Single-Port Laparoscopic Interval Appendectomy for Perforated Appendicitis With a Periappendiceal Abscess
Article information
Abstract
Purpose
Nonoperative management followed by an interval appendectomy is a commonly used approach for treating patients with perforated appendicitis with abscess formation. As minimally-invasive surgery has developed, single-port laparoscopic surgery (SPLS) is increasingly being used to treat many conditions. We report our initial experience with this procedure using a multichannel single-port.
Methods
The study included 25 adults who underwent a single-port laparoscopic interval appendectomy for perforated appendicitis with periappendiceal abscess by using a single-port with or without needlescopic grasper between June 2014 and January 2016.
Results
Of the 25 patients, 9 (36%) required percutaneous drainage for a median of 7 days (5–14 days) after insertion, and 3 (12%) required conversion to reduced-port laparoscopic surgery with a 5-mm port insertion because of severe adhesions to adjacent organs. Of 22 patients undergoing SPLS, 13 underwent pure SPLS (52.0%) whereas 9 patients underwent SPLS with a 2-mm needle instrument (36.0%). Median operation time was 70 minutes (30–155 minutes), and a drainage tube was placed in 9 patients (36.0%). Median total length of incision was 2.5 cm (2.0–3.0 cm), and median time to soft diet initiation and length of stay in the hospital were 2 days (0–5 days) and 3 days (1–7 days), respectively. Two patients (8.0%) developed postoperative complications: 1 wound site bleeding and 1 surgical site infection.
Conclusion
Conservative management followed by a single-port laparoscopic interval appendectomy using a multichannel single-port appears feasible and safe for treating patients with acute perforated appendicitis with periappendiceal abscess.
INTRODUCTION
A periappendiceal abscess (PAA), or phlegmon, is found in about 3.8% of patients with appendicitis [123]. However, an immediate appendectomy for acute appendicitis with PAA can result in excessive tissue manipulation to detach adhesions, which leads to inflammatory reactions and damage to adjacent organs [14]. Since Murphy [5] emphasized the necessity of an interval appendectomy after a drainage procedure for treating patients with PAA, nonoperative management followed by an interval appendectomy has become one of the preferred protocols for the treatment of patients with abscessed perforated appendicitis.
The laparoscopic appendectomy, first described by Semm [6] in 1983, has been rapidly accepted as an adequate option for treating patients with uncomplicated appendicitis as it shows several advantages over the open approach. Minimally-invasive surgery has rapidly developed in recent years, minimizing surgical trauma and improving cosmetic outcomes, which have evolved to become current topics of active discussion. These concepts have led to the development of single-port laparoscopic surgery (SPLS) for the treatment of patients with a variety of conditions.
Recent reports have shown that patients with acute appendicitis may undergo SPLS safely [78]. Advances in the development of laparoscopic instruments and accumulated physician experience with SPLS for the treatment of patients with appendicitis have led to this procedure being used more frequently in patients with complicated appendicitis [9]. However, the application of the SPLS to patients with a PAA has been reported only in pediatric patients, and its safety and its feasibility for use in adult patients have not yet been determined [10]. The aim of this study is to describe our initial experience with a single-port laparoscopic interval appendectomy to treat adult patients with PAA and to assess its safety and the feasibility of its use for treating adult patients.
METHODS
A total of 345 patients underwent a laparoscopic appendectomy for acute appendicitis at Keimyung University Dongsan Medical Center, Daegu, Korea, between June 2014 and January 2016. Of these 345 patients, 320 (92.8%) underwent an immediate laparoscopic appendectomy, including 92 (28.8%) single-port approaches and 228 (71.2%) multiport approaches. The remaining 25 (7.2%) consecutive patients with PAA who underwent a single-port laparoscopic interval appendectomy using the Glove Port (Sejong Medical, Paju, Korea) with or without a Mini-Lap needlescopic grasper (Stryker Endoscopy, San Jose, CA, USA) constituted the study group. All cases were performed by a single surgeon who was a colorectal specialist with experience in 6 cases of using SPLS for treating patients with acute appendicitis. The prospectively collected data included patients' demographics, duration of antibiotic therapy used for conservative management, number of patients requiring percutaneous drainage (PCD) insertion, duration of PCD, and inflammatory laboratory findings. Details of operative outcomes included the types of operation and appendicitis, number of patients who underwent conversion to reduced-port laparoscopic or open surgery, total operative time, number of patients with periappendiceal fluid collection, diameter and length of the resected appendix, number of patients with drain placement, and total length of incision. Postoperative data included the time to diet initiation, duration of hospital stay, postoperative complications, number of patients needing readmission, and histology reports. In the present study, we included patients who underwent SPLS using a 2-mm needle instrument in the SPLS group. Conversion to open surgery was defined as interruption of the laparoscopic approach followed by a laparotomy. Conversion to reduced-port laparoscopic surgery or multiport laparoscopic surgery (MPLS) was defined as the requirement for an additional port or more than two additional port placements, respectively, at any time to complete the entire surgical procedure.
Patients with PAA were treated intravenously with a combination of two antibiotics (ceftriaxone and metronidazole) with or without PCD insertion. An associated large abscess (>4 cm) was drained percutaneously if anatomically applicable. Patients were discharged when afebrile, white blood cell count and C-reactive protein (CRP) had reverted to nearly normal, movement with minimal pain was possible, and a soft diet was tolerated. Patients underwent colonoscopy and an abdominal computed tomography scan 4 weeks after their acute illness to exclude colitis or neoplasms, and 6 to 8 weeks after discharge, an interval appendectomy was performed. Data are expressed as medians with range, and statistical analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
All surgical procedures were carried out under general anesthesia with the patient in the supine position. Cefuroxime (1.0 g) was administered intravenously for systemic antibiotic prophylaxis at the time of general anesthesia induction. The patient was placed in the supine position at 30° and tilted right-side down at an angle of 10°–15°. After the base of the umbilical stalk had been everted by using two penetrating towel clamps placed on either side of the midline, a single 2.0-cm vertical incision was made through the umbilical skin (Fig. 1A). The subcutaneous tissue was dissected toward the linea alba, which was incised vertically, and the peritoneum was opened. A single-port was placed in the abdominal cavity through the umbilical incision (Fig. 1B). After pneumoperitoneum with insufflation of CO2 up to 12 mmHg had been achieved, a 5-mm diameter telescope with fiber-optic light transmission and a 30° angled view was inserted through the 5-mm channel of the single-port. In this study, no specialized instruments, either bent or flexible (Fig. 1C), were used. The laparoscope was introduced through the port, and all 4 quadrants were inspected. When adequate and timely counter-traction was needed, a 2-mm needle instrument was inserted into the right lower quadrant under direct vision (Fig. 1D, E). The mesoappendix was divided by the sequential use of a Covidien Sonicision (Covidien, Mansfield, MA, USA) device. The appendiceal base was ligated by the application of two Vicryl endo-loops (Sejong Medical) or the Endo-GIA stapler (Covidien) (Fig. 1F). The appendix was removed through the umbilical incision and placed into the sterile bag component of the single-port, after which thorough irrigation of the periappendiceal and the subhepatic areas with normal saline was performed. Following removal of the single-port, the umbilical fascia was closed with 2-0 Vicryl sutures, and the subcutaneous layer was sutured with 4-0 Monosyn (B. Braun Aesculap AG & Co KG, Tuttlingen, Germany) buried interrupted sutures. An umbilical dressing consisting of a small piece of gauze packed into the umbilicus was applied and covered with a compressive dressing.

Single-port laparoscopic interval appendectomy with a needle instrument for appendicitis with abscess. (A) A single 1.2-cm vertical incision was made through the umbilical skin. (B) A multichannel single-port was inserted through the umbilical incision. (C) The laparoscope was introduced through the single-port, revealing an inflamed appendix with a severe adhesion between appendix and omentum. (D) A mini-laparoscopic instrument was inserted into the right lower abdomen. (E) Dissection with adequate and timely counter-traction. (F) The appendiceal base was ligated with an endoscopic linear stapler.
RESULTS
The median age of the 25 patients in the study group was 62 years (range, 19–82 years) and included 12 women (48.0%) and 13 men (52.0%) (Table 1); the mean body mass index was 24.4 kg/m2 (range, 17.5–31.3 kg/m2). Eleven patients (44.0%) were classified into class I, 11 (44.0%) into class II, and 3 (12.0%) into class III according to their physical status score (American Society of Anesthesiologists classification). The median duration of symptoms prior to diagnosis was 7 days (range, 2–26 days), and the median interval between discharge from conservative management and the interval appendectomy was 7.0 weeks (range, 3.4–10.7 weeks).
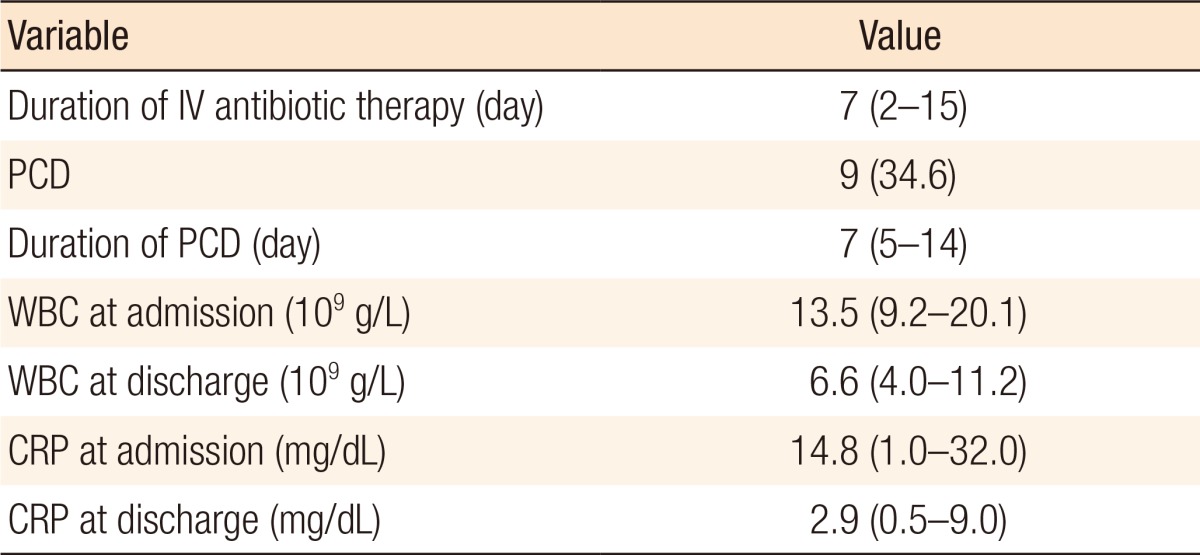
The median duration of intravenous antibiotic therapy during conservative management was 7 days (range, 2–15 days) (Table 2). Nine patients (36.0%) required the insertion of a PCD during initial treatment, with a median of 7 days (range, 5–14 days) between insertion and removal. Laboratory test results on admission showed a median white blood cell count of 13.5 × 109 g/L (range, 9.2–20.1 × 109 g/L) (normal values: 4.0–10.50 × 109 g/L) and a median CRP level of 14.8 mg/L (range, 1.0–32.0 mg/L) (normal values: 0–4.9 mg/L). Laboratory test results at discharge showed a white blood cell count of 6.6 × 109 g/L (range, 4.0–11.2 × 109 g/L) and a CRP level of 2.9 mg/L (range, 0.5–9.0 mg/L).
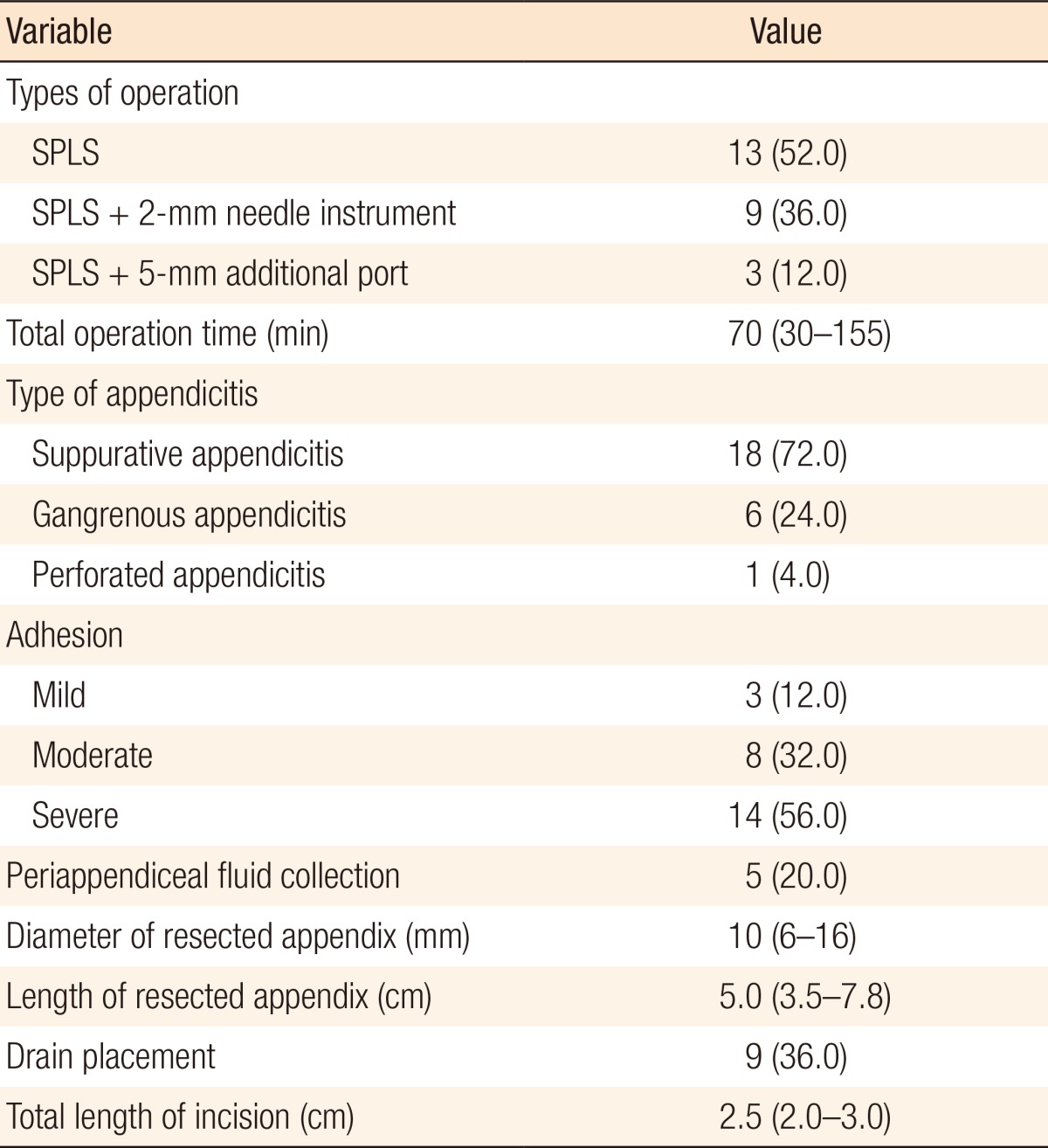
All 25 patients underwent technically successful procedures without the need for conversion to open surgery (Table 3). However, 3 patients (12.0%) required conversion to reduced-port laparoscopic surgery with insertion of a 5-mm port because of severe adhesions to the small bowel, omentum, or abdominal wall. Of the 22 patients undergoing SPLS, 13 patients underwent pure SPLS (59.0%) whereas 9 patients (36.0%) underwent SPLS with a 2-mm needle instrument. The median total operation time for all 25 patients was 70 minutes (range, 30–155 minutes). Of the 25 total patients, 18 (72.0%), 6 (24.0%), and 1 patient (4.0%) developed suppurative, gangrenous, and perforated appendicitis, respectively. In addition, intraoperative findings included 14 (56.0%) and 5 patients (20.0%) with severe adhesions to adjacent organs and periappendiceal fluid collection, respectively. The median diameter and length of the resected appendix were 10 mm (range, 6–16 mm) and 5.0 cm (range, 3.5–7.8 cm), respectively. A drain was placed in the pelvic cavity in 9 patients (36.0%), and the median total length of incision was 2.5 cm (range, 2.0–3.0 cm).
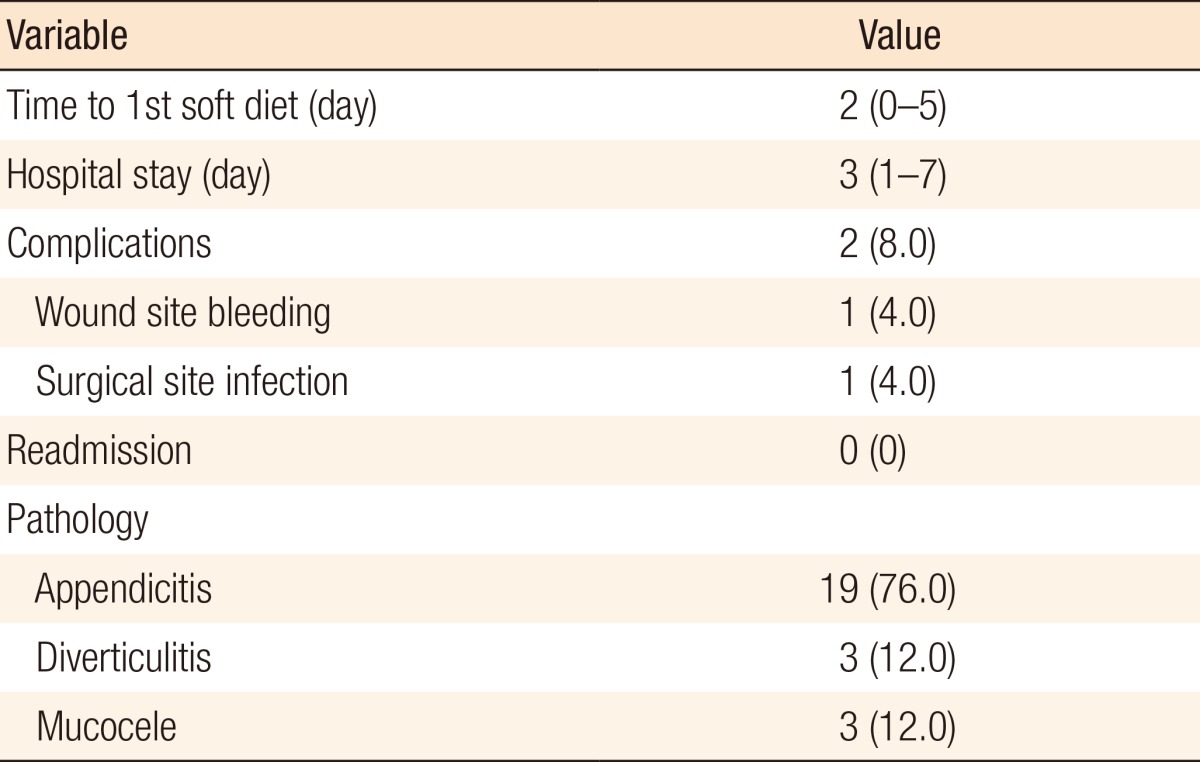
The median times to initiation of a soft diet and length of stay were 2 days (range, 0–5 days) and 3 days (range, 1–7 days), respectively (Table 4). Two patients (8.0%) developed postoperative complications, including one wound site bleeding and one surgical site infection. None of the patients were readmitted. Final pathologic findings demonstrated appendicitis, mucocele with low grade dysplasia, and diverticulitis in 19 (76.0%), 3 (12.0%), and 3 patients (12.0%), respectively.
DISCUSSION
Although the need for an interval appendectomy is controversial, with some studies suggesting that an interval appendectomy is unnecessary and that nonoperative management has a cost advantage over a routine interval appendectomy after initial recovery with conservative management for perforated appendicitis [111213], traditionally, an interval appendectomy has been recommended for 3 patients 6 to 8 weeks after presentation for 2 primary reasons: to prevent recurrence of appendicitis and to exclude neoplasms such as carcinoids, adenocarcinomas, mucinous cystadenomas, and cystadenocarcinomas [141516].
In this study, 2 minimally-invasive approaches, (1) nonoperative management followed by an interval appendectomy and (2) SPLS, were integrated into the management of patients with appendicitis and PAA. The advantage of an interval appendectomy with or without PCD is that the surgery is performed once peritoneal contamination has been resolved, potentially resulting in fewer postoperative complications, including bowel obstruction, wound infection, fistula formation, intra-abdominal abscess, and bowel injury due to difficult dissection. The potential advantages of SPLS are less postoperative incisional pain, improved cosmetic outcome, fewer wound complications, and lower risk of hemorrhage, incisional hernia, and organ injury.
The present study demonstrates that an interval appendectomy using a single-port with a multi-channel system can be performed with technical efficiency and favorable short-term outcomes. Perioperative outcomes, including median time to soft diet initiation and mean hospital stay of 2 and 3 days, respectively, were comparable to those for multiport laparoscopic surgery (MPLS) for PAA [1718]. One of the controversies surrounding SPLS is the increased operation time when compared with conventional techniques. In particular, some have reported increased SPLS operation times for patients with uncomplicated appendicitis compared with those of MPLS [71920]. Moreover, a single-port laparoscopic interval appendectomy for PAA is a more technically demanding procedure than a laparoscopic appendectomy for uncomplicated appendicitis, and available data from studies comparing SPLS and MPLS for treating patients with a PAA are extremely rare. A few previous studies on MPLS for treating a PAA in adult and pediatric patients reported average operatives time of 58 and 55 minutes, respectively [1821]. In the present study, operative times ranged from 30 to 155 minutes, with a median of 70 minutes. These slightly longer operative times may originate from patients for whom the intervention took longer as a result of severe adhesions to adjacent organs (56.0%) and or periappendiceal fluid collection (20.0%).
In the current study, 3 patients (12.0%) required 5-mm additional port insertion because of difficulties encountered in dissecting severe adhesions. In these patients, the laparoscope was introduced through the single-port, revealing an inflamed gangrenous appendix with a PAA and severe adhesion between the cecum and the small bowel mesentery. Soon after laparoscopic exploration, we decided to add a 5-mm port to enable safe and efficient continuation of the laparoscopic approach. One of those patients needed intracorporeal suturing due to a serosal injury to the cecum. The operation was completed safely without the need for conversion to open surgery, and the total operation time was 155 minutes. Muensterer et al. [22] reported that 3 of 9 pediatric patients (33.3%) required an additional port insertion during SPLS for appendicitis with a PAA, and Ohno [10] demonstrated that an accessory port was necessary in 8 of 21 pediatric patients (38.1%), 2 of whom successfully underwent laparoscopic surgery while the remaining six were converted to open appendectomy. It is important to keep in mind that the use of an additional port is not a SPLS failure. In fact, a single-port with an additional port laparoscopic appendectomy for complicated appendicitis reduces the risk of collision between laparoscopic instruments and the camera, allows adequate and timely traction, and facilitates pelvic drain placement through the additional port incision.
Mini-laparoscopic instruments with outer diameters of 2 mm allowing direct percutaneous placement into the abdomen can be used as a modified single-port laparoscopic surgery. In this study, when adequate and timely countertraction was needed because of severe adhesions or inflammation, a mini-laparoscopic instrument was inserted into the abdomen (usually into the right lower abdomen) to hold the appendix or adjacent structures; this occurred in nine patients. Some studies have reported on a mini-laparoscopic appendectomy using three incisions, including a 5- or a 10-mm conventional port, for treating patients with acute appendicitis [2324]. We think that a single-port with a mini-laparoscopic instrument technique can be used as a modified single-port laparoscopic approach for treating patients with appendiceal disease because this technique can result in cosmetic advantages similar to those of SPLS and in better ergonomics than pure SPLS in complicated cases (Fig. 2).
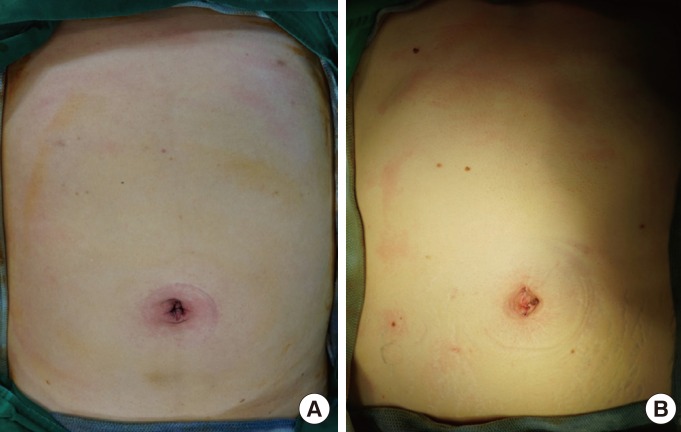
Postoperative scar: (A) pure single-port laparoscopic surgery (SPLS) and (B) SPLS with a 2-mm needle instrument.
SPLS has its own unique challenges, including the relative loss of triangulation due to the straight instruments being parallel to the laparoscope, clashing of instruments, and the steep learning curve needed for mastering the procedure. However, in the current study, the problems anticipated for the loss of triangulation were overcome by using a mini-laparoscopic instrument in complicated cases. To overcome the technical challenges associated with the use of single-port or reduced-port laparoscopic surgery, Lasheen et al. [25] used a spiral needle to facilitate the procedure in two-port surgery for appendectomy, and Padilla et al. [26] reported SPLS using a magnet-assisted single trocar for adequate exposure. Moreover, Ates et al. [27] introduced a percutaneously-inserted suture from the right lower quadrant into the peritoneal cavity during SPLS for an appendectomy.
Our study has several limitations including its retrospective nature, small size of the study, and lack of data on pain or cosmesis for single-port versus multi-port surgery.
In conclusion, conservative management followed by a single-port laparoscopic interval appendectomy using a multichannel single-port is feasible and safe for the treatment of PAA in adult patients. However, further large-scale comparative studies are needed to prove the advantages of this procedure.
Notes
This study was presented at the 48th Annual Meeting of the Korean Society of Coloproctology. April 10-12, 2015, Pusan, Korea.
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.