Radiofrequency ablation (Rafaelo Procedure) for the treatment of hemorrhoids: a case series in the United Kingdom
Article information
Abstract
Purpose
Hemorrhoidal disease remains a common condition that can have a significant effect on a patient’s quality of life. Various methods have been introduced over the years; however, their overall success rates remain low. Although the traditional Milligan Morgan technique is effective, the associated pain level prevents it from being an attractive form of treatment. This study was devised to assess the safety and efficacy associated with a novel minimally invasive approach, radiofrequency ablation (RFA).
Methods
Forty-two patients underwent RFA at a single center, by 1 of 2 surgeons. This was performed under local anesthetic and sedation. Outcomes including postoperative pain levels, recurrence rates, and patient satisfaction scores were recorded and analyzed using medians and interquartile ranges
Results
The median postoperative pain score was 2.5/10 (interquartile range [IQR], 0–4.5) and the overall patient satisfaction score was 9 out of 10 (IQR, 6.5–10). Recurrence rates (6–12 months following the procedure) were low at 12% and all patients reported milder symptoms at recurrence. There were no serious adverse complications
Conclusion
The results from this case series supports other limited data in concluding that RFA is a safe and effective method in the treatment of hemorrhoids and patients report a high level of satisfaction following
INTRODUCTION
Hemorrhoids have a high prevalence among the international population, resulting in symptoms such as bleeding, itching, pain, and prolapse. It is estimated that 50% of the population has hemorrhoids by the age of 50 years [1]. Although prevention remains better than cure, once established, the condition can be difficult to treat effectively and definitively. Optimal treatment remains under debate and new techniques and instrumental tools continue to be introduced to reduce postoperative pain and complications, including longer-term recurrences.
For grade I to II hemorrhoids, rubber band ligation (RBL) has been the initial mode of therapy. The results are superior to those of injection sclerotherapy [2] and the procedure can be carried out in the outpatient setting with no anesthetic. Single versus multiple RBL was investigated in 2 randomized studies and triple RBL was found to be more cost-effective with no increase in complication rate [2]. More recently, hemorrhoidal artery ligation (HAL) was introduced and the HubBLe Trial [3] demonstrated that there were fewer recurrences at 1 year with the HAL compared to RBL; however, the results were similar when compared with repeat RBL. There are not yet any studies that demonstrate long-term outcomes (> 3 years) with the HAL procedure.
In prolapsing grade III–IV hemorrhoids, the traditional Milligan Morgan hemorrhoidectomy (derived in 1937) has high success rates in minimizing recurrence; however, prolonged postoperative pain and recovery time are common complications [4]. This reduces overall patient satisfaction scores. Most patients would prefer a less invasive modality of treatment if given the option.
Radiofrequency ablation (RFA) is slowly being introduced as a potentially faster and less painful treatment than other methods. Radiofrequency is a type of electrical energy. RFA uses heat made by radio waves to thermally destroy tissue cells. The alternating current generates changes in the direction of ions within the tissue fluid. This creates ionic agitation and frictional heating, leading to coagulative necrosis of tissue. Long-term, in hemorrhoidal disease, this achieves plication of anorectal mucosa and improved symptoms. Although RFA is a novel approach for hemorrhoidal disease, it has been successfully used to treat other conditions such as varicose veins and Barrett’s esophagus/dysplasia. Studies looking at outcomes of RFA in hemorrhoidal disease are limited. This is the largest case series reported in the United Kingdom, with a total of 42 patients who were treated at a single site, by 1 of 2 consultant colorectal surgeons.
METHODS
This study included 42 patients who underwent the Rafaelo Procedure (Modern Aesthetics Solutions Ltd) which uses the established technology of RFA for grade I to III hemorrhoids in a hospital by 1 of 2 colorectal consultants. The surgical method was standardized between both consultants performing the procedure and is described below. The treatment was performed under local anesthetic with minimal propofol sedation in the left lateral position. All procedures were carried out as day cases and patients were sent home with simple analgesia including 7 days of paracetamol +/– ibuprofen.
Prior to the procedure, the standard patient data was gathered including age, sex, comorbidities, symptoms, and their impact on patient quality of life (QoL). Intraoperative data including the number of hemorrhoids treated, hemorrhoidal positions, energy levels used, and complications were all recorded for each patient. The dataset was statistically analyzed using medians and interquartile ranges. All the patients consented for inclusion into the study.
Rafaelo Procedure
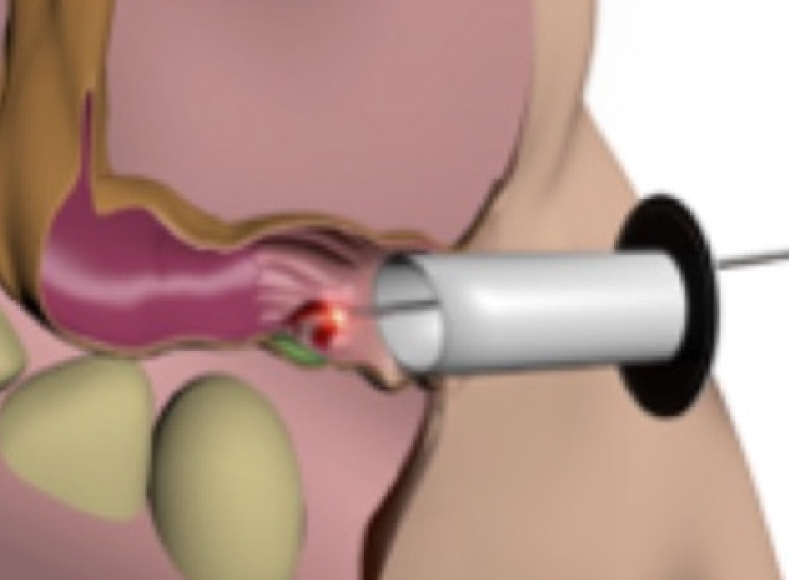
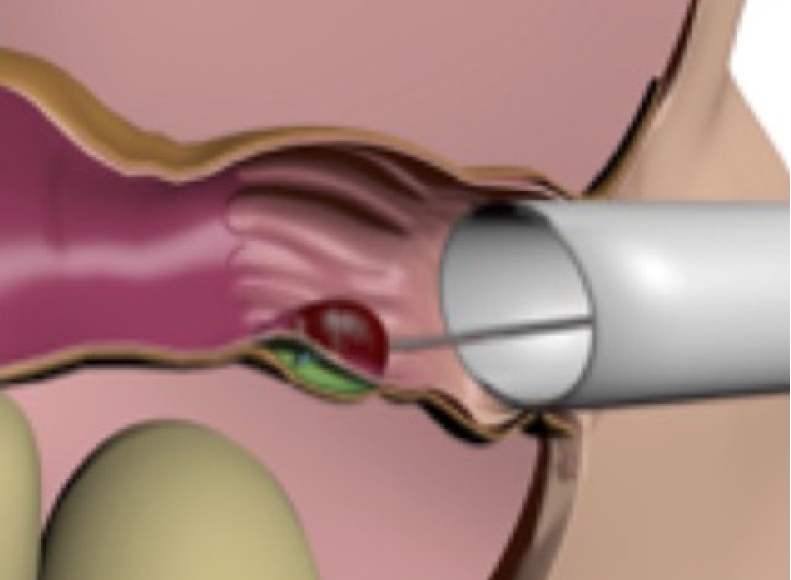
A lubricated proctoscope is inserted into the anal canal, allowing good visualization of the hemorrhoids. Local anesthetic is inserted into the submucosal plane of each hemorrhoidal tissue (Fig. 1). This provides a fluid barrier to protect the internal anal sphincters against the transmission of heat, as well as providing a local anesthetic effect. A specially designed probe (Rafaelo HPR45i) connected to a radiofrequency generator is then inserted into hemorrhoid causing the tissue to heat up, and hemorrhoid to become necrotic and shrink (Fig. 2). The HPR45i probe allows good visualization of the tissues and the radiofrequency signal to be applied onto the tip of the probe when the generator is activated. The length of the probe measures 210 mm and the tip measures 10×2 mm.
Injection of local anesthetic into the submucosal plane of the hemorrhoid. Permission for image taken from Mark Plass at Modern Aesthetics Solution Ltd.
Follow-up
All patients were followed up 6 to 8 weeks postoperatively in the outpatient clinic, and 6 to 12 months later by telephone consultation. At the latter stage, a patient questionnaire regarding postoperative pain level and procedure satisfaction score were recorded using the Likert scale.
RESULTS
Forty-two patients were treated with RFA between March 2017 and December 2018 at Dunedin Hospital in Reading, UK. Patient demographics are listed in Table 1. Number and grade of hemorrhoids treated, mean energy levels, and time of energy application are shown in Table 2. The 2 main symptoms that patients complained of were bleeding (28, 66.7%) and pain/discomfort (29, 69.0%). Other symptoms included mucus discharge (1, 2.4%), itching (10, 23.8%), prolapse (4, 9.5%), and urgency/incontinence of feces (2, 4.8%). When asked to quantify the effect of these symptoms on QoL using the Likert scale (0–10, 10 being maximum impact on QoL), the median score was 7 (IQR, 6–8.25).
Following the procedure, the median pain score (0–10, 10 being maximum pain) was 2.5 (IQR, 0–4.5) and this lasted 5 days on average. The patients of 33% required simple analgesia postoperatively. The patients of 38% reported no pain in both the immediate and initial postoperative weeks following surgery. Nine patients had already undergone previous HAL and comparatively, the median associated pain score was reported as 8 out of 10. Overall, the median satisfaction score with RFA was 8.4 out of 10 (IQR, 6.5–10) (Table 3).
There were no significant postoperative complications. The readmission rate was 4.8%. One patient was admitted for postoperative bleeding that settled without intervention, and 1 patient was admitted for pain management. Neither required an overnight hospital stay.
DISCUSSION
The purpose of this study was to test the safety and efficacy of the Rafaelo Procedure in a single cohort of patients with grade I to III hemorrhoids. This is the largest case series reported in the United Kingdom. The results illustrate a median pain score of 2.5 out of 10 with only 1/3 patients requiring postoperative analgesia. Only 1 patient returned to the hospital with pain that was not controlled with conventional analgesia. Patients were followed up at 6 to 12 months to allow a reasonable period of time for symptom recurrence. Five patients (11.9%) required further operative management within this period; however, all but 1 of these patients described milder symptoms at recurrence. All patients who required further treatment had grade III hemorrhoidal disease. The reasons for recurrence in these patients were felt to be multifactorial including high-grade disease, and lifestyle factors, such as dietary intake and infrequent bowel motions. The Rafaelo Procedure can be performed in stages for larger hemorrhoids. In conclusion, within this study group, the Rafaelo Procedure has been used safely in both primary and recurrent hemorrhoidal disease with no serious complications.
The literature was reviewed and compared to the results of this study. A recent case series in Cologne looked at 102 patients with grade III hemorrhoids undergoing the Rafaelo Procedure [5]. Their results also support the procedure being safe with no undesired effects. Their patient symptom score dropped from 9.9 to 1.1 after 3 months and pain levels were similar to our reported patient cohort. A polish center has also used the Rafaelo probe in a total of 4,000 interventions with no reported adverse complications (not yet published) [5]. The long-term results of both studies are not yet known. A more recent publication of results in the United Kingdom (Eddama et al. [6]) reports results in 27 patients and has shown a significant reduction in symptoms postprocedure. Their satisfaction scores match those found in our patient cohort.
Much of the other data regarding RFA in hemorrhoidal disease has been published in India. Two randomized trials were conducted; one comparing RFA with band ligation [7] and the other comparing RFA with the Milligan Morgan technique [8]. Both studies were small, with patient numbers under 60. However, they both concluded that RFA is a safe method of treatment for patients with grade II to III hemorrhoids. They also reported lower postoperative pain scores and no serious adverse complications of RFA were documented, such as anal stenosis, incontinence, or wound sepsis.
The strengths of this study include a reasonable-sized case series, with a standardized operative method carried out by a limited number of surgeons. This reduces variability in technique. Clinic follow-up was also standardized, and individual telephone consultations were made to avoid losing patient to follow up, which enables a complete dataset for analysis. Limitations include possible recall bias, the fact this is a single centered study, and that there is no comparable treatment group.
This study supports other limited data in assurance that RFA is a safe and acceptable method of treatment for hemorrhoidal disease. Although the satisfaction scores are promising, further randomized controlled trials are needed to confirm the true efficacy of this method. A further trial is currently being conducted within this same center to assess pain levels and satisfaction scores with RFA treatment under local anesthetic without sedation in the outpatient setting.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: RB, SM; Data curation: SH, DM, SM; Formal analysis: SH; Investigation: SH; Methodology: SH, DM, SM; Project administration: all authors; Supervision: SM; Validation: DM, SM; Visualization: SH, DM, SM; Writing–original draft: SH; Writing–review & editing: DM, RB, SM. All authors read and approved the final manuscript.