Treatment of a Recurrent Rectourethral Fistula by Using Transanal Rectal Flap Advancement and Fibrin Glue: A Case Report
Article information
Abstract
Rectourethral fistulas (RUFs) in adults are rare and could result from complicated trauma, and prostatic or rectal surgery. RUFs have been treated initially by using primary repair and omental interposition with or without a colostomy during surgery. Recurrent RUFs require complex surgery, such as a low rectal resection and coloanal anastomosis, an interposition flap of the datos muscle or gracilis muscle, and others. Recently, transanal rectal flap advancement and fibrin glue injection have provided an effective occlusion of RUFs. However, no reports about this technique exist for cases of recurrent RUFs. We report a case of a recurrent RUF successfully repaired by using transanal rectal flap advancement combined with fibrin glue injection into the fistula tract. The postoperative course was uneventful without complications. At the 1-year follow-up, no complications such as urethral stricture or recurrence existed, and voiding was normal without anal incontinence.
INTRODUCTION
In prostate cancer, rectourethral fistula are known to develop after retropubic prostatectomy in 0.5 to 9% of patients [1]. When the size of the rectourethral fistula is small, a natural cure is anticipated after urinary diversion or a temporary colostomy. Thomas et al. [2] reported that about 54% of the rectourethral fistula cases were naturally treated if not accompanied by fecaluria. However, in cases of major symptoms, such as recurrent urinary duct infection or fecaluria, and development of complications, surgical treatments are required. The ratio of natural healing after primary treatment of a rectourethral fistula, including a colostomy and urinary tract catheterization, was reported at 14 to 46.5%. In cases of fecaluria, systemic infection, and recurrence of colostomy and urinary diversion, additional surgical treatments are required [2-4].
There are various methods of surgery for treating a rectourethral fistula that is a recurrent occurrence. When rectal trauma is found during a prostatectomy, a colostomy and primary suture are performed, or the intraabdominal approach for interposition can be performed [3]. In the transperineal approach, interposition of the gracilis muscle and the dartos muscle is often used, but visual fields are difficult to secure during surgery, and the risk of causing urinary incontinence is high.
Recently, advancement of a rectal flap through the anus was introduced as a simple and effective method with a short operative time and few complications [4]. In addition, a successful case of treating a patient, who was not observed with an internal opening in cystoscopy, by injecting cynoacrylate glue, which is a kind of a mixture solution having strong stenosis and hemostatic effects, into the fistula via an endoscope was reported [5]. However, no successful case of treating a patient who had a recurrent rectourethral fistula which was observed at both the urethera and the rectum by injecting fibrin glue into the fistula and simultaneously performing a rectal advancement flap has been reported yet. We report, with a literature review, a case of successful treatment using rectal advancement flap and fibrin glue for a patient who had a recurrent rectourethral fistula that developed after primary suture and colostomy.
CASE REPORT
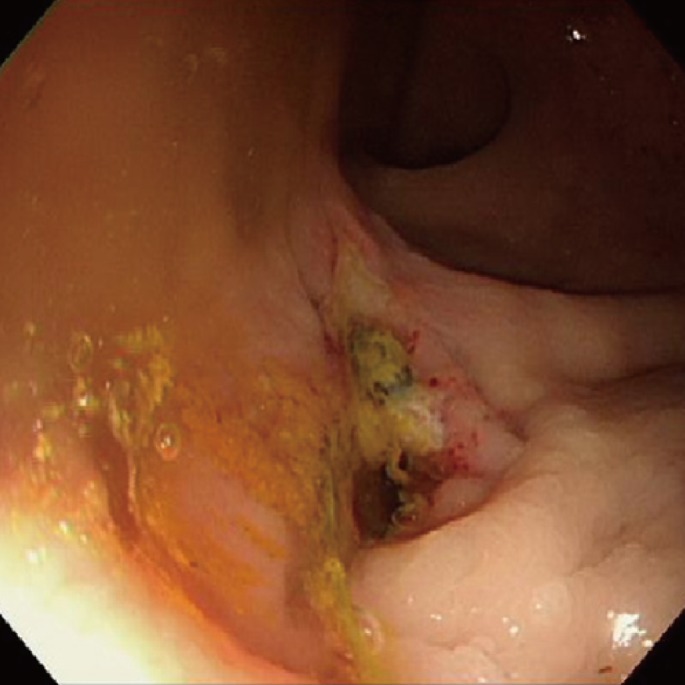
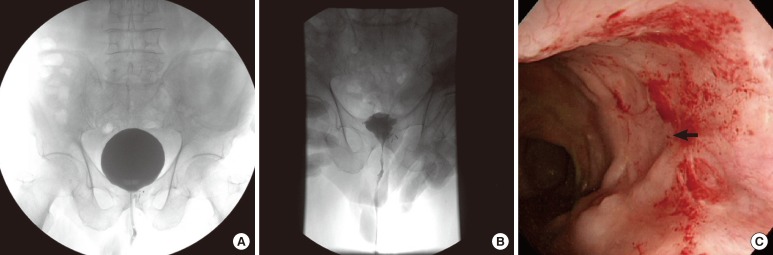
A 75-year-old male patient visited Chungbuk National University Hospital complaining of pain in the right flank and frequent urination that had stared 2 months before. Transrectal ultrasound showed a low-echogenicity at the left lobe of the prostate. After a fine-needle aspiration biopsy under the guidance of transrectal ultrasound, a diagnosis of an adenocarcinoma with 1-mm invasion according to the Gleason's score (3 + 3) was made; then, an extensive retropubic prostatectomy was performed. On the postoperative day 7, leukocytosis, fever, fecaluria and pneumaturia were observed, and the drainage was dark brown. Upon digital rectal examination, a fistula opening was detected at the 12 o'clock direction. At sigmoidoscopy, a perforation with a 1.0-cm diameter was observed 5 cm above the anal verge (Fig. 1). On the diagnosis of a rectourethral fistula, primary suture on the colostomy and fistula was performed. At 3 months after the operation, recurrence of the rectourethral fistula was observed, but no further procedure was performed because spontaneous closure was expected. However, because the rectourethral fistula persisted on the sigmoidoscopy, retrograde cystogram and cystoscopy after 6 months, eventually surgery was decided (Fig. 2).
Sigmoidoscopy and retrograde cystogram showing the rectourethral fistular opening at 6 months after the primary repair with a colostomy for a rectourethral fistula: (A) sigmoidoscopy showing the recurrent rectourethral fistula and rectal fistular opening, and (B) urethrogram showing the rectourethral fistula, with the arrow indicating the fistular tract.
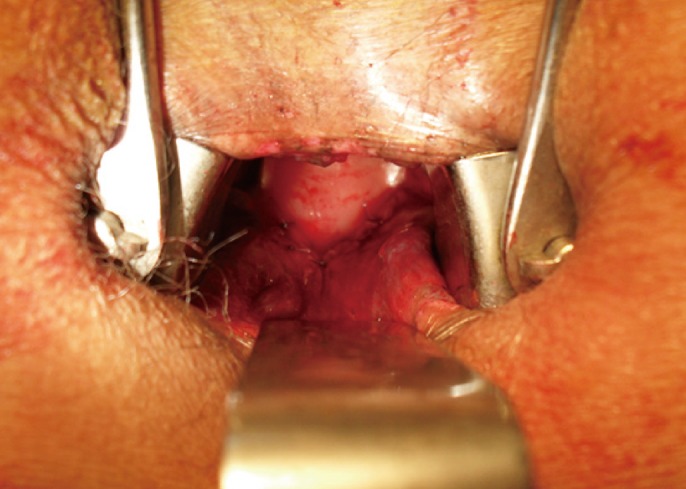
Prior to surgery, an 18 Fr urinary catheter was inserted to detect the urethra-side fistula during surgery and to prevent leakage of fibrin glue. Under spinal anesthesia, the patient was in the Jackknife position. Using a Parks anal retractor, the anus was opened, and the rectum-side opening was confirmed; then, stay sutures were made at the surrounding four directions. After injection of 1 : 100,000 epinephrine diluted with saline into the submucosa of the rectum, a Y-shaped incision was made on the rectal mucosa to separate the mucosal and submucosal layer from the muscular layer. The fibroid fistular opening and the granulation tissues around the stay sutures were removed using electrocautery, and the urethra-side opening was confirmed. The urethra-side opening was 2 mm in diameter, and the urinary catheter was observed. After injection of fibrin glue (1 mL; Greenplast, Green-Cross Co., Seoul, Korea) into the fistula using a syringe, we waited for 2 to 3 minutes until the fibrin glue had clotted. A simple interrupted suture was horizontally made on the rectal muscle layer using Vicryl 3-0. After drawing down the rectal advancement flap making a U shape, a simple interrupted suture was performed using Vicryl 3-0 (Fig. 3). The operative time was 25 minutes, and the urinary catheter was maintained after surgery without change. No piece of fibrin, which had been used during surgery, was found with the naked eye.
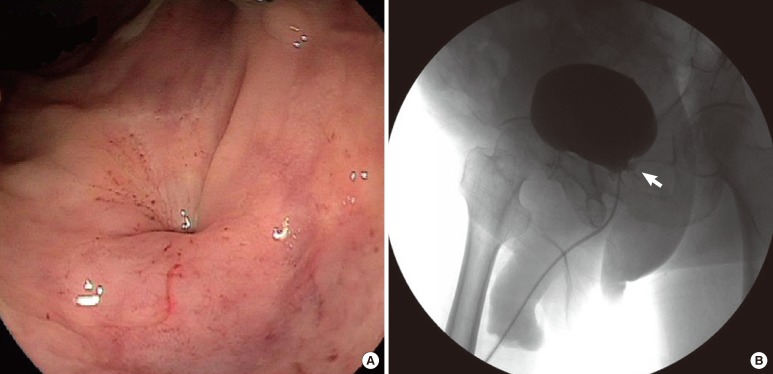
At postoperative three months, voiding cystourethrography and sigmoidoscopy were conducted to confirm a complete closure of the fistula (Fig. 4), and the sigmoid colostoma was taken down at postoperative five months. Until now at postoperative one year, there has been no clinical evidence of recurrence of the fistula, and sigmoidoscopy confirmed that the fistula closure site has healed well.
DISCUSSION
According to their etiology, rectourethral fistulas are classified into congenital, iatrogenic, traumatic, neoplastic and inflammatory. A congenital rectourethral fistula is more common than an acquired one, with the incidence of 5,000 to 1. It is more common in boys and is often accompanied by an anorectal anomaly. Posterior sagittal anorectoplasty is the standard procedure for the treatment of a congenital rectourethral fistula [6]. Rectourethral fistulas in adults are very rare, and etiology includes perineal trauma, prostate and rectal surgery, radiologic treatment on the pelvic bones, cryotherapy and Crohn's disease [7].
A rectourethral fistula after retropubic prostatectomy is rare, with an incidence of 0.5 to 9%. Various treatments have been introduced, but no standard procedure has been established yet. Rectal trauma occurring during surgery can be initially treated using a proximal diverting colostomy, primary suture or interposition. After the primary suture, the recurrence rate of a rectourethral fistula is reported to be 10 to 40%, and highly advanced techniques are necessary for the complicated surgery of recurrent cases [3]. The York-Mason procedure, which is a posterior middle transsphincteric approach, requires less operative time and blood loss compared with traditional techniques. In addition, perfect separation can be made in accordance with the directions of urine and stool. However, when the posterior middle transsphincteric approach is used, damage to the neurovascular bundle, which is important for sexual and voiding functions, should be avoided [8]. The York-Mason procedure reports a nearly 100% success rate and a low complication rate. However, compared with the rectal advancement flap procedure, the operative time is long with more blood loss, and patient satisfaction is lower due to postoperative pain [4]. Wilbert et al. [9] introduced transanal endoscopic microsurgery, but only for 2 patients. Ryan et al. [10] introduced a method of using gracilis muscle transposition. The gracilis muscle is difficult to obtain, and complications such as flap necrosis developed due to the narrow space between the rectum and the urethra. Garofalo et al. [4] recently performed 12 cases of transanal repair using a rectal advancement flap. The success rate was 66.6% (8 cases) after the first repair, 50% (2 cases) after the second operation for recurrent cases, showing a total success rate of 83% (10 cases). Urethral stricture developed in all 3 patients who underwent the York-Mason procedure whereas only 1 patient out of the 12 patients who underwent a rectal advancement flap reported urethral stricture, demonstrating its excellence in the treatment of rectourethral fistulas. However, both the rectal advancement flap and the York-Mason procedure still have difficulty in suturing accurately to close the internal opening; urethral stricture by suture can also occur.
Fibrin glue is the first biomaterial popularly used for fistula treatments. Fibrin glue activates thrombin to form fibrin clots. During the slow process of fibrinolysis, fibrin clots promote tissue healing to close the fistula. Fibrin glue not only closes the fistula but also prevents stenosis, reduces serous fluid, and leads to endo-epitheliatization [11]. Treatments of complex fistulas and rectovaginal fistulas using fibrin glue report a 30 to 80% success rate without significant complications. Two cases of rectourethral fistulas caused by Crohn's disease and by prostatectomy were reported to be treated with fibrin glue [12, 13]. Bhandari et al. [5] reported a successful case of a rectourethral fistula treated by injecting cynoacrylate glue into the rectal fistula transanally via a colonoscope. The glue is a type of mixture solution having strong adhesive and hemostatic effects. Fibrin glue and the mixture solution do not show side effects and tissue reactions, and they can be used safely. Since the size of the fistular opening is usually not large, the fibrin glue promoting the tissue healing process is effective in preventing complications such as stenosis caused by suturing the urethra.
As described above, the rectal advancement flap and injection of fibrin glue is a simple and effective procedure, but it still has a limitation: suture of the internal opening. The case of Bhandari et al. [5] involved a rectourethral fistula with a very small opening that could not be detected by cystoscopy. Accordingly, it was difficult to apply to the recurrent case in the present report, which had an internal opening. In the present case, the procedure with fibrin glue without suturing the opening could be finished in 25 minutes, which was shorter than the time of Garofalo et al. [4], who spent 83 minutes for replacing suture of the internal opening in the rectal advancement flap procedure with fibrin glue. In addition, urethral stricture was prevented by retaining a urinary catheter for over 3 weeks.
We report, with a literature review, a case of a recurrent rectourethral fistula after primary suture and colostomy. An opening was observed in cystoscopy, and the rectal opening was large, as confirmed in colonoscopy. The patient was treated successfully with fibrin glue injection and rectal advancement flap without suturing the internal opening.
ACKNOWLEDGMENTS
This work was supported by the research grant of the Chungbuk National University in 2010.
Notes
No potential conflict of interest relevant to this article was reported.