumoretroperitoneum after PPH is extremely rare. Only several cases have been reported in the literature. The presence of air in the retroperitoneal space may be due either to filtration of air through the staple-line defect or to leakage of bacterial content, leading to pelvic sepsis. An instant fecal diversion was done in the present case because the rectal staple-line dehiscence was evident, and the patient showed signs of peritonitis. However, in one report, the pneumoretroperitoneum was treated conservatively with antibiotics and delayed oral intake in a silent case with an intact staple line [15]. The exact cause of staple-line dehiscence is unclear, although many possible mechanisms have been suggested. Staple-line dehiscence is often accompanied by extensive hemorrhage [13]. Other suspected causes include a malfunctioning stapler, surgeon inexperience, and deep placement of a purse-string suture. If this complication is to be prevented, any staple-line hemorrhage should be treated at an early stage, the staple line should be checked at the end of the operation, and bleeding points should be ligated rather than treated with simple electrocautery. Purse-string sutures must be placed within the submucosal plane, as advocated by Longo [4], to prevent full thickness resection. In addition, any case with a true rectal prolapse must be excluded.
As seen in the present case, rectal perforation due to anastomotic dehiscence is possible at PPH although it is extremely rare. The surgeon has to be alert to this complication, and early diagnosis and timely treatment are mandatory.
Notes
No potential conflict of interest relevant to this article was reported.

