Laparoscopic Hartmann reversal: experiences from a developing country
Article information
Abstract
Purpose
Laparoscopic surgery is considered a promising approach for Hartmann reversal but is also a complicated major surgical procedure. We conducted a retrospective analysis at a city hospital in Vietnam to evaluate the treatment technique and outcomes of laparoscopic Hartmann reversal (LHR).
Methods
A colorectal surgery database in 5 years between 2015 and 2019 (1,175 cases in total) was retrieved to collect 35 consecutive patients undergoing LHR.
Results
The patients had a median age of 61 years old. The median operative time was 185 minutes. All the procedures were first attempted laparoscopically with a conversion rate of 20.0% (7 of 35 cases). There was no intraoperative complication. Postoperative mortality and morbidity were 0 and 11.4% (2 medical, 1 deep surgical site infection, and 1 anastomotic leak required reoperation) respectively. The median time to first bowel activity was 2.8 days and median length of hospital stay was 8 days.
Conclusion
When performed by skilled surgeons, LHR is a feasible and safe operation with acceptable morbidity rate.
INTRODUCTION
The Hartmann procedure (HP), named after a French surgeon Henri Hartmann, was first described in 1921 as a technique for the treatment of rectal cancer [1]. This procedure included a sigmoidectomy and closure of the rectal stump ended with a terminal colostomy. Although Hartmann never considered the restoration of intestinal continuity, the closure of the colostomy with the open technique has been performed since 1950. This open Hartmann reversal (OHR) is still considered a major surgical procedure with a certain level of risk of significant morbidity. The rate of anastomotic leakage ranged from 4% to 16%, the mortality rate was up to 10%, and 46.5% of patients had postreversal complications [2-4]. In 1993, Lucchetta and De Manzini [5] and Anderson et al. [6] published the first report of a laparoscopic colostomy closure for previous HP. Some recent reviews showed that laparoscopic Hartmann reversal (LHR) brings several advantages over OHR, including fast postoperative recovery, less postoperative pain, earlier restoration of bowel function, and reduced morbidity [4, 7]. Since then, LHR has become more common and the procedure has been reported to be safer and easier than OHR. With the technical advantages such as circular stapler and laparoscopic surgery, it is easier to do adhesiolysis, localization of rectal stump, and anastomosis compared to OHR. This makes the Hartmann reversal (HR) possible even in the high-risk patient group. Moreover, LHR involves less intraoperative bleeding and a lower surgical site infection rate [7]. Our study examined the intraoperative and postoperative clinical outcomes of patients undergoing LHR in the Department of General Surgery at Nhan dan Gia Dinh Hospital in Ho Chi Minh, Vietnam.
METHODS
This study was approved by Institutional Review Board of Nhan dan GIa Dinh Hospital (No. 95-2019/NDGĐ-HĐĐĐ) and the patient’s written informed consent was obtained.
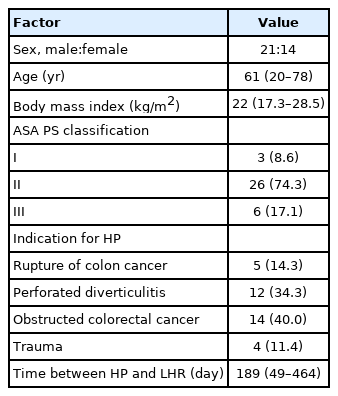
This is a retrospective, single-center study using a prospectively colorectal surgery database in 5 years (1,175 cases in total). We collected 35 cases in which LHR was performed at the General Surgery Department at Nhan dan Gia Dinh Hospital. These patients underwent HP between 2015 and 2019 for acute complicated diverticulitis, cancer, or trauma. Other indications for Hartmann revesal procedure were excluded. We did not include patients who had American Society of Anesthesiologists physical status classification IV or above, nor disseminated malignancy. Of the 35 patients who underwent LHR, there were 21 men and 14 women. The average body mass index was 22.5 ± 3.0 kg/m2. The time from the HP to the reversal procedure was at least 1 month with a median of 6.3 months (Table 1). We used both computed tomography scan and endoscopy to evaluate the remaining proximal colon and rectal stump and excluded any other condition such as polyps, diverticulum, or spread the malignancy. We performed rectoscopy stump to measure the length of the stump for reference. The length of rectal stump was not an indicator for choosing between open or laparoscopic LH. Mechanical bowel preparation and enemata were used for proximal colon and rectal stump respectively. Intravenous broad-spectrum antibiotics were given for prophylaxis as routine. Operative technical aspects and postoperative morbidity including medical or surgical complications were recorded.
Surgical procedure
Patients were placed in a supine position with legs spread apart and both arms along the body. Access into the abdominal cavity was gained through Hasson technique, with a 12-mm trocar at the right iliac fossa for scope. Pneumoperitoneum was then established. After adhesiolysis was done at the periumbilical site with a 5-mm trocar at the right upper quadrant, a 10 mm trocar was inserted at this site to be optic trocar for a 30° camera. Depending on the operative difficulty and location of adhesion we placed 3 to 5 trocars in total. The first surgical step was to free stoma and stump site by adhesiolysis. The peritoneal adhesion was described as mild, severe, and severe with angiogenesis based on adhesion grade score [8]. The small bowel was mobilized from the left iliac fossa and out of the pelvis to have space for anastomosis. The left gonad vessels and ureter were carefully identified. A circular stapler (CDH, Ethicon Endosurgery, Cincinnati, OH, USA) was used as a rectal probe to identify the rectal stump and to verify the actual possibility of creating a secure anastomosis. In some cases, we could not insert the CDH into the top of stump due to stricture of stump so we had to remove this stricture portion by endoscopic linear stapler. The reason for this stump stricture was not well understood, possibly due to poor blood supply in the stump. Rectal stump mobilization was systematically performed to ensure the feasibility of the end-to-end anastomosis and to avoid bladder injury. On the other hand, the splenic flexure mobilization was not performed routinely if the anastomosis was tensionfree. The stoma was then mobilized on the level of the abdominal wall and freed from the fascia. Subsequently, the colostomy was excised, and the bowel was mobilized out of the abdomen for anvil introduction and secured by a purse string. The circular staplers (CDH29, Ethicon Endosurgery) were the most frequently used. The bowel was returned to the abdominal cavity and a circular stapler was introduced into the rectum to make the anastomosis, and colorectal end-to-end anastomosis was performed without stoma diversion. In all procedures, a tension-free anastomosis was systematically obtained. A 24-French drain was placed in the pelvis. Complications were recorded during the postoperative course and up to 30 days after LHR.
RESULTS
Technical data
We performed laparoscopic surgery for all 35 cases. We did not use any hand-assist device but conversed to open to do the anastomosis after adhesiolysis laparoscopically in 7 cases. All the conversion cases were resulted in hand-sewn anastomosis due to severe adhesion and rectal stump stenosis. We used 3 trocars in 65.7% of patients. The adhesion of previous HPs was noticed in operation, there were 80% of cases having severe adhesion in the abdominal cavity. The mean operating time was 185 minutes. It was not necessary to perform splenic flexure mobilization routinely in our patients; this procedure was performed only when we observed the tension of anastomosis.
There was no intraoperative complication although the operation time was longer in patients with severe adhesion. None of the patients needed a blood transfusion in operation. All were allowed clear fluids beginning on postoperative day 2. Normal bowel activity was present within 2.8 ± 0.9 days. No patient required a temporary colostomy or an ileostomy. The length of hospital stay ranged from 5 to 22 days, with an average of 8.3 days (Table 2).
Morbidities and mortality
There was no death in our study. The morbidity rate was 11.4% including one deep surgical site infection and one anastomotic leak. The rate of surgical complication requiring reoperation and anastomotic dehiscence was 2.9%. There was no patient requiring a temporary colostomy or an ileostomy. In the case of anastomotic leak, we did HP again and HR was done 6 months later by laparotomy (Table 3).
DISCUSSION
The results of our study have demonstrated that laparoscopic reversal of HPs can be safe in the first instance in all patients, with the knowledge that conversion to open does not result in an increased risk of negative short-term outcomes. Moreover, laparoscopic reversal is beneficial for patients in terms of improved length of stay and 30-day morbidity. Many previous studies showed that the laparoscopic approach to HR should be considered when technically feasible and this approach was associated with fewer complications than open surgery [6, 9].
Many different laparoscopic techniques have been described in the literature, but the ideal laparoscopic fashion and the relative advantages of each procedure are still debated. Regarding the location of the first trocar, a 12-mm trocar at the right iliac fossa was chosen because HR was related to the left-sided colon, subsequently, there was limited even no adhesion in the right iliac fossa, avoiding trocar related complications when advancing periumbilical site trocar as well.
Lysis was the most important step in the LHR procedure and we spent most of the operative time on this step. In some cases with severe adhesion, we tried to lysis as much as we could to minimize the length of incision when conversion so the operative time was much longer than the other cases. The ideal time for the reversal is unknown, in our study the average time between HP and LHR was 27 weeks, while other authors confirmed that intraoperative difficulties appeared to be lower after a delay of 15 weeks from the index surgery [10].
From previous studies regarding LHR, the LHR principle can be divided into 2 groups of approaches including “stoma first” approach or “stoma the last” approach. In the stoma first approach, authors chose to take down the stoma first; the stoma site was used as a port for trocar or even single port insertion [11-14]. In our study, we chose to take down the stoma at the end of procedure to make sure everything ready for establishing anastomosis. Since there was a certain level of possibility of failure of reversal and permanent stoma in HR, this kind of approach could help to avoid making a new stoma when the reversal failed [3]. Conventional laparoscopy was applied to our patients instead of single port laparoscopy with the reason stated above. The conversion rate in our study was similar to other studies with the same technique but was better than series of single port LHR [13, 14].
Apart from the small sample size, our results may be similar to previous studies, which have an average mortality rate of 0.9% and an average anastomotic leak rate of 3.7% [3, 6]. Moreover, we had no intraoperative events and the conversion rate was acceptable.
In conclusion, our results are consistent with the previously published literature on the advantages of LHR over the OHR. When performed by skilled surgeons, LHR is a feasible and safe operation with an acceptable morbidity rate. However, our descriptive study with a small sample could not make any conclusion regarding the superiority of LHR. Nevertheless, higher level of evidence such as prospective studies from large multicenter on LHR and ORH is necessary to establish the conclusive judgment.
Notes
CONFLICT OF INTEREST
No potential conflicts of interest relevant to this article were reported.
FUNDING
None.