Strangulated internal hernia through a defect of the broad ligament: a case report of laparoscopic surgery
Article information
Abstract
An internal hernia is defined as the protrusion of an internal organ through a defect in the abdominal cavity. Broad ligament hernia (BLH) is an extremely rare type of internal hernia that is difficult to diagnose preoperatively because the symptoms are nonspecific. However, early diagnosis is crucial, and early surgery is required to reduce complications such as strangulation. Laparoscopy has the advantage of enabling simultaneous diagnosis and treatment of BLH. With the advancement of the laparoscopic techniques, several cases of laparoscopic treatment of BLH have been reported. Nevertheless, open surgery is primarily performed in patients requiring bowel resection. We present a case of laparoscopic surgery for a strangulated internal hernia through a broad ligament defect. We successfully resected the strangulated small intestine and closed the defect of the broad ligament laparoscopically with a minor incision.
INTRODUCTION
An internal hernia is defined as the protrusion of an internal organ through a defect in the abdominal cavity. Broad ligament hernia (BLH) is an extremely rare type of internal hernia. Quain [1] first reported a case of BLH in 1861, often called “Quain hernia.” In 1955, Allen and Masters [2] introduced a series of cases of broad ligament defects called Allen-Masters syndrome.
BLH is difficult to diagnose preoperatively because the symptoms are nonspecific. Computed tomography (CT) is useful for diagnosis, and BLH may be suspected when closed-loop obstruction is observed near the uterus. Early diagnosis is crucial and early surgery is required to reduce complications such as strangulation [3]. Laparoscopy has the advantage of enabling simultaneous diagnosis and treatment of BLH. We present a case of laparoscopic surgery for a strangulated internal hernia through a broad ligament defect.
CASE REPORT
A 57-year-old woman with no medical or surgical history was referred to the emergency department of Chungnam National University Sejong Hospital (Sejong, Korea). She complained of abdominal pain without vomiting or diarrhea. On physical examination, her abdomen was soft and slightly distended, and bowel sound was decreased. Mild tenderness was observed in the lower abdomen, without rebound tenderness. The patient’s initial vital signs were stable and within normal limits, except for elevated blood pressure (165/95 mmHg). Laboratory findings were unremarkable and within normal ranges. Contrast-enhanced CT was performed, and a small bowel loop with decreased wall enhancement was detected next to the uterus (Fig. 1). Abdominal pain and decreased wall enhancement of the small bowel on CT scan indicated intestinal ischemia. Therefore, we diagnosed it as a closed-loop obstruction with intestinal strangulation and decided to perform an emergency surgery. As she had mild abdominal distension and her vital signs were stable, we determined to try laparoscopic access. The operative plan was to inspect laparoscopically, and then to decide whether to continue the laparoscopic surgery or converse to open surgery.

Computed tomography findings. (A, B) Small bowel loop with decreased wall enhancement was detected next to the uterus (arrows).
The patient was placed in the supine position under general anesthesia. A 10-mm balloon trocar was introduced through the umbilicus using the Hasson technique, and a carbon dioxide pneumoperitoneum was induced. A 10-mm laparoscope was inserted through the balloon trocar and two 5-mm trocars were introduced in the right upper and lower quadrants under laparoscopic guidance. The entire abdomen was examined laparoscopically, and a strangulated small intestine herniated through the left broad ligament of the uterus was detected (Fig. 2A). An additional 5-mm trocar was introduced into the left middle abdominal area. After widening the defect using electrocautery, the adherent small intestine was dissected (Fig. 2B). The defect in the broad ligament was oval in shape with a diameter of approximately 3 cm (Fig. 2C). The defect was closed using a nonabsorbable barbed 3-0 suture (Fig. 2D). Mini-laparotomy was performed by extending the umbilical wound. The dissected small intestine was taken out through the injury. Approximately 15cm of the small intestine was necrotic. Segmental resection of the necrotic small intestine was performed using linear staplers, followed by end-to-end hand-sewn anastomosis. The anastomosed small intestine was placed into abdominal cavity, and the wound was closed. The total operative time was 133 minutes, and the laparoscopic time was 37 minutes.
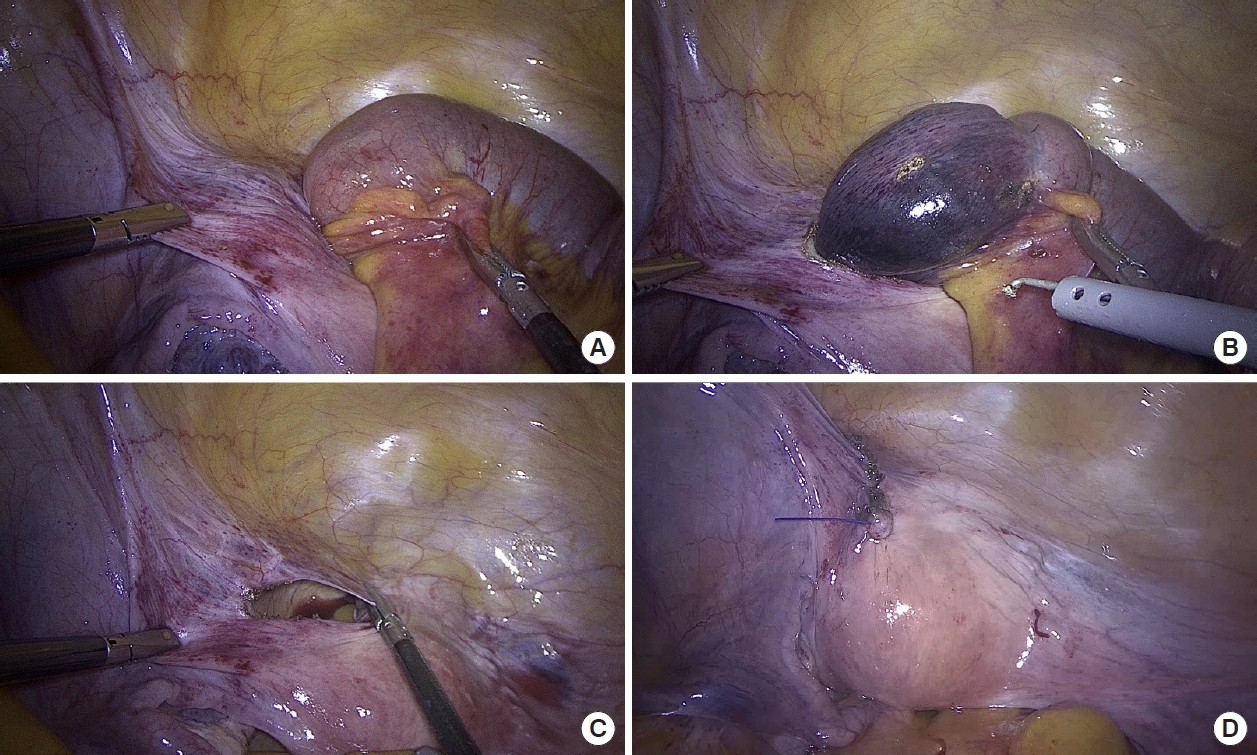
Laparoscopic findings. (A) Strangulated small intestine herniated through the left broad ligament of the uterus. (B) After widening the defect using electrocautery, the adherent small intestine was dissected. (C) The defect in the broad ligament was oval in shape with a diameter of approximately 3 cm. (D) The defect was closed using a nonabsorbable barbed 3-0 suture.
On postoperative day (POD) 2, the patient complained of severe abdominal pain and distension. Her vital signs were stable and within normal limits, except for mild fever (37.9°C) and a C-reactive protein of 25.2 mg/dL. Radiography revealed distension of the stomach and small intestine, suggesting postoperative ileus (Fig. 3). A nasogastric tube was inserted, and approximately 200 mL of greenish content was drained. After conservative treatment, the nasogastric tube was removed on POD 7. She tolerated a soft diet on POD 11 and was discharged on POD 13. The biopsy revealed a mural infarction with hemorrhage.

Radiologic finding on postoperative day 2. Distension of the stomach and small intestine, suggesting postoperative ileus.
Ethics statement
This case report was approved by the Institutional Review Board of Chungnam National University Sejong Hospital (No. CNUSH 2023-02-018). The requirement for informed consent was waived by the Institutional Review Board.
DISCUSSION
There are 2 classifications of BLH. Hunt [4] introduced a classification based on the degree of the defect, which includes the fenestra and pouch types. Our case was the fenestra type, with a complete 2-layer deficiency of the broad ligament. Cilley et al. [5] classified BLH into 3 types based on the anatomical location of the defect. According to Cilley’s classification, our case was a type 1 defect, caudal to the round ligament.
If BLH is suspected, diagnostic laparoscopy should be performed immediately, regardless of the type. The first case involving laparoscopic repair of a BLH was published in 2003 [6]. Subsequently, several cases of laparoscopic BLH treatment were reported. Most cases treated with laparoscopy were incarcerated BLH without strangulation; however, in cases requiring bowel resection, open surgery was mainly performed [7–10]. To our knowledge, only 1 case of laparoscopic surgery for strangulated BLH has been reported [11]. In the present case, the decision to perform laparoscopic surgery was based on a number of factors, including the patient’s clinical presentation and imaging findings, as well as the surgeon’s experience and expertise in laparoscopic procedures. Laparoscopic surgery offers several advantages over open surgery, such as shorter hospital stay, less postoperative pain, and faster recovery. We successfully resected the strangulated small intestine and closed the defect of the broad ligament laparoscopically with a minor incision.
In conclusion, BLH should be considered in women with no history of abdominal surgery and small bowel obstruction near the uterus. Laparoscopy is an effective method for the diagnosis and treatment of BLH.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: JSK; Formal analysis: JHS; Investigation: all authors; Methodolgy: JSK; Project administration: JSK; Supervision: JSK; Validation: JSK; Visualization: JSK; Writing–original draft: JHS; Writing–review & editing: all authors. All authors read and approved the final manuscript.
