Is There a Relationship Between Stool Consistency and Pain at First Defecation After Limited Half Hemorrhoidectomy? A Pilot Study
Article information
Abstract
Purpose
While the first defecation pain is a problem following hemorrhoidectomy, it is unknown whether the stool consistency has an influence on pain. This pilot study aimed to investigate whether the intensity of defecation pain varied according to stool consistency.
Methods
This prospective cohort study evaluated patients who underwent hemorrhoidectomy in combination with injection sclerotherapy for grade III or IV hemorrhoids. The pain intensity and stool form during the first postoperative defecation were self-recorded by the patients using a visual analogue scale (score of 0–10) and Bristol Stool Form Scale, respectively. The patients were classified into 3 groups according to stool consistency, and the intensity of defecation pain was compared among the groups using analysis of variance.
Results
A total of 61 patients were eligible for this study and were classified into the hard stool (n=15), normal stool (n=21), and soft stool groups (n=25). No significant intergroup differences were identified in the intensity of pain at defecation (P=0.29).
Conclusion
This pilot study demonstrated that there were no clear differences in pain intensity during the first defecation after surgery among the 3 groups with different levels of stool consistency.
INTRODUCTION
Intense postoperative defecation pain is a well-known complication following hemorrhoidectomy [1-3]. In particular, the first defecation following surgery is stressful and painful for patients, even after undergoing gynecological surgery [4]. One of the practices recommended by surgeons is the administration of stool softeners [5, 6]. However, it remains unknown whether hard stool, normal stool, or soft stool minimizes defecation pain. The author hypothesized that harder stool would have an increased physical impact on the wound, thereby causing more pain. There was no precedent study using Bristol Stool Form Scale (BSFS) [7] for the consistency of the postoperative stool. The aim of this study was to test this hypothesis via an experiment using BSFS.
METHODS
Study design and setting
This was a prospective cohort study of patients who underwent distal hemorrhoidectomy with aluminum potassium sulfate and tannic acid (DH-ALTA) [8] for grade III or IV hemorrhoids between March 2019 and July 2019 at the Yano Proctological Clinic (Takamatsu, Japan). The patients were classified into 3 groups according to stool consistency, and the intensity of pain at defecation was compared among the 3 groups.
Exclusion criteria
Patients who met any of the following criteria were excluded: complication with anal fistula or anal fissure, history of proctological surgery, pregnancy, inflammatory bowel disease, and consent for participation not provided. Patients who submitted no records, those who incorrectly recorded the first defecation, those who did not defecate once over 3 days, and those who did not adhere to instructions regarding oral analgesics were also excluded.
Ethics and permissions
The study protocol was approved by the independent ethics committee of the Japan Medical Association Ethical Review Board on 25th February 2019. The study is registered under the Medical Information Network and clinical trial registry (JMACCT-CTR Number IIA00413). The study was performed according to the Declaration of Helsinki, and written informed consent was obtained from all participants prior to inclusion in the study.
Procedures
All hemorrhoidectomies were performed as day surgeries, and all 3 hemorrhoids were treated. The DH-ALTA procedure was used for hemorrhoidectomy. In this procedure, the internal hemorrhoid components are not resected, but instead, sclerosing agents (ALTA; Zione, Tanabe-Mitsubishi Pharma Corp., Osaka, Japan) are injected into them, and only the external hemorrhoid components are resected. In the conventional DH-ALTA procedure, the external hemorrhoids are excised via ligation, whereas in this study, diathermy was used to excise the external hemorrhoids without any ligation (Fig. 1). Surgery was initiated after inducing local anesthesia in the patient in the Sims’ position. For local anesthesia, 20 mL of 1.0% lidocaine was submucosally injected to the anal verge and around the hemorrhoids. The external hemorrhoids were resected before ALTA was injected into the internal hemorrhoids. A 25-gauge needle was used for ALTA injection. The surgeon resected the larger 2 of the 3 hemorrhoids and decided to leave the smallest hemorrhoid unremoved. ALTA was injected into all 3 hemorrhoids. Using a proctoscope, the ALTA solution was submucosally injected into the internal hemorrhoids, and the total amount of ALTA injected was recorded. The surgery was deemed to start when local anesthesia was initiated and to end when the ALTA injections were completed. The surgery time was recorded accordingly. The wounds were left open. No sponge dressing was placed in the anal canal after surgery. All procedures were performed by an experienced surgeon.

Schematic diagram showing the procedure of limited half hemorrhoidectomy with aluminum potassium sulfate and tannic acid (ALTA) injection sclerotherapy. Gray dotted lines indicate removal of 2 external hemorrhoids (EH) at the dentate line via diathermy. Black dotted arrows indicate injection of ALTA solution into 3 internal hemorrhoids (IH).
Postoperative care
For all patients, oral nonsteroidal anti-inflammatory drug (NSAID, loxoprofen sodium hydrate; Loxonin 60 mg, Daiichi-Sankyo, Tokyo, Japan) tablets were used to control pain. The patients were instructed to take a 60-mg tablet orally every 6 hours for 3 days. The first NSAID tablet was administered in the operating room immediately after surgery. At their individual discretion, patients chose whether to receive the laxative magnesium hydroxide (660 mg/day) for 7 days from 4 days prior to surgery. All patients were recommended to consume adequate amounts of dietary fiber and water and to use warm sitz bath.
Assessments
In this study, stool consistency was evaluated using the BSFS. A nurse who was not involved in the study provided a sheet of paper containing illustrations of 7 different forms of stool with a verbal explanation of the illustrations to the patients. This was back-translated into Japanese by a native English speaker who was also fluent in Japanese into the following explanations: type 1, separate hard lumps, like nuts; type 2, sausage-shaped but lumpy; type 3, sausage-shaped but with cracks on the surface; type 4, sausage or snake-shaped, smooth and soft; type 5, soft blobs with clear-cut edges; type 6, fluffy pieces with ragged edges, mushy stool; and type 7, watery with no solid pieces. The nurse trained patients to record the stool consistency and intensity of pain at defecation on recording forms after each defecation for 3 days after surgery. On the forms, there were three 10-cm straight lines per day to record the pain intensity for up to 9 defecations in 3 days. The intensity of pain during defecation was rated 0 to 10 using a visual analogue scale (VAS) (0 cm representing no pain at all; 10 cm representing the worst pain imaginable). There was a blank space below the straight line for recording which stool form (type 1–7) most applied to the patient. The VAS line and stool form space were both left blank when there was no defecation. The day of surgery was indicated as day 1. Patients submitted the forms within 1 week after surgery. At the time of submission, patients were questioned by the nurse on whether they had taken the analgesic as instructed.
Outcome measurements and grouping
The earliest VAS score of pain at defecation recorded during the 3 days was defined as the first defecation pain score, which was the primary outcome measure, and the consistency of stool at that defecation was defined as the first BSFS score, which was the secondary outcome measure. In this study, only the data on the first defecation were used, and no data on the second and subsequent defecations were used. The first BSFS scores of all patients were arranged in ascending order (1–7) and were classified into the hard, normal, and soft stool groups. To classify the data into the 3 groups as equally as possible, 2 boundaries were created using the cumulative percentage as a guide.
Statistical analysis
The Kolmogorov-Smirnov test was used to test the normality of all values. Data for which normality was confirmed are shown as mean± standard deviation, whereas data without normality are shown as median (range). The demographic parameters and first defecation pain score were compared among the groups as follows; although the hemorrhoid grade is an ordinal variable, it was regarded as a binary variable because only grade III and IV cases were included in this study. Similarly, sex and laxative use, which are nominal variables, were treated as binary variables. Pearson chi-squared test was used for the binary variables, hemorrhoid grade, sex, and laxative use. The Kruskal-Wallis test was used for the days of the first defecation, which is an ordinal variable. Of the interval variables of age, ALTA dose, duration of surgery, and first defecation pain score, the normally distributed variables of ALTA dose, duration of surgery, and first defecation pain score were subjected to Bartlett’s test for equality of variance followed by oneway analysis of variance (ANOVA) test, while age, which was nonnormally distributed, was subjected to the Kruskal-Wallis test. Previous study suggested that young age and male sex may affect the intensity of postoperative pain [9]. Therefore, these 2 variables were considered to be confounding factors of the first defecation pain score. An analysis of covariance (ANCOVA) test was used to control adjust confounding variables. In the ANCOVA for the young age group, 3 age groups (< 30 years, 31–45 years, and > 45 years) were used as covariates as in a previous study. Data were analyzed using IBM SPSS Statistics ver. 25 (IBM Corp., Armonk, NY, USA). For all analyses, a P-value of less than 0.05 was considered to be statistically significant.
RESULTS
Demographics and grouping
The study flow chart is shown in Fig. 2. The 2 patients who were not eligible had concomitant anal fissure. Among a total of 61 patients enrolled in this study, the first BSFS score was type 1 in 4, type 2 in 6, type 3 in 5, type 4 in 21, type 5 in 18, type 6 in 7, and type 7 in no patients. Because the cumulative percentiles for respective first BSFS scores were 6.6%, 16.4%, 24.6%, 59.0%, 88.5%, 100%, and 100%, respectively, the 2 boundaries for grouping were set as follows: the boundary between the hard and normal stool groups was between 3 and 4 and that between the ordinary and soft stool groups was between 4 and 5. As a result, 15, 21, and 25 patients were placed into the hard, normal, and soft stool groups, respectively. Patient demographics and clinical data are shown in Table 1.
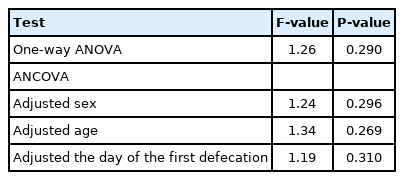
Correlation between stool consistency and first defecation pain
The first defecation pain score in 61 patients was 6.6± 2.2. The first defecation pain scores in patients who had the first defecation on day 1 (n= 20), day 2 (n= 33), and day 3 (n= 8) were 6.9± 2.5, 6.3± 2.0, and 7.7± 1.8, respectively. The Bartlett’s test results for ALTA dose, duration of surgery, and first defecation pain score demonstrated equality of variance (P= 0.70, 0.98, and 0.10, respectively). Fig. 3 shows that ANOVA detected no differences among the 3 groups in the first defecation pain score [F(2, 58) = 1.26, P= 0.29]. After adjusting for male sex, young age, or the day of the first defecation by ANCOVA test, there were still no significant differences among the 3 groups (Table 2).

Box plot of defecation pain scores in relation to degree of stool consistency. Median values (horizontal lines), interquartile range (boxes), range (error bars), and mean (cross marks) excluding outlier (circle) are shown.
DISCUSSION
This pilot study has 2 unique features. First, it focused on the first defecation after surgery, which is a concern for many patients; second, stool consistency was assessed using a measure called the BSFS. It is noteworthy that the results of this pilot study showed no apparent differences in the intensity of defecation pain among the hard, normal, and soft stool groups. The fact that the same result was obtained in the analysis after adjustment for previously reported confounding factors such as young age and male sex, may further increase the significance of the present study. The result of this study did not support the hypothesis that a harder stool causes a bigger pain. If future studies with enough sample size support the result of this study, the surgeons should stop using stool softeners to reduce pain.
Sphincter spasm close to the wound has previously been presumed to contribute to postoperative pain [10]. In this study, the wound has 2 different characteristics from the one in conventional hemorrhoidectomy. First, the incision size was half the conventional size due to internal hemorrhoids not being removed. Next, the present surgical procedure (reported previously as limited hemorrhoidectomy [11]) involves only 2 incisions unlike conventional hemorrhoidectomy, which requires 3 incisions. Although the wound in this study assumed to cause less spasm, it is interesting that the intensity of pain was no great difference from the previous reports [12, 13].
This study may have involved selection bias as this was a single-center study including day surgery cases only. Additionally, confounding bias cannot be ruled out because defecation pain has been investigated in only a small number of previous studies and confounding factors remain to be clarified.
This study had several limitations. First, only the first defecation was investigated. Second, the analgesics were assumed to be equally efficacious, although the length of time between medication and defecation varied among patients. Third, the surgical procedure used in this study was unique and not a commonly used procedure. Fourth, the sample size was small as this was a pilot study. Therefore, a large-scale study with adequate statistical power in which the conventional common hemorrhoidectomy procedure is performed and the length of time between administration of analgesics and defecation is measured needs to be conducted.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The author thanks Dr. Michio Asano for his useful advice.