Chronic fistula in ano associated with adenocarcinoma: a case report with a review of the literature
Article information
Abstract
The malignant transformation of chronic fistula in ano is rare, accounting for 3% to 11% of all anal canal malignancies. It results from long-standing inflammation and chronic irritation. No guidelines are available for the management of these cases. We herein present a case report of a 55-year-old man who presented with a history of constipation, perianal pain, and discharging fistula in ano of 4-year duration and underwent fistula surgery with recurrence. Biopsy of the fistulous tract revealed adenocarcinoma. He received neoadjuvant chemoradiotherapy, followed by abdominoperineal excision including excision of the fistulous tract. After 18 months of follow-up, he is free of recurrence. We present this case with a review of the literature, highlighting the management strategies.
INTRODUCTION
Fistula in ano (FIA) is a common disease in proctology clinics. However, adenocarcinoma in the setting of chronic FIA is rare, accounting for 3% to 11% of all anal canal malignancies [1]. Malignant transformation of FIA was first reported by Rosser [2] in 1934, and since then, only a few case reports and case series have been published in the literature. The genesis of adenocarcinoma results from dysplastic changes in a chronic or recurrent fistula or the infiltration of a fistula by malignant cells arising from the colorectal epithelium [3]. The diagnosis is often delayed, because it mimics a benign condition and there is a social stigma associated with anorectal disorders. In a case of nonhealing chronic FIA, a high index of suspicion should be kept for a possible malignancy. Despite low-grade histology, these neoplasms are locally aggressive in nature. Most patients require extensive surgery, which often necessitates flap closure. However, because of inflammation, it is difficult to assess the local extension of the tumor, resulting in a relatively high risk of local recurrence [4]. Some series have shown favorable outcomes with neoadjuvant treatment, followed by radical surgery [5, 6].
The outcomes of anorectal malignancies have improved during the last decade due to a better understanding of the disease, better neoadjuvant and adjuvant therapy, and the standardization of surgery. Herein, we present a rare case of the malignant transformation of chronic FIA, along with a review of the literature regarding its management.
CASE REPORT
A 55-year-old man presented with FIA that had lasted for 4 years. He had associated constipation and occasional pain at the fistula site. There was no history of bleeding per rectum, mucous discharge, or tenesmus. He had new-onset anorexia, generalized weakness, and a loss of body weight for 4 months. He had undergone anal fistulotomy at a primary health care hospital, and biopsy of the excised tissue revealed mucinous adenocarcinoma. The patient was then referred to a tertiary care hospital for further management. His general physical examination and abdominal examination were essentially normal. A perianal examination showed a pus-mixed mucous discharge from the FIA with external openings at the 8- and 11-o’clock positions (Fig. 1). An indurated, nontender swelling was palpable around the external opening. A firm, submucosal bulge was palpable, extending from the 6- to 12-o’clock positions just above the anal verge, and the mucosa over it was freely mobile. No internal opening could be visualized. His respiratory and cardiovascular system examinations were normal. Blood investigations were normal and human immunodeficiency virus (HIV) serology was negative. Serum carcinoembryonic antigen (CEA) was 3.62 ng/mL (reference range, <3 ng/mL). Complete colonoscopy revealed normal colonic and rectal mucosa with a bulge in the lateral wall. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis demonstrated an enhancing lesion in the perianal area around the fistulous tract, extending from the anal verge to the mid-rectum. Subcentimetric mesorectal nodes were present, which were radiologically insignificant, and postoperative histopathology showed only discrete tumor deposits (N1c). There was no evidence of dissemination. The case was reviewed at a multidisciplinary tumor board (MDT) meeting; however, there was no guideline available for the management of this condition. Thus, based on previous case reports and series and institutional experiences of adenocarcinoma in the lower rectum, neoadjuvant chemoradiotherapy and chemotherapy were planned.
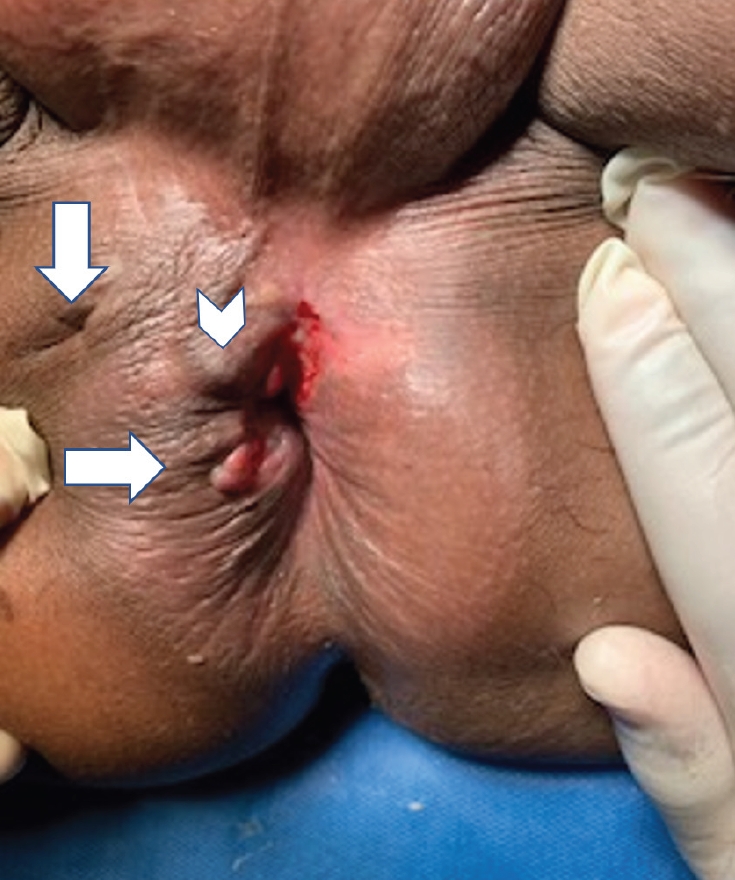
Perianal area showing fistula in ano with external openings at 8- and 11-o’clock (arrows) and an indurated area (arrowhead).
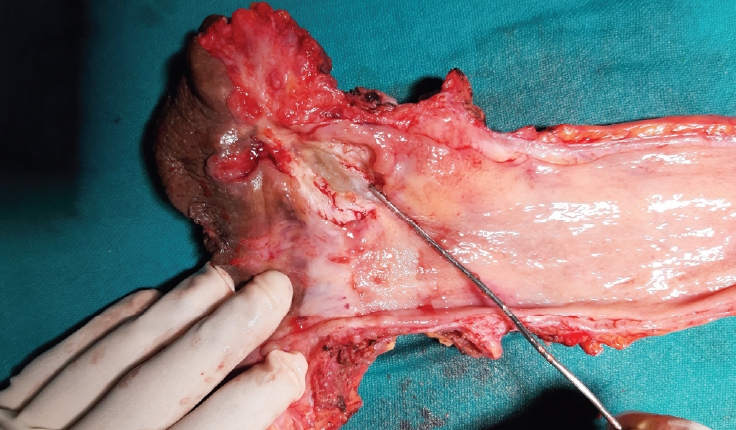
The patient received neoadjuvant concurrent chemoradiotherapy (45 Gy in 25 fractions of radiotherapy, as well as oral capecitabine) followed by chemotherapy (4 cycles of capecitabine and oxaliplatin). The regimen and duration of neoadjuvant treatment, which included 4 cycles of preoperative and 2 cycles of postoperative chemotherapy, were based on the MDT meeting discussion and our departmental protocol for the treatment of adenocarcinoma of the rectum. After receiving neoadjuvant treatment, the was evaluated with CECT of the chest and abdomen and magnetic resonance imaging (MRI) of the pelvis. On MRI of the pelvis, there was an asymmetric circumferential mural thickening (between the 6- and 7-o’clock positions), extending from 2 cm of the anal verge to the mid-rectum (Fig. 2). No adjacent organs were involved. The patient underwent abdominoperineal excision (APE) with wide local excision of the fistulous tract and primary closure of the wound. On gross examination of the specimen, the fistulous tract was laden with tumor tissue and mucus (Fig. 3). The rectal mucosa was normal. The patient’s postoperative course was uneventful. Histopathology of the resected specimens revealed R0 resection with mucinous adenocarcinoma (ypT3N1c). The patient had an uneventful postoperative course and received adjuvant chemotherapy (capecitabine and oxaliplatin). There was no clinical evidence of recurrence as of the last follow-up (18 months).
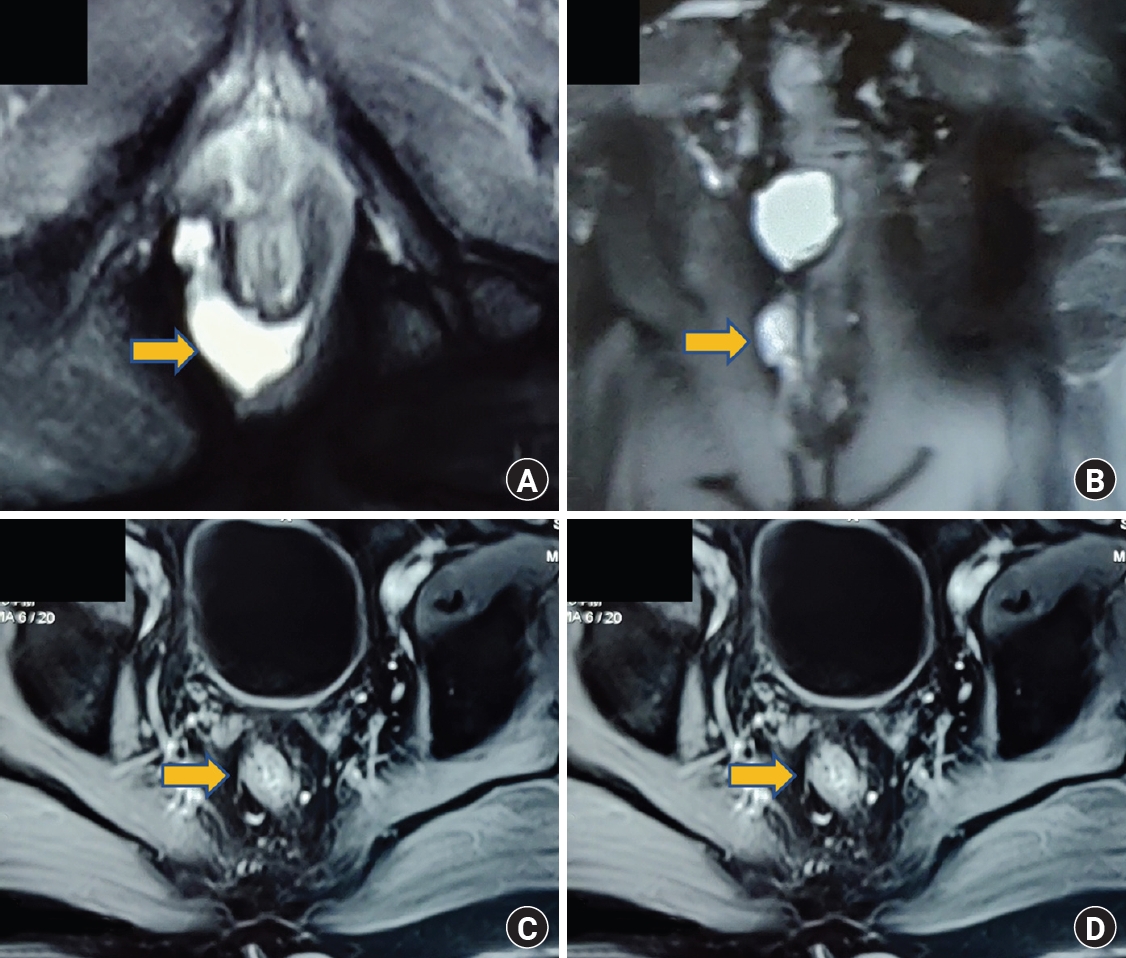
Magnetic resonance imaging (MRI) of the pelvis. (A) A mucinous tumor with normal overlying mucosa (arrow). (B) A mucinous tumor in the fistulous tract (arrow). (C, D) T2-weighted MRI showing the absence of mesorectal infiltration or nodes (arrows).
Written informed consent for the publication of the research details and clinical images was obtained from the patient.
DISCUSSION
FIA is a disturbing disease entity for patients because of its tendency to recur after treatment and associated poor quality of life. These fistulas usually result from cryptoglandular abscesses. These are classified into anal duct, ectopic perianal, and fistula-associated malignancies. FIA is classified in relation to the sphincter complex. The anal canal acts as a transition zone between the rectum and perianal skin; thus, both squamous cell carcinoma and adenocarcinoma can be found. Malignant transformation of FIA is rare, and its mechanism is still unknown.
Whether FIA developed first or malignancy led to fistulization is a challenging question for clinicians. To standardize the diagnosis of malignant transformation of FIA, Rosser [2] reported criteria that include 3 essential components: (1) the fistula should precede the carcinoma by at least 10 years; (2) the only tumor present in the rectum or anal canal should be secondary to direct extension from the carcinoma in the fistula; and (3) the internal opening of the fistula should be into the anal canal and not into the tumor itself.
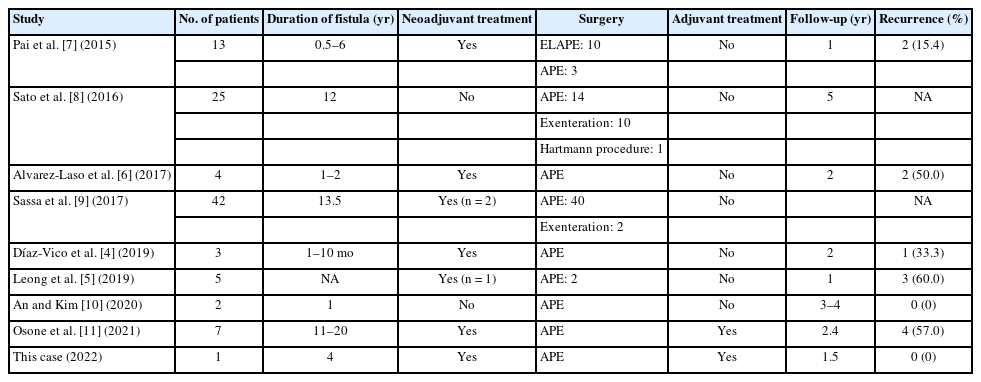
Clinical features may include protracted and worsening symptoms of FIA, persistent pain, a characteristic mucoid discharge instead of stool or pus, a perianal mass, and lymphadenopathy [5]. Our patient developed anorexia and weight loss, which suggested malignancy. Therefore, each patient presenting with prolonged FIA should be asked about these symptoms. An examination and evaluation should rule out any mass in the rectum or colon. In our patient, the fistula had been present for 4 years and there was no tumor present in the rectal mucosa. The authors of other studies in the literature have reported a varied time period between the onset of a fistula and its presentation as a malignant lesion (Table 1) [4–11].
The diagnosis is made through a histopathological examination of tissue obtained during fistula surgery or an examination under anesthesia and biopsy. Pai et al. [7] reported the detection of malignancy in surgical specimens of fistulas in 20% of patients in their series. MRI plays a crucial role in the diagnosis and management planning. Mucinous adenocarcinomas show T1 hypointensity and T2 hyperintensity [12]. In nonmalignant FIA, mucin is encapsulated and localized. However, mucinous malignancy presents with infiltration, a mass, and lymphadenopathy [12].Thus, these findings help in the diagnosis and characterization of the tumor. Serum CEA levels are the most commonly used tumor marker, but elevated serum CEA levels are only observed in 73% of patients [7]. In a nutshell, physicians should have a strong clinical suspicion of malignancy in cases of chronic nonhealing FIA, and biopsy of the lesion is important for the diagnosis. However, there are instances where malignant cells from a distant colorectal malignancy implant into a fistula, and it is therefore important to rule out any synchronous malignancy on colonoscopy [3]. In our patient, colonoscopy revealed normal rectal and colonic mucosa, and a bulge was noted in rectum. Shigoka et al. [13] reported that after fistulectomy, a patient with an adenocarcinoma related to FIA developed a recurrent lesion requiring APE. That report suggests that conservative surgery plays no role in the management of this condition; however, with the advent of neoadjuvant treatment, the role of local excision is uncertain. The basic principle of surgery is to achieve R0 resection, which is challenging, since the margin of resection is obscured by inflammation and edema. Surgical management includes abdominoperineal excision, extralevator APE, or exenteration. However, studies comparing these surgical techniques are not available. The 2 largest series were published by authors from Japan; those reports documented better survival with surgery only, and the majority of patients in their series underwent APE [8, 9].
The risk of recurrence (local or distant) is relatively high because associated inflammation may make margin assessment difficult. Therefore, studies have reported better outcomes with neoadjuvant treatment followed by surgery [5, 6]. The type of neoadjuvant treatment is not uniform across studies; our patient received concurrent chemoradiotherapy (45 Gy in 25 fractions of radiotherapy, as well as oral capecitabine), followed by chemotherapy (4 cycles of capecitabine and oxaliplatin) and adjuvant chemotherapy.
As with other gastrointestinal malignancies, neoadjuvant treatment (NAT) is expected to play a role in achieving R0 resection and preventing local recurrence, however, this possibility has not been established. Some studies have shown favorable outcomes with NAT [5–7]. Hongo et al. [14] have shown complete pathological response in 85% of cases following NAT, with better outcomes in patients who received NAT, APE, and adjuvant treatment. An older report by Gaertner et al. [15] showed that all patients receiving NAT were alive at follow-up (7 out of 7); however, 4 out of 7 patients who did not receive neoadjuvant treatment died during the study period. Pai et al. [7] reported complete response following NAT in 42% of cases, and all patients were free of recurrence at follow-up. They concluded that better outcomes could be achieved due to NAT and extralevator APE. Malignancy in chronic FIA is locally advanced anatomically, and associated inflammation may mask the resection margin; hence, NAT can help sterilize the resection margins, decrease the extent of resection, and prevent local recurrence. However, no consensus exists regarding chemotherapy or chemoradiotherapy. In our patient, neoadjuvant chemoradiotherapy with 4 cycles of chemotherapy was administered according to the MDT decision, which was based on the outcomes of lower rectal adenocarcinoma.
This case report shows that a high level of clinical suspicion and prompt tissue biopsy can diagnose this clinical entity early. In equivocal clinical cases, pelvic MRI can distinguish an inflammatory FIA from malignancy. Surgery plays a pivotal role, and adequate resection has resulted in good outcomes. No consensus exists regarding neoadjuvant or adjuvant chemotherapy or radiotherapy, which needs to be individualized according to institutional policy.
Anal fistula is a common entity, but its malignant transformation is rare. A high index of suspicion based on clinical features is required to detect malignancy in chronic nonhealing fistulas. The majority of patients need APE or more radical excision for R0 resection. However, NAT is an essential component for improving recurrence-free survival. Further studies are required to standardize the treatment of this rare clinical condition.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: AK; Formal analysis: NKG; Writing–original draft: NKG; Writing–review & editing: AK. All authors read and approved the final manuscript.