A New Technique Using Ultra-slim Endoscopy for High-Grade Crohn's Stricture
Article information
Abstract
Crohn's disease (CD) is a chronic inflammatory bowel disease of unknown etiology. Most patients with CD will eventually develop a stricturing or penetrating complication. Colonoscopic findings may predict the clinical course in patients with CD. Moreover, since CD patients are at increased risk for developing dysplasia and colorectal cancer, surveillance colonoscopy is necessary for the detection of malignancies. We describe here a CD patient with a high-grade anorectal stricture who successfully underwent a total colon examination with an ultra-slim upper endoscope after an insertion failure with a standard colonoscope and gastroscope.
INTRODUCTION
Crohn's disease (CD) is a chronic inflammatory bowel disease (IBD) of uncertain etiopathogenesis. Most patients with CD will eventually develop a stricturing or penetrating complication [1]. Colonoscopy may predict the clinical course in patients with CD because deep and extensive ulcerations are associated with increased risks of complications and surgery [2, 3]. Moreover, because CD patients are at increased risk for development of dysplasia and colorectal cancer (CRC), periodic colonoscopy is essential for the surveillance of malignancies [2].
We describe here a CD patient with a high-grade anorectal stricture who successfully underwent a total colon examination with an ultra-slim upper endoscope (GIF-XP260N; 5.0 mm Ø with an instrumental channel of 2.0 mm Ø; Olympus Co., Tokyo, Japan) after failure with a standard colonoscope (CF-H260AI, Olympus Co.) and gastroscope (GIF-P230, Olympus Co.).
CASE REPORT
A 37-year-old man, diagnosed with CD in 1999, presented with diarrhea and a perianal fistula. He had been treated with mesalazine, 3 g/day, but had not undergone a colonoscopy since the diagnosis because of a high-grade stricture in the anorectum. In 2002, he was referred to our gastrointestinal department for a second opinion on his CD. Diarrhea and intermittent abdominal pain developed three months before admission. An abdominal computed tomography (CT) scan demonstrated diffuse bowel-wall thickening and enhancement throughout the ileum and colon with multifocal strictures (Fig. 1). Laboratory data were unremarkable. After informed consent had been obtained, a colonoscopy was performed to assess disease activity and as surveillance for cancer. At three centimeters from the anal verge, however, passage of both a standard colonoscope and gastroscope (GIF-P230, 8.5 mm Ø; Olympus Co.) was blocked due to severe anal stricture (Fig. 2A). We, therefore, performed a colonoscopy with an ultra-slim upper endoscope (GIF-XP260N, Olympus Co.), which passed through the rectal stricture without any resistance (Fig. 2B). Although other focal strictures were found in his transverse (Fig. 3C) and sigmoid (Fig. 3D) colon, we succeeded in reaching the cecum (Fig. 3A) in 3 minutes, but we failed to reach the terminal ileum due to a narrowed ileocecal valve (Fig. 3B). Careful examination of the colon revealed a huge ulcer in the transverse colon. Biopsies were taken from the mucosa of the anal stricture to rule out colon cancer. These biopsies showed no evidence of malignancy.

Computed tomography scan showing a multiple colonic stricture, mesenteric root enhancement, and pseudosacculation in the antimesenteric border of a small bowel loop.

Endoscopic view of the anorectal stricture: (A) initial colonoscopy, showing a luminal stricture with ulceration and inflammatory exudates, and (B) second endoscopic view using ultra-slim upper endoscopy.
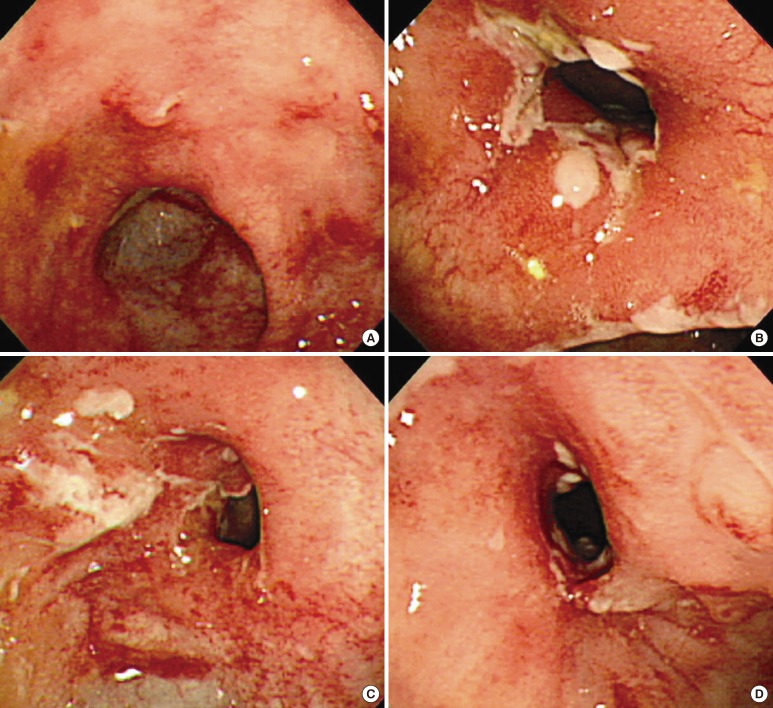
Ultra-slim upper endoscopic views: (A) ulceration and erosion in cecum, (B) Crohn's stricture on the mucosa of the ileocecal valve, (C) Crohn's stricture and a huge ulceration in the transverse colon 55 cm from the anal verge, and (D) Crohn's stricture in the sigmoid colon 25 cm from the anal verge.
DISCUSSION
The primary advantage of a small-caliber endoscope over a standard colonoscope is its smaller diameter and greater flexibility, making it more suitable for patients with narrowed colons. Although full colonic examination by ileal intubation using a small-caliber upper endoscope (GIF XP160, 5.9 mm Ø; Olympus, Tokyo, Japan) (Fig. 4) has been shown to be feasible in non-IBD patients [4], to our knowledge, there have been no reports describing the use of an ultra-slim upper endoscope for total colonoscopy in CD patients with strictures. Our patient had never undergone a colonoscopy due to high-grade anal and colonic strictures. The ultra-slim upper endoscope was useful for examining the total colon and for taking biopsies.

Left (arrow), ultra-slim upper endoscope (GIF-XP260N, 5.0 mm Ø with instrumental channel = 2.0 mm Ø, working length = 110 cm; Olympus Co., Tokyo, Japan). Right (arrow head), standard colonoscope (CF-H260AI, 12.9 mm Ø with instrumental channel = 3.7 mm Ø, working length = 133 cm; Olympus Co.)
A mucosal evaluation using an ultra-slim endoscope has two advantages. After introduction of a biologic agent, mucosal healing is likely to predict a more sustained clinical remission and a better long-term outcome. In addition, because CRC is a problem in patients with long-lasting CD, the use of an ultra-slim endoscope may make surveillance and biopsies possible. In addition, although CD patients with strictures and prestenotic dilatation, as well as all medically-refractory patients with CD, should be considered candidates for surgery, asymptomatic patients and those with mild symptoms require frequent endoscopic examination.
Notable characteristics of the gastroscope are a smaller suction channel, which makes it more difficult to clear liquid stool/debris, and its operative channel, whose exit is opposite that of the colonoscope. Various techniques may be used to overcome these differences. When using a gastroscope for colonoscopy, more torque is necessary because of its limited angulation range (up/down 210°/90° and right/left 100° vs. in a colonoscope, up/down 180° and right/left 160°). Also, a gastroscope is more rigid than a colonoscope, and an endoscopist knows that he or she has previously failed the index examination [5].
Colonoscopy in this patient was performed by an expert (KKJ) without any complications. The primary concerns associated with colonoscopy in patients with high-grade strictures are its operator-dependent nature and its higher risk of perforation [6]. As long as appropriate care is taken, colonoscopy with an ultra-slim upper endoscope might be feasible and useful in selected patients with CD strictures.
Moreover, colonoscopy using a gastroscope may be useful even though there have been no reports describing the use of an ultraslim upper endoscope for total colonoscopy in patients with stricturing CRC. However, compared to IBD patients, examining the entire colon may be difficult even though passing through the entire colon may be possible. A plausible explanation for the greater difficulty is that the healed colon in patients with IBD tends to be shortened compared to its original length. However, a colon with stricturing CRC is not shortened. Instead, a study reported that CT colonography may have a role in the evaluation of the more proximal colon in patients with stricturing colon cancer [7]. In summary, when CD patients with anorectal stricture are encountered, gastroscopy could be a reasonable diagnostic option for a colon examination.
Notes
No potential conflict of interest relevant to this article was reported.