Comments on “Laser hemorrhoidoplasty versus conventional hemorrhoidectomy for grade II/III hemorrhoids: a systematic review and meta-analysis”
Article information
Dear Editor,
We have read with great interest the systematic review and metaanalysis about laser hemorrhoidoplasty versus conventional hemorrhoidectomy for grade II/III hemorrhoids, published by Wee et al. [1], and we congratulate the authors on this valuable study. However, we have some comments on the methodology of this systematic review and meta-analysis.
The authors investigated heterogeneity using the I2 statistic. The value of I2 was interpreted as quantifying inconsistency. However, this concept is not accurate, and Wee et al. [1] did not cite any sources for using this concept to assess heterogeneity. Higgins et al. [2] reported this modality, which remains an opinion of an expert (level 5 of evidence according to the Oxford classification). After a few years, in 2017, Borenstein et al. [3], published a new article entitled “I2 is not an absolute measure of heterogeneity” to address the problem of using this modality of heterogeneity assessment. Instead, heterogeneity should be assessed by the 95% predictive interval, which presents variation in the true effect size (4, 5), and its variance (Tau2).
As concerns the model used to measure the effect size, a random-effects model was chosen when the I2 statistic was greater than 50%, and a fixed-effects model otherwise. The results were reported with 95% confidence intervals, and a P-value of less than 0.05 was treated as statistically significant. Generally, a random-effects model is often considered the appropriate choice for capturing uncertainty resulting from heterogeneity among studies. However, this concept is also not accurate. When dealing with different populations, a random-effect model must always be applied, whatever the I2. Indeed, there is no place for the fixed-effect model in this context [4]. In addition, for the retained studies, we would like to point out that the article by Maloku et al. [5] is a high-quality study with a large sample size, and a fixed-effect model provides a greater weight to larger pooled studies than to studies with a small sample size [6, 7]. We think that for this reason, it would be more accurate to present the forest plot comparing early postoperative bleeding (Fig. 3 in Wee et al. [1]) using a random-effects model because the weight of the study of Maloku et al. [5] was reported to be 67%. To improve accuracy, the authors should use the odds ratio instead of the risk ratio because they included randomized and nonrandomized clinical trials. When we recalculated the data, we found lower bleeding in the laser hemorrhoidoplasty group (odds ratio, 0.12; 95% confidence interval, 0.04–0.42; P < 0.001) and low heterogeneity among the different studies (Fig. 1).
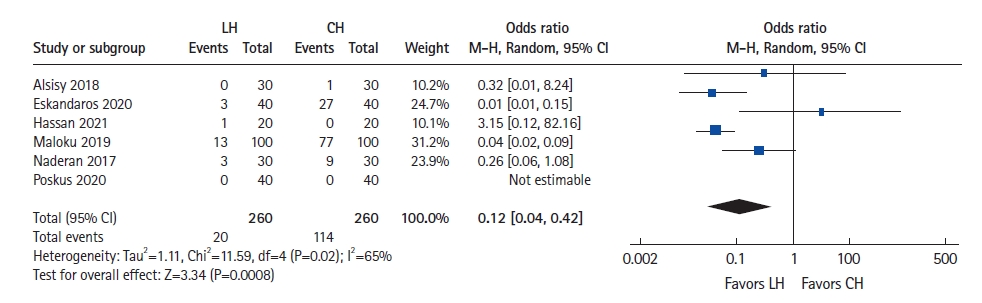
Forest plot comparing early postoperative bleeding between laser hemorrhoidoplasty (LH) and conventional hemorrhoidectomy (CH). M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval.
In addition, we would like to point out several mistakes in the different figures presenting forest plots. The authors referred to the experimental group as “H”; however, they used “LH” as an abbreviation for “laser hemorrhoidoplasty.” In addition, in the control group, we found “open surgery” or “hemorrhoidectomy” referring to “conventional hemorrhoidectomy,” which was abbreviated as “CH.”
We believe that these corrected results should be brought to the readers to prevent incorrect interpretations of these findings.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
