Introduction of extraperitoneal tunneling method: a way to secure the drain tube in the pelvic cavity after proctectomy
Article information
Abstract
The effectiveness of closed drainage tube insertion after low anterior resection has been controversial. We believe that drain tube displacement, which occurs up to 35% in real clinical practice, reduces the effectiveness of the drain tube. We report in this video a simple way to secure the drain tube in the pelvic cavity after low anterior resection and introduce a case that used the drain fixation method and treated anastomotic leakage without interventional procedure.
INTRODUCTION
Closed drain insertion has been widely used after colorectal anastomosis followed by proctectomy due to the following advantages: early detection of anastomotic leakage (AL), removal of the infected source from the pelvis, and reduction of pelvic sepsis if an anastomotic disruption occurs [1]. Until now, clinicians have routinely inserted drainage tubes after colorectal anastomosis, but several studies have questioned the benefits of prophylactic drainage tube insertion. One randomized trial revealed that the use of a pelvic drain after proctectomy did not confer any benefits to patients [2]. A recent meta-analysis also revealed that routine use of prophylactic drainage in colorectal anastomosis has no benefits in reducing postoperative complications [3]. Moreover, according to the recent enhanced recovery after surgery protocol, routine drain insertion is not recommended [4].
The benefit of prophylactic drainage tube insertion is influenced by postoperative tube displacement. Drain tube migration from the original placement frequently occurred after lower abdominal surgery (Fig. 1). Indeed, 2 studies reported that the rate of drain tube migration from the original insertion site were 31.5% and 37.5% [1, 5].

X-ray findings on postoperative day 2. Drain tube (arrow) displacement occurs. Anastomosis is indicated (arrowhead).
We believe that the effectiveness of drain tube insertion is undermined by drain displacement due to drain tube migration. Therefore, we attempted to find a way to fix the drain tube for the intended period after proctectomy. In this video article, we introduce a method to fix the drain tube called the extraperitoneal tunneling method.
TECHNIQUE
Extraperitoneal tunneling is performed from the left lower quadrant (LLQ) port site; therefore, conventional laparoscopic port insertion is preferred for this procedure. If this method is used in open surgery, the procedure can be performed similarly to the technique performed under a laparoscope.
Ethics statement
The study was performed following the principles stated in the Declaration of Helsinki and Good Clinical Practice. The Institutional Review Board of Yeungnam University Medical Center approved this study and waived the requirement for informed consent (No. YUMC 2022-12-030).
Method 1: using Drain-TG
The Drain-TG (DTG; JSR Medical) was devised by 1 of the authors (JHK) and is specially designed to insert the drain via the extraperitoneal tunneling method (Fig. 2).

Images of Drain-TG (JSR Medical). (A) Handle and drain tube insertion hole. (B) Full picture. The total length of the device is 30 cm. (C) Distal end and drain tube extraction hole.
After bowel anastomosis, the LLQ port site trocar was removed near the end of the surgical procedure. The DTG was inserted through the LLQ port site, and the preperitoneal space was gently dissected using a DTG tip. The DTG was pushed to the desired position while tunneling the preperitoneal space along the left abdominal and pelvic walls. During this process, gentle dissection is essential to prevent damage to ureters or blood vessels.
After the DTG tip was inserted into the pelvic cavity, a drain tube was inserted through the DTG hole. After insertion of the drain tip into the pelvic cavity, the DTG was removed carefully. During this process, the drain tube tip was held with laparoscopic forceps and fixed such that the drain tube was not removed together with the DTG. The drainage tube should have all evacuation sites located within the pelvic cavity to prevent tractitis along the drain tube. After this process was completed, the tube in the pelvic cavity was placed around the colorectal anastomosis site using laparoscopic forceps. If the tube in the pelvic cavity is still too long, it can be cut using laparoscopic scissors to achieve the desired length.
Method 2: using laparoscopic dissector
This method is mostly similar to the method using DTG described above. However, extraperitoneal tunneling was performed using laparoscopic instruments instead of a DTG. In this method, the drain tube was inserted through another trocar port site because there is no entry site for drain tube insertion at the laparoscopic dissector. Therefore, the drain tube was extracted from the pelvic cavity through extraperitoneal tunneling using a laparoscopic dissector.
Case briefing
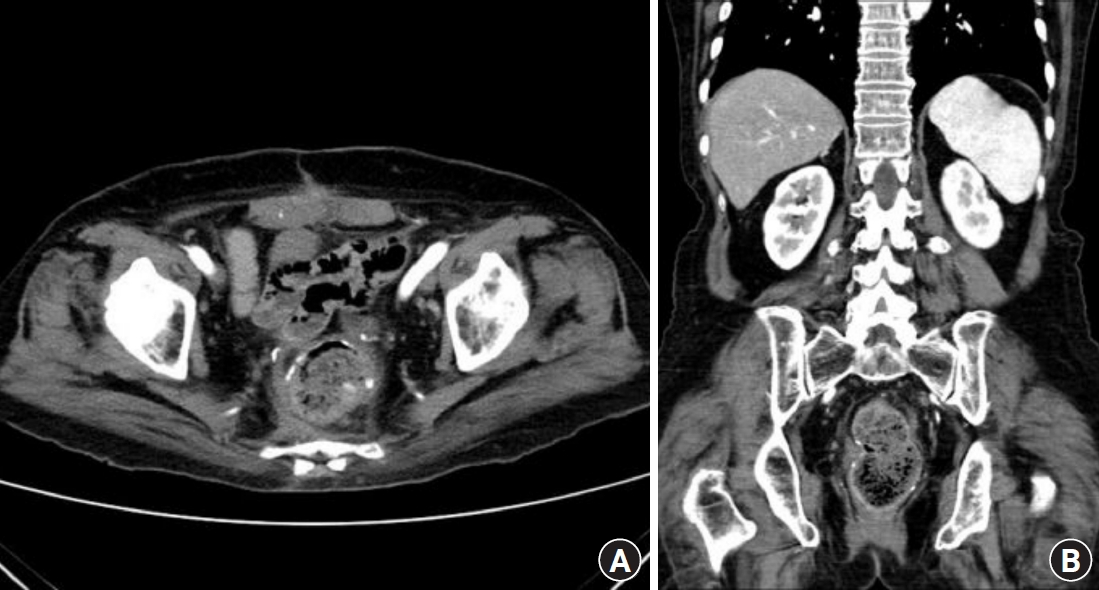
An 82-year-old woman underwent open low anterior resection (LAR) and hysterectomy for a rectouterine fistula. She had a past medical history of diabetes mellitus, hypertension, and open LAR due to rectal cancer 20 years prior. During the last surgery, extraperitoneal drain fixation was performed. During the postoperative course, AL was found on postoperative day 7, and the drainage color changed to a dirty color with a foul odor. However, there were no symptoms related to peritonitis, such as fever or abdominal pain, and no leukocytosis on laboratory examination. She was discharged with a drain tube on postoperative day 14, which was removed on postoperative day 38 at her outpatient clinic follow-up. Radiography performed on postoperative day 38 revealed that the drain tube maintained its original position until it was removed (Fig. 3). Abdominal and pelvic computed tomography 3 months after surgery revealed no AL sequelae on imaging (Fig. 4). In conclusion, although the patient in this case had AL after LAR, AL was resolved with only extraperitoneal tunneling drain tube fixation without any intervention or surgery.
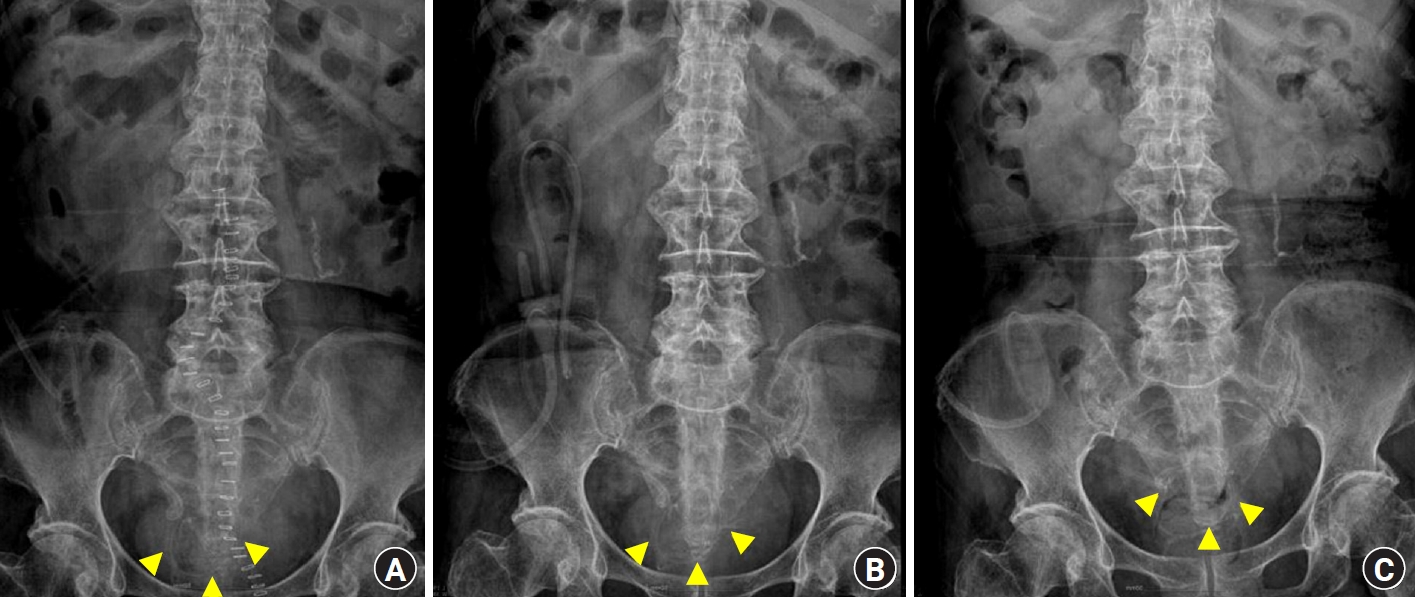
Serial x-ray findings for the drain placement. Drain tube is indicated (arrowheads). (A) Postoperative day 7. (B) Postoperative day 20. (C) Postoperative day 38.
DISCUSSION
Historically, using a drain tube insertion after rectal surgery has been considered to prevent severe complications originating from AL because it can be detected earlier when AL happens and drain the contaminated content via a drain tube. However, recent studies revealed that the drain tube in pelvic cavity has no beneficial effect on overall outcomes after rectal surgery [2, 3, 6]. Based on these results, enhanced recovery after surgery society recommended that pelvic and peritoneal drains should not be used routinely [4].
However, few papers have investigated drainage and displacement, which are directly related to the efficacy of the drainage tube, and this obscures the advantage of the drain tube. In actual clinical practice, displacement of the drainage tube frequently occurs. A recent retrospective study shows that the rate of drain displacement after rectal surgery was 37.5% and drain displacement was associated with increased reintervention rate in patients with AL [1]. Therefore, we think the healing rate without intervention or reoperation when AL occurs can be increased if the drain tube is secured to the original position. The extraperitoneal tunneling method to secure the drain tube after proctectomy is simple and feasible and maximizes the drain tube insertion effect.
There are concerns about complications during this process, such as ureter or vessel injury, hematoma, or tractitis. If a laparoscopy dissector is used for extraperitoneal tunneling, this concern is more pronounced because the tip of the device is rather sharp. However, when DTG is used, the possibility of damage to the ureter or blood vessels that can occur during extraperitoneal tunneling is reduced because the dissection tip of DTG is rounded. Another advantage of using the DTG is that the drain tube can be inserted directly through the DTG. Another advantage of using DTG is that the drain tube can be inserted directly through the DTG. In contrast, when performing extraperitoneal tunneling using a laparoscopic instrument, it is inconvenient to insert the drain tube into the abdominal cavity first and then withdraw it to the tunneling site. Tractitis can be prevented by inserting the evacuation part of the drain tube completely into the pelvic cavity and not remaining inside the tunnel.
In our experience with over 60 cases, there were no complications, such as ureter or vessel injury or tractitis, related to the extraperitoneal tunneling method. However, large-scale studies will be needed for proving this hypothesis about the benefit of the extraperitoneal tunneling method of drain tube fixation.
Notes
Conflict of interest
Jae Hwang Kim is the representative of JSR Medical (Daegu, Korea). No other potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: all authors; Data curation: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript. All authors read and approved the final manuscript.