Clinical Significance of Preoperative Virtual Colonoscopy for Evaluation of the Proximal Colon in Patient With Obstructive Colorectal Cancer
Article information
Abstract
Purpose
Virtual colonoscopy is the most recently developed tool for detecting colorectal cancers and polyps, but its effectiveness is limited. In our study, we compared the result of preoperative virtual colonoscopy to result of preoperative and postoperative colonoscopy. We evaluated also the accuracy of preoperative virtual colonoscopy in patients who had obstructive colorectal cancer that did not allow passage of a colonoscope.
Methods
A total of 164 patients who had undergone preoperative virtual colonoscopy and curative surgery after the diagnosis of a colorectal adenocarcinoma between November 2008 and August 2013 were pooled. We compared the result of conventional colonoscopy with that of virtual colonoscopy in the nonobstructive group and the results of preoperative virtual colonoscopy with that of postoperative colonoscopy performed at 6 months after surgery in the obstructive group.
Results
Of the 164 patients, 108 were male and 56 were female patients. The mean age was 62.7 years. The average sensitivity, specificity, and accuracy of virtual colonoscopy for all patients were 31.0%, 67.2%, and 43.8%, respectively. In the nonobstructive group, the average sensitivity, specificity, and accuracy were 36.6%, 66.2%, and 48.0%, respectively, whereas in the obstructive group, they were 2%, 72.4%, and 25.4%. Synchronous cancer was detected via virtual colonoscopy in 4 of the 164 patients.
Conclusion
Virtual colonoscopy may not be an effective method for the detection of proximal colon polyps, but it can be helpful in determining the therapeutic plan when its results are correlated with the results of other studies.
INTRODUCTION
Colorectal cancer is the third most common cancer in men and the second most common cancer in women worldwide. In Asia, colorectal cancer is the fourth most common cancer in men and the fifth most common cancer in women. Especially, the incidence of colorectal cancer is higher in East Asian countries than in all Asian countries [1]. In Korea, the prevalence of colorectal cancer is the second highest after that of stomach cancer, and the incidence rate of colorectal cancer is the third highest after those of thyroid cancer and stomach cancer. Also, the incidence of colorectal cancer is increasing, and because colorectal cancer develops from a precursor adenomatous polyp, the detection and removal of polyps are important in preventing colorectal cancer [2].
In colorectal cancer evaluation, a proximal colon evaluation is necessary. The incidence of coexisting polyps has been reported to be about 27%–55% and the incidence of synchronous cancer to be about 1.8%–19% [3]. Therefore, the National Comprehensive Cancer Network (NCCN) guidelines have suggested a complete colonoscopy preoperatively. However, in patients who have obstructive colorectal cancer, the colonoscope cannot pass into the proximal colon, so the proximal colon cannot be evaluated. In these cases, virtual colonoscopy may be helpful [4]. However, the clinical significance of virtual colonoscopy has not yet been established. Therefore, the aim of this study is to evaluate the clinical usefulness of preoperative virtual colonoscopy for examining the proximal colon in patients with colorectal cancer.
METHODS
Of the patients who were scheduled for a curative operation based on the diagnosis of a colorectal adenocarcinoma, a total of 164 patients in whom preoperative virtual colonoscopy had been performed between November 2008 and August 2013 were pooled. Patients who needed an emergent operation for colon obstruction were excluded. The 164 selected patients were subdivided into 2 groups: the nonobstructive (137 patients) group and the obstructive group (27 patients), where preoperative colon obstruction was defined as obstruction that prevented the colonoscope from passing into the proximal colon from the primary tumor. In the obstructive group, patients who received a right hemicolectomy were excluded. This is the reason we could not evaluate the proximal colon postoperatively after curative surgery. In the nonobstructive group, the results of preoperative complete colonoscopy were compared with those of preoperative virtual colonoscopy. In the obstructive group, the results of preoperative virtual colonoscopy were compared with those of complete postoperative colonoscopy performed within 6 months after curative surgery.
For virtual colonoscopy, mechanical bowel preparation was essential. The method of administering polyethylene glycol (PEG) was as follows: a total 4 L of PEG was taken 12 hours before virtual colonoscopy. In particular, in patients with preoperative colon obstruction, bowel preparation was performed under close monitoring of defecation. The fasting status was maintained for at least 12 hours. Abdomino-pelvic computed tomography (CT) was performed using a 64-channel multidetector CT scanner (LightSpeed VCT, GE Healthcare, Chicago, IL, USA). An automatic inflator with CO2 (6 L) was used to create the pneumo-colon. The virtual colonoscopic image was reconstructed through the use of software (Rapidia, version 2.8, Infinitt Healthcare, Seoul, Korea).
RESULTS
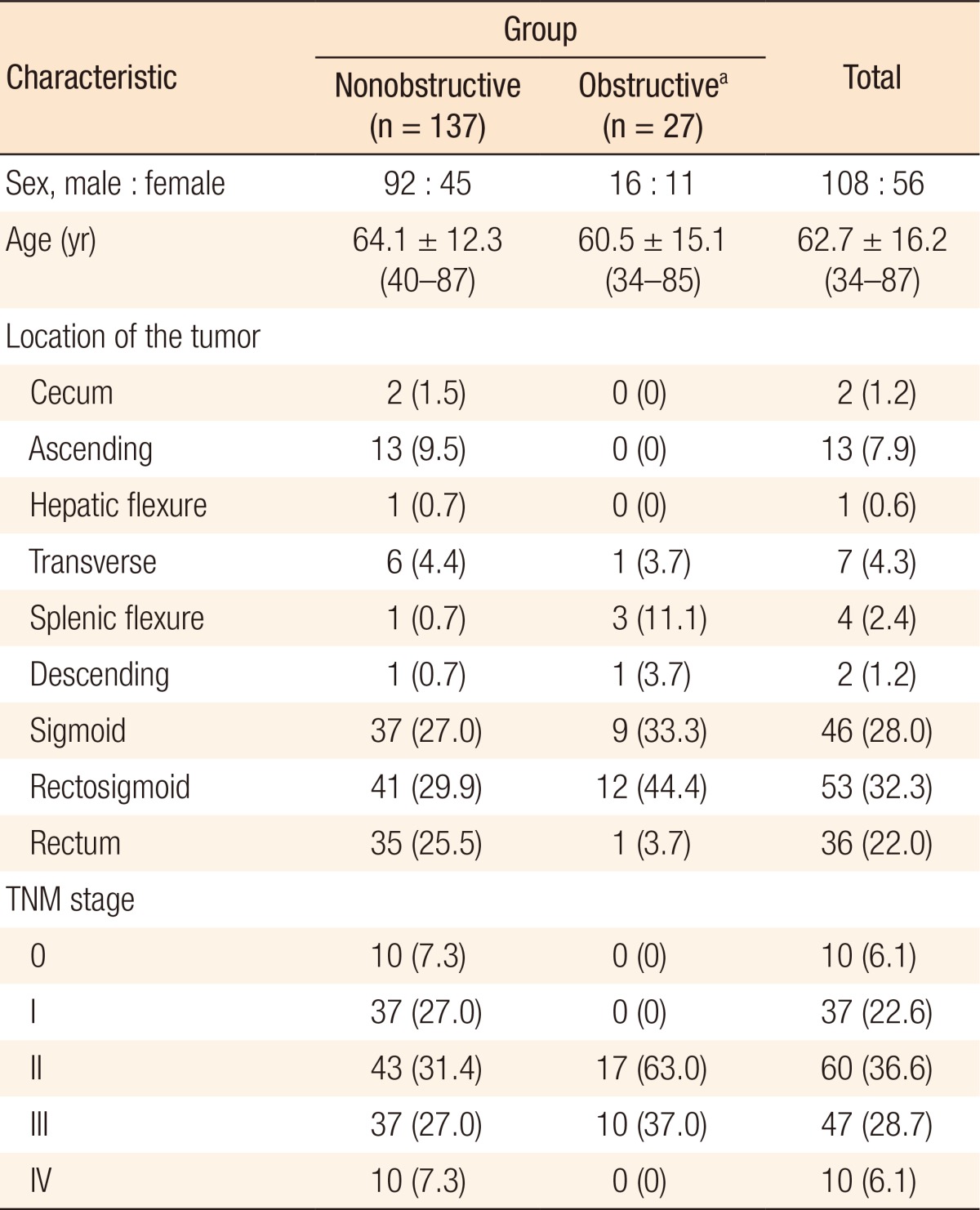
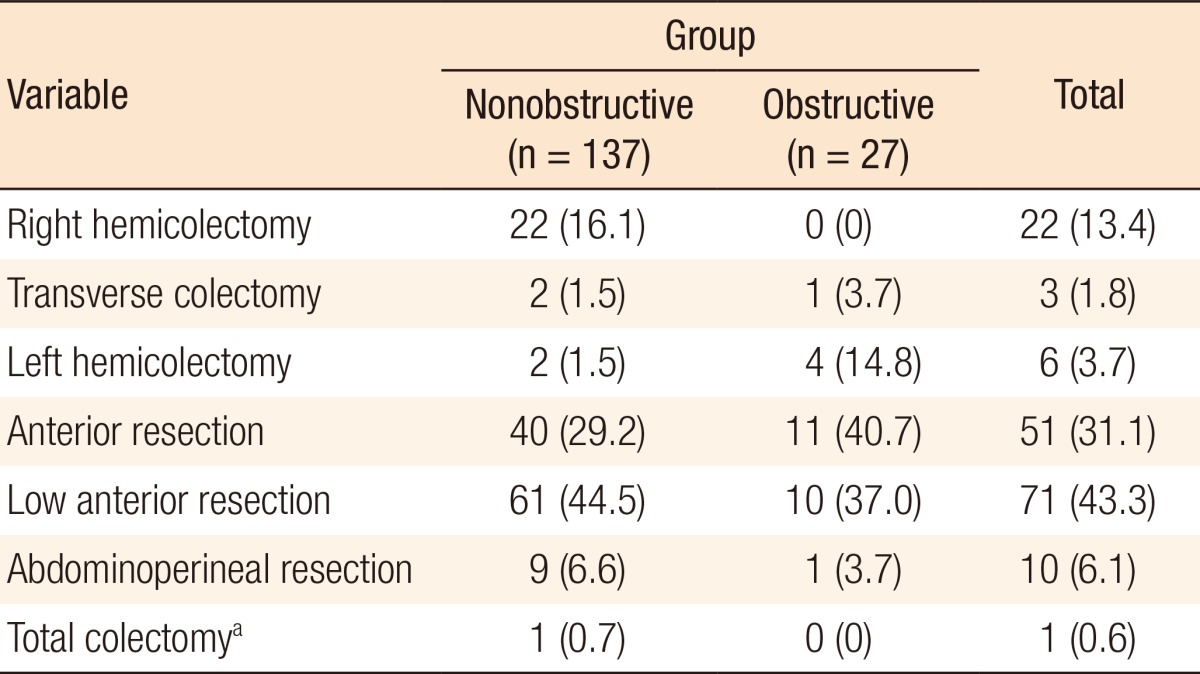
A total of 164 patients were enrolled, including 108 men and 56 women. The mean age was 62.7 years (range, 34–87 years). Preoperative obstruction was found in 27 patients (16.4%). Most of the primary tumors were located in the sigmoid and the rectosigmoid colon. In the nonobstructive group, the tumor was mainly located in the sigmoid and the rectosigmoid colon in 78 patients (56.9%) and in the rectum in 35 patients (25.5%). In the obstructive group, the tumor was located in the sigmoid and the rectosigmoid colon in 21 patients (77.7%). The distribution of the TNM stage is shown in Table 1. The most commonly performed operations were a low anterior resection (71 patients, 43.3%) and an anterior resection (51 patients, 31.1%) (Table 2).
Of the 161 polyps detected by using preoperative colonoscopy in the nonobstructive group, 59 (36.6%) were also detected by using virtual colonoscopy (Table 3). Of the 76 polyps with sizes greater than or equal to 6 mm detected by using preoperative colonoscopy, 45 (59.2%) were also detected by using virtual colonoscopy. Of the 45 polyps detected by using postoperative colonoscopy in the obstructive group, 5 (11.1%) were also detected by using virtual colonoscopy. Of the 20 polyps (≥ 6 mm) detected by using postoperative colonoscopy in the obstructive group, 5 (25.0%) were also detected by using virtual colonoscopy. The detection rate of polyps with sizes ≥ 6 mm was higher than that of all polyps in both groups.
The sensitivity, specificity, and accuracy for polyp detection by using virtual colonoscopy are shown in Table 4. For all polyps, in the nonobstructive group, the sensitivity was 36.6%, the specificity was 66.2%, and the accuracy was 48%. In the obstructive group, the sensitivity was 11.2%, the specificity was 72.4%, and the accuracy was 25.4%. For polyps with sizes larger than or equal to 6 mm, the accuracy of polyp detection was 63.7% in the nonobstructive group and 44.1% in the obstructive group. In the obstructive group, synchronous cancer was detected by using virtual colonoscopy in 4 patients (14.8%). For 2 patients, the operative plan was changed due to virtual colonoscopic findings. The proximal mass was not far from the distal mass, so the proximal mass could be fully included in the resection margin without changing the originally planned operation. The operations performed were an abdominoperineal resection and a left hemicolectomy.
In a 52-year-old female patient, the primary cancer was located at the rectosigmoid junction, and the operative plan was to perform a lower anterior resection. However, cecal cancer was suspected on virtual colonoscopy findings and an uptake of Fluorine-18 fluorodeoxyglucose in the cecum was seen on positron emission tomography (PET)-CT. Therefore, we performed a lower anterior resection and right hemicolectomy. The final path-ological diagnosis of the cecal mass was a well-differentiated, T1N0M0, stage I adenocarcinoma.
A 34-year-old female patient was scheduled for surgery on a distal sigmoid colon cancer found on conventional colonoscopy, but a tumor in the proximal sigmoid colon was found on virtual colonoscopy. Also, based on PET-CT findings, another malignancy in the proximal sigmoid colon was suspected. According to the clinical information, the operative plan was changed to an extended anterior resection. The final pathological diagnosis of the proximal colon mass was an adenocarcinoma.
DISCUSSION
In this study, the accuracy of polyp detection for virtual colonoscopy was 48.0% in the nonobstructive group and 25.4% in the obstructive group. Even though the detection rate of virtual colonoscopy was not high enough, in some patients, the surgical plan was changed based on the result of virtual colonoscopy.
In colorectal cancer patients, the incidence of synchronous colorectal cancer has been reported to be about 1.8%–19% at the time of the diagnosis of colorectal cancer [3]. Therefore, a complete colonoscopy of the entire colon is very important before surgery, and this process of work up is also recommended in the NCCN guidelines [5]. However, in patients with obstructive colorectal cancer, which means that colonoscope cannot pass into the proximal colon, a complete colonoscopy may not be available. In the past, a barium enema was considered as a way to overcome this limitation. The disadvantages of a barium enema include the risk of colon perforation and problems caused by barium remaining in the proximal colon during surgery. With the development of the imaging modality, virtual colonoscopy has been suggested as a possible alternative [46].
Virtual colonoscopy has many advantages. Compared with colonoscopy, the procedure is faster, it provides more physical comfort, sedation is not needed, it is less painful, and it is a less difficult examination [789]. In addition, virtual colonoscopy is an imaging tool used in combination with CT. Therefore, it has the advantage of CT, which can evaluate the extracolonic findings simultaneously [10]. Due to these advantages, the clinical information can be viewed comprehensively. On the other hand, virtual colonoscopy has certain disadvantages. Like the barium enema, the possibility of false positive results is present because of residual fecal material, haustral folds, the impression of organs, or normal variations of the ileocecal valve [1112]. However, through the use of imaging combined with CT, these drawbacks can be overcome. Other disadvantages include radiation hazard and high cost [12].
In colorectal cancer, virtual colonoscopy can be used for the evaluation of colonic polyps and synchronous colorectal cancer. In the literature, the sensitivity of virtual colonoscopy for the detection of adenomatous polyps varies from about 45% to 97% [5]. However, in our study, the sensitivity for the detection of polyps by using virtual colonoscopy was relatively low, being 36.6% in the nonobstructive group and 11.2% in the obstructive group. This difference probably originated from the other studies having different aims and different patient groups. The studies that assessed the sensitivity and the specificity of virtual colonoscopy enrolled a high number of normal or asymptomatic patients who had undergone a virtual colonoscopy for health checkup. Therefore, those studies focused more on detecting small polyps.
Especially in the obstructive group, the sensitivity, specificity, and accuracy of virtual colonoscopic polyp detection were lower than they were in the nonobstructive group. This may be because of residual fecal material due to insufficient bowel preparation. Also, it may have originated from the limitation of our study. In the obstructive colorectal cancer group, the timing between preoperative virtual colonoscopy and postoperative colonoscopy differed by about 6 months. Even though the polyp detection rate was low in our study, a meaningful note is that the detection rate of proximal synchronous colorectal cancer was about 15% in patients with obstructive colorectal cancer.
In conclusion, virtual colonoscopy alone is a limited imaging tool for detecting proximal colon polyps. However, in patients with obstructive colorectal cancer, its use may have a limited benefit in detecting proximal synchronous colorectal cancer.
Notes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.