Long-term outcomes of high-volume stapled hemorroidopexy to treat symptomatic hemorrhoidal disease
Article information
Abstract
Purpose
The study aimed to assess the long-term results of the stapled hemorrhoidopexy (SH) using high-volume devices equipped with innovative technology, evaluating recurrence rate, complications rate, and patients’ satisfaction.
Methods
All the patients who underwent SH using high-volume devices (TST Starr plus, Touchstone International Medical Science Corp., Ltd.) for II to IV symptomatic hemorrhoidal disease from November 2012 to December 2014 were enrolled. Between December 2019 and January 2020, all of them were phone called to come to undergo a proctological reevaluation and asked to fill some questionnaires about hemorrhoidal prolapse recurrence, symptoms recurrence, and surgery satisfaction.
Results
Fifty-nine patients with a mean age of 47 years completely answered the questionnaires. Twenty-two of them accepted to come to undergo a proctological reevaluation while 27 preferred to answer only by phone due to their referred wellbeing. The median follow-up was 70.5 months (range, 60–84 months). The recurrence rate was 5.1% with a mean satisfaction level after surgery was 9.1 (range, 0–10) and 84.7% of patients whose satisfaction scored ≥8. The mean value of Cleveland Global Quality of Life assessment was 0.79 (range, 0.71–0.93). There were no cases of new onset of impaired anal continence after surgery.
Conclusion
The new generation high-volume devices to perform SH resulted to be safe and effective for II to IV degree hemorrhoidal prolapse leading to a lower long-term recurrence rate with an evident reduction of postoperative complications in comparison with the low-volume SH.
INTRODUCTION
Hemorrhoidal disease is one of the most common proctological diseases whose estimated prevalence rate is around 4.4%. Almost half of the 50 years old population experienced hemorrhoidal symptoms in their life [1], but only about 10% to 20% of them need surgery [2]. Since its first proposal by Longo in 1998 [3], circular stapled hemorrhoidopexy (CSH) has become an alternative to conventional hemorrhoidectomy for the treatment of symptomatic hemorrhoidal prolapse (HP). Several clinical studies have demonstrated that stapled hemorrhoidopexy (SH) is associated with less operating time, less pain, shorter hospital stay with an earlier return to normal activities and also improves symptoms of obstructed defecation that are frequently reported in these patients [4-12]. However, the recurrence rate and the need for further surgical procedures are higher if compared to the conventional hemorrhoidectomy [13-16]. Anyhow, these results come from the use of first-generation devices which had some limitations due to the low casing volume, whereby trying to improve the outcomes, new generation devices with high-volume casing were delivered on market [17]. The aim of the present study was to assess the long-term results of SH using a high-volume device (HVD) equipped with innovative technology, evaluating recurrence rate, complications rate, and patients’ satisfaction.
METHODS
All the patients undergone to SH using HVD (TST Starr plus, Touchstone International Medical Science Corp) for II to IV symptomatic hemorrhoidal disease from November 2012 to December 2014 were retrospectively analyzed taken the data from a prospectively maintained database. Between December 2019 and January 2020, all of them were phone called to come to undergo a proctological reevaluation and asked to fill some questionnaires about HP recurrence, symptoms’ recurrence, and surgery satisfaction.
lowing protocol; complete clinical evaluation with the medical history, physical examination, and anoscopy. Colonoscopy was preoperatively performed in case of rectal bleeding or age of > 50 years. Those patients who referred obstructed defecation syndrome (ODS) underwent further preoperative investigations such as X-ray defecography or dynamic pelvic magnetic resonance and anorectal manometry.
Indications to SH
Indication for SH to treat HD takes into consideration these 6 items: (1) anatomical presentation: circumferential HP associated to internal rectal prolapse; (2) type of symptoms: bother prolapse (independently from Goligher degree), bleeding and discharge; (3) frequency of symptoms: frequent (at least once per week) or always present (everyday); (4) associated diseases: ODS due to rectal intussusceptions and rectocele because it may improve if associated to the HP; (5) absolute contraindications: anal stenosis preventing an adequate circular anal dilator (CAD) placement and impaired anal continence; (6) relative contraindications: anticoagulant and/or antiplatelet therapy.
Surgical procedure
Spinal anesthesia was always preferred if there are no contraindications. Antibiotic therapy short-course was chosen using a single dose of third-generation cephalosporin and metronidazole before the beginning of the operation.
The surgical procedure is based on 8 steps [17]: (1) Introduction of the CAD. (2) Evaluation of the prolapse. (3) Fashioning a purse-string suture or use the parachute technique with 6 stitches at 1–3–5–7–9–11 o’clock. During this step as well as just before firing it is mandatory, in the women, to accurately control of the posterior vaginal wall using a vaginal valve thus preventing rectovaginal fistula. (4) Introduction of the stapler head beyond the suture. (5) Close the stapler and fire. (6) Open the stapler ad remove it. (7) Check the specimen. (8) Check the staple line and remove the CAD. Measure the specimen volume by putting it inside a 60-mL syringe containing 20 mL of saline solution and evaluating the final volume obtained.
Postoperative complications
Postoperative complications recorded were stratified according to Clavien-Dindo classification [18] and were hematoma, bleeding, urinary retention, persistent anal pain, anastomotic stenosis, tenesmus, and impaired anal continence which was evaluated through the Fecal Incontinence Severity Index (FISI) that ranges from 0 to 61 (0 is the best score) [19].
Long-term outcomes
The symptoms (bleeding, itching, burning, pain, and discharge) were investigated through a questionnaire already used [16] in which the frequency of symptoms was divided as follows; always, more than once a week, more than once a month, less than once a week, and never. Quality of life was investigated using the Cleveland Global Quality of Life (CGQL) focusing on 3 items [20]. Overall postoperative satisfaction about the procedure and postoperative course was evaluated through the following questions: “How much is your satisfaction for the surgical procedure and postoperative course on a scale from 1 to 10?”, “Would you undergo this surgery again?”, and “Would you recommend this type of surgery to a relative or a friend?”
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
RESULTS
Patients’ characteristics
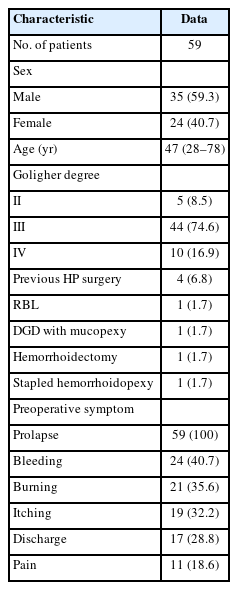
Sixty-one patients underwent SH with HVD in the investigation period but only 59 (female, 24; male, 35) with a mean age of 47 years (range, 28–78 years) completely answered the questionnaires. Twenty-two of them accepted to come to undergo a proctological reevaluation with digital examination and anoscopy while 37 preferred to answer only by phone due to their referred wellbeing. The patients’ characteristics were resumed in Table 1. All patients were affected by II to IV degree HP. The main symptoms associated with HP were daily bleeding (40.6%), burning (35.5%), itching (32.2%), discharge (28.8%), and pain (18.6%). The median follow-up was 70.5 months (range, 60–84 months). Four patients (6.8%) had a recurrent HP which was previously treated with 1 rubber band ligation, 1 Doppler-guided dearterialization with associated mucopexy, 1 hemorrhoidectomy, and 1 CSH.
Details for surgical features
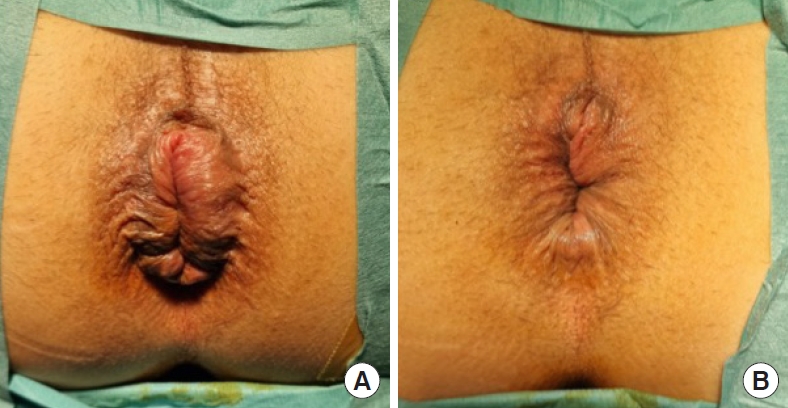
Mean operating time was 28.3 minutes (range, 15–60 minutes) without any significant intraoperative complications. In 1 patient (1.7%), there were some difficulties to introduce the CAD but achieving it anyway. In 55.9% there was the need for hemostatic stitches at the suture line level, with a mean of 2.4 stitches (range, 1–4 stitches) for each patient. The mean resected volume was 12.6 mL (range, 9–16 mL), and the mean length was 4.4 cm (range, 3.5–7.0 cm). All resected cylinders were complete and of full thickness. The mean hospital stay was 1.7 days (range, 1–7 days) with a readmission rate within the first week of 6.8% (n=4), due to postoperative bleeding. All details are resumed in Table 2 and in Fig. 1 preoperative and postoperative images of anus and HP are shown.
Postoperative complications
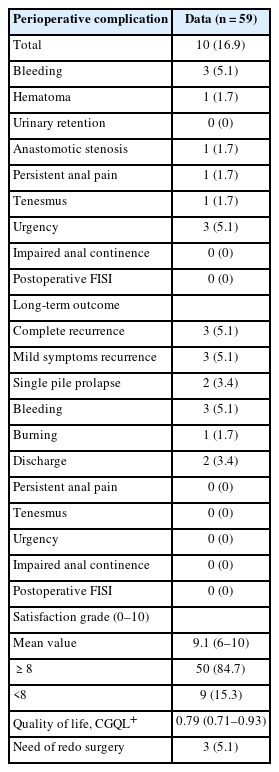
Overall perioperative complications rate was 16.9% (Table 3) with a serious adverse events rate of 5.1% whose course was favorable. The overall reoperation rate was 5.1%. All the complications were stratified according to Clavien-Dindo classification as follows: 4 of grade I, 3 of grade II, and 3 of grade IIIb. None of these had long-term consequences.
Postoperative bleeding rate was 5.1% with an overall bleeding reoperation rate of 1.7%. In 2 cases, it was mild and treated conservatively with medical therapy; instead, in 1 case, the patient needed a surgical revision. This patient subsequently developed a subclinical stricture which did not require any further treatment. In any cases, a blood transfusion was needed.
Pararectal hematoma occurred in 1 case (1.7%) and it was stable without active bleeding at the moment of readmission. Two days after it drained spontaneously at the staple line level and the patient, treated conservatively with fasting, parenteral nutrition, and antibiotic therapy, was then discharged 8 days after in good clinical conditions without any further complications.
Tenesmus rate was 1.7% and it was treated with topical medications (nonsteroidal anti-inflammatory) for 30 days and it completely resolved within 3 months after surgery. Urgency, instead, was reported in 10 patients (16.9%) at 7 days after surgery. Of these, 3 patients resolved symptoms at 1 month and 4 patients within 3 months after surgery. At 12-month follow-up, only 5.1% reported urgency, and 1 of them was affected by fibromyalgia; but none of them reported urgency at 5-year follow-up. There was not any new onset of perioperative anal incontinence with FISI score of 0.
Persistent anal pain rate was 1.7% caused by a rigid suture fixed on the deep planes at the level of puborectalis muscle ad it was quickly treated (within 6 months as already reported) [21] removing tracts of a rigid suture with a complete symptoms resolution thereafter.
There was only 1 case (1.7%) of anastomotic stenosis which was treated firstly with outpatient dilatation and then due to the symptoms’ persistence, a redo surgery was performed at 5 months after surgery removing part of the stenotic stricture with complete symptoms resolution.
Long-term outcomes
The recurrence rate was 5.1% (n=3) and all of them required reoperation because they were non-responders to the medical therapy. The surgeries performed were 2 hemorrhoidectomies and 1 redo SH carried out between 4 and 5 years after the first procedure. Among the other patients, after a follow-up lasted at least 5 years, only 5.1% referred mild anatomical (1 single pile in 3.4%) and symptomatic recurrence (bleeding of 5.1%, burning of 1.7%, and discharge of 3.4%) which were treated at first with medical therapy but in 2 cases, due to the persistence, outpatient treatment was performed with a complete symptoms’ resolution.
The mean satisfaction level after surgery was 9.1 (range, 0–10) with 84.7% of patients whose satisfaction scored ≥ 8. Moreover, 81.3% stated that they would recommend this kind of surgery to a friend and/or relative and 89.8% would also undergo this surgery again. The mean value of CGQL assessment was 0.79 (range, 0.71–0.93). Preoperative FISI score was 0 due to the inclusion/exclusion criteria above mentioned. The long-term postoperative FISI score remained 0 without any anal incontinence new onset.
DISCUSSION
Several studies as well as the recent guidelines [4] have reported that SH is a safe and effective surgical treatment for HP. Indeed, SH is a quick procedure characterized by less operating time, shorter hospital stay, and earlier return work if compared with the conventional treatment. These good postoperative results are related to less postoperative pain, better wound healing, and earlier bowel function recovery which are the strengthen points of SH and frequently fit the preoperative requirements of patients. However, the postoperative outcomes of the first-generation devices could be considered disappointing regarding the recurrence rate and the overall complication rate [16]. These results were related to the intrinsic limitations of the device because of the low casing volume. To overcome this condition, it was needed to use a double stapler to resect an adequate amount of prolapse. But, if from a side the double stapler hemorrhoidopexy (DSH) properly treats the prolapse [22], from the other side has some weak and fixed points at the crossing suture which may influence the final results. To improve the final results avoiding the flaws of low-volume CSH and DSH, the HVD was introduced [17]. The preliminary and early outcomes were really impressive [23] and the present study confirmed them in a long-term period.
The many advantages of HVD are that it is a simple procedure resulting to be easier than DSH thus reducing the likelihood of technical error. It also allows a better view and control of the operative field without any more blind surgery. This result was achieved thanks to a better technology of the device with new patents which guaranteed optimal head stability avoiding staples misalignment during fire without any barrier inside the casing space. Furthermore, the use of only 1 device instead of 2 as in the case of DSH to resect the same prolapse amount is inevitably linked to a significant costs reduction.
In the present paper, the recurrence rate was 5.1% and it is very similar to other HVD rates reported [24]. However, it is sharply lower if compared to the conventional CSH in which it can reach up to 50% [12, 25] and it is also related to a very high patients’ satisfaction rate.
The reported range of the overall recurrence rate is frequently fairly wide, possibly indicating the lack of a clear definition of recurrence. Where some authors consider only the cases which show a complete relapse of the preoperative anatomy and symptoms some others count any case that includes the partial or total return of preoperative condition (anatomic, symptomatic, or both).
Moreover, concerning the recurrence rate, it is surprisingly unclear how in some studies transanal hemorrhoidal dearterialization/hemorrhoidal artery ligation and rectoanal repair show similar or even better results when compared to SH for the same cluster of patients [26, 27]. Theoretically, SH should hang the hemorrhoids higher than what the mucosuspension can reach, and interrupts the down-streaming arterial flow more efficiently than single or multiple arterial ligations may do using absorbable sutures.
The perioperative overall complication rate considering all the possible postoperative discomfort and bother symptoms was 16.9% which is less than that reported by Tjandra and Chan [11]. Analyzing in detail, none of them had long-term effects because they resolved spontaneously or using medical therapy. Only 5% required a surgical revision. The overall serious adverse events rate was less than that reported by Watson et al. [28] in eTHoS trial.
Postoperative bleeding rate was 5.1% less than the 21.7% reported by Goldstein et al. [29] with only 1 case needing reoperation. In this series, it was reported 1 case of potential life-threatening complication such as pararectal hematoma which has anyway a favorable course. However, the authors want to underline the importance of knowing the possible complications and how to manage them supported by the availability of interventional radiologist service in case of necessity [17].
The incidence rates of persistent anal pain and anastomotic stricture were both 1.7% similar to the values already published in the literature even if some authors reported rates over 15% [30].
The perioperative tenesmus rate was 1.7% but later on completely disappeared. These data are very different from the rate of 48% at 2 years follow-up as previously published [28]. Furthermore, as well as also for the long-term urgency and impaired anal continence, in the present series there was not any patient complaining of these bother and quality-of-life limiting complications as for other series [24]. This is probably due to strict selection criteria associated with the use of HVD allowing a regular circular rectal excision associate with a wide anastomosis.
The present study has some limitations due to the lack of proctologic reevaluation in half of the patients and also the use of a non-validated questionnaire to assess long-term symptoms presence or modification.
Hence, the new generation HVD to perform SH resulted to be safe and effective to treat symptomatic II to IV degree HP following the above-mentioned indications. It showed to have less operating time, less pain associated with shorter hospital stay, and faster return to normal activities if compared with the conventional hemorrhoidectomy [4]. The innovative technology with a new conformation allows better intraoperative visualization and a tailored prolapse resection according to the intraoperative evaluation. All these characteristics lead to a lower long-term recurrence rate with an evident reduction of postoperative complications in comparison with the low-volume SH.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.