Extraperitoneal Spread of Anorectal Abscess: A Case Report and Literature Review
Article information
Abstract
Supralevator abscess is a rare form of anorectal disease responsible for very rare but morbid manifestations, one of which is superior spread through fascial planes. We present a rare case of a spreading anorectal abscess in a patient who presented with only diffuse abdominal pain, and we review similar cases in the literature according to anatomical considerations, presentation, diagnostic procedures, and treatment options. We identified 7 previously reported cases of spreading anorectal abscesses. Most abscesses had a horseshoe morphology, and all patients presented or developed abdominal pain. All patients had perianal swelling and pain. Five out of 7 patients were previously mistreated. Only 2 abscesses spread through both the pre- and retroperitoneal planes. Abdominal pain is a dominant feature of extraperitoneal inflammation originating from anorectal abscesses. The absence of perianal signs is rare, and proper inspection of the patient along with the medical history can lead to quicker diagnosis and decisive treatment.
INTRODUCTION
Anorectal abscesses represent one of the most often encountered colorectal diseases in the emergency department (ED) with 70, 000 to 90,000 annual cases in the United States. They occur from blockage or infection of anal crypts and glands due to chronic constipation, inflammatory bowel diseases (IBD; Crohn disease or ulcerative colitis), malignancy, foreign bodies, and sexually transmitted diseases [1]. Parks et al. [2] classified anorectal abscesses into perianal, ischiorectal, intersphincteric, and supralevator [2]. Supralevator abscesses are the least common, occurring in 1% to 9% of patients, and they present with nonspecific anal pain and fever while redness or swelling of the buttocks may be absent. Spread across specific anatomic spaces is a very rare complication but may potentially lead to sepsis and death. We report a unique case of supralevator abscess in a patient who presented with only diffuse abdominal pain while the abscess expanded massively through both the abdominal and retroperitoneal fascia.
CASE REPORT
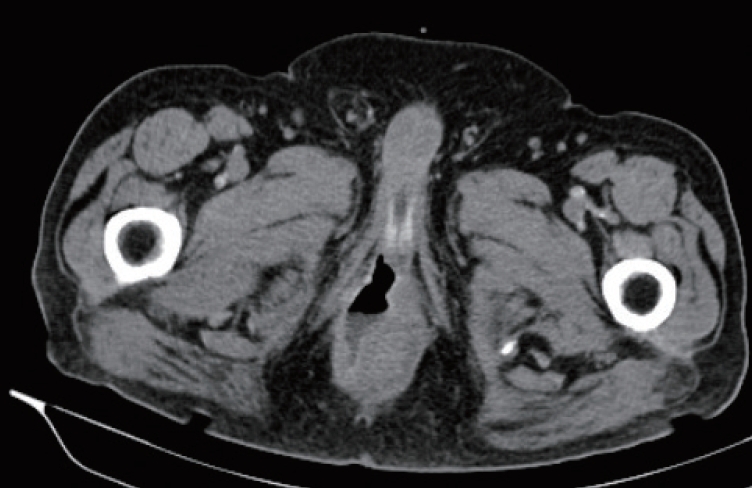
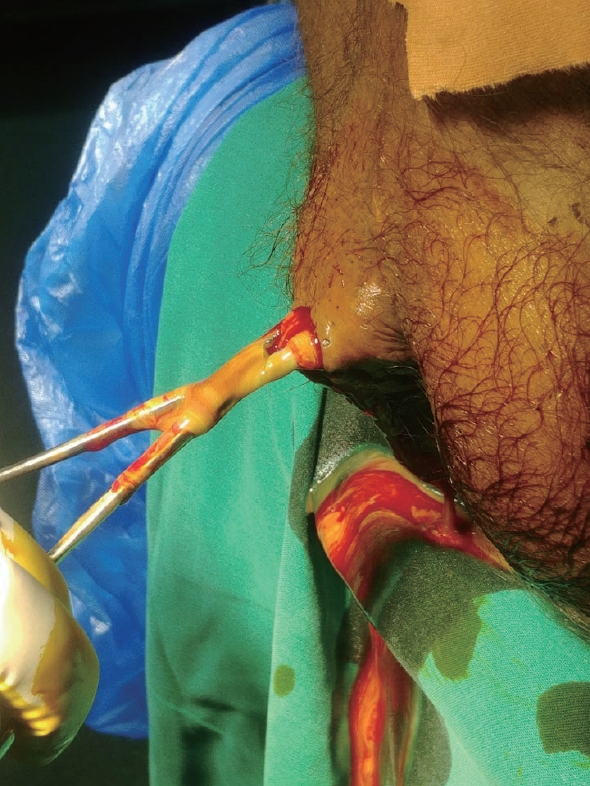
A 57-year-old male presented to the ED with diffuse pain vaguely located at the lower abdomen over the previous 24 hours. He was awake and alert and did not complain of pain in any other site. His past medical history included type 2 diabetes mellitus (DM), gout, myocardial infarction and chronic obstructive pulmonary disease. There was no history of constipation or perianal inflammation. He was a heavy smoker, his body mass index was 45 kg/m2, and he admitted poor compliance with all of his medications. On admission he was febrile (body temperature, 39.5°C), hypertensive (blood pressure, 160/90 mmHg), slightly tachycardic (heart rate, 88 beats/minute), and hyperglycemic (blood glucose, 250 mg/dL). Physical examination revealed pain with deep palpation, no rebound tenderness, negative Giordano sign, and no signs of deep vein thrombosis in the extremities. The scrotum and groin were normal. The digital rectal examination was negative for blood but revealed mild nonspecific pain. A plain abdominal radiograph was normal, and laboratory findings consisted of elevated white blood cell count and C-reactive protein (white blood cells, 26,000/μL; neutrophils, 85%; C-reactive protein, 21.58 mg/L). Under suspicion of bowel perforation, abdominal contrast-enhanced computed tomography (CT) was performed and revealed a perirectal fluid-filled cavity and air spreading retroperitoneally and through the abdominal wall fascia (Fig. 1, 2) and a perirectal fluid-filled cavity (Fig. 3, 4). In addition, random diverticula were spotted at the left and sigmoid colon. After fluid resuscitation and intravenous antibiotics, the patient was taken to the operating room and underwent a right gluteal incision and intrasphincteric drainage (Fig. 5). A Pezzer tube was placed and used for daily povidone-iodine washes. After 10 days, the patient was afebrile with normal lab values, and he was discharged from the hospital. The patient had no signs of recurrence during a 6-month follow-up period.

Axial view showed an emphysematic collection of air at the anterolateral abdominal wall. This image can be easily mistaken for diverticulitis or localized bowel perforation, but with close inspection, the air is spotted extraperitonealy.
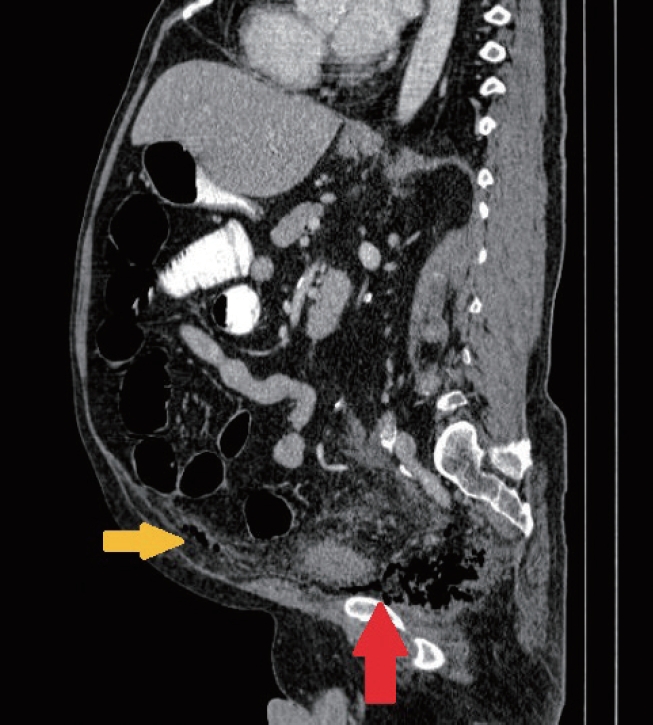
Sagittal view showed the migration from the supralevator plane (red arrow) preperitoneally (yellow arrow).

Frontal view of the abscess cavity on the right side (circle) with contralateral extension to the left suprasphincteric space (arrow).
Written informed consent for publication of the clinical images was obtained from the patient.
DISCUSSION
Deep spreading perianal abscesses represent one of the most morbid entities in anorectal disease. Their rarity and insidious clinical manifestations can lead to delayed diagnosis, severe sepsis, and death. Comorbidities, such as IBD, heart disease, obesity, or DM, raise the risk of complications [3], and the absence of typical signs along with abdominal pain can confuse the physician in search of abdominal pathology.
Retroperitoneal abscesses usually originate from the genitourinary tract, may be idiopathic or postoperative, and infrequently involve other organs like the colon, duodenum, and pancreas. Traditionally, lumbar incision was proposed for treatment, with the transperitoneal approach being the least successful, in an overall mortality background of 26% highly associated with critically ill patients and delayed diagnoses [4].
Anatomically, the supralevator space is a pelvic compartment above the levator ani muscle that communicates anteriorly with the space of Retzius, bilaterally with the retroinguinal spaces, and posteriorly with the retroperitoneum. The puborectalis muscle acts as a barrier to expanding abscesses. However, abscesses can rarely appear above or inside the muscle, usually along with a fistula, allowing the spread of inflammation through both anterior and posterior extraperitoneal abdominal compartments.
The therapeutic plan is vast, and many approaches have been proposed. Percutaneous intersphincteric drainage for limited supralevator abscesses is more difficult, and even fluoroscopic monitoring of the abscess often has inadequate results and might prolong sepsis [5]. The gold standard has always been open drainage and debridement. Fistulotomy can be achieved in one stage with drainage, but there is still some controversy in suprasphincteric abscesses [6]. In abscesses with massive pre- or retroperitoneal extension, access to the peritoneal cavity must be avoided due to the high risk of contamination and secondary peritonitis. Optimal treatments have been proposed by different authors, including abdominal stab-like incisions [7] or extraperitoneal drainage with lower midline abdominal incision with excellent outcomes [8, 9]. The wound can be closed primarily with drains or with vacuum assistance devices [10, 11]. Among the literature, a case of ischiorectal horseshoe abscess with anterolateral extraperitoneal spread was treated with open drainage, canalization through the ischioanal fossa through an abdominal incision, and diversion loop colostomy while performing fistulotomy, all in the same operation [12]. On the contrary, a complicated case of expanding abscess causing ileus was treated successfully with simple drainage after a rather difficult diagnosis [13].
We identified 7 previous cases of anorectal abscesses that fulfilled our criteria of expansion through imaging and clinical presentation (Table 1). To our knowledge, these are all the cases that have been reported. Although there was not a specific type of predominant abscess, 4 out of 7 had a horseshoe morphology. Six patients had abdominal pain at presentation, while the 7th developed abdominal pain with abscess expansion during hospitalization. We conclude that abdominal pain is indicative of an extraperitoneal spreading abscess and a strong indication for further diagnostic studies and imaging, especially in the presence of a previously discovered anorectal abscess. Five patients were either insufficiently treated or misdiagnosed (extension of the primary abscess or the condition itself), and they required a secondary intervention as their conditions worsened. Only 2 out of 7 patients were reported to have uncontrolled DM, but most of the authors did not investigate or did not mention basic medical history elements. All patients survived. We strongly consider early recurrences, after incision, as a major risk factor for abscess expansion, especially if the patient bears comorbidities, such as DM. Lastly, the length of hospital stay ranged from 5 days to 1.5 months with a median of 18 days, although the hospitalization period was not thoroughly analyzed because patients were treated with multiple sessions and sometimes by different surgeons and institutions.
Despite their rarity, extended anorectal abscesses should be considered in differential diagnosis for a septic patient with multiple comorbidities. Immediate resuscitation, CT imaging, and definite intervention are necessary for proper diagnosis and treatment. Expansion of inflammation is unpredictable and can occur in various anatomic planes. Keeping in mind the various manifestations of the disease and its potential spread, physicians could avoid delayed diagnosis or unnecessary laparotomy. Finally, abdominal pain strongly indicates spreading fasciitis, and more aggressive treatment is often needed to ensure a good prognosis for this potentially lethal condition.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
We would like to show our gratitude to the Director of Surgery, Spyros Rathosis M.D., Ph.D., for his permission and invaluable guidance about the case.