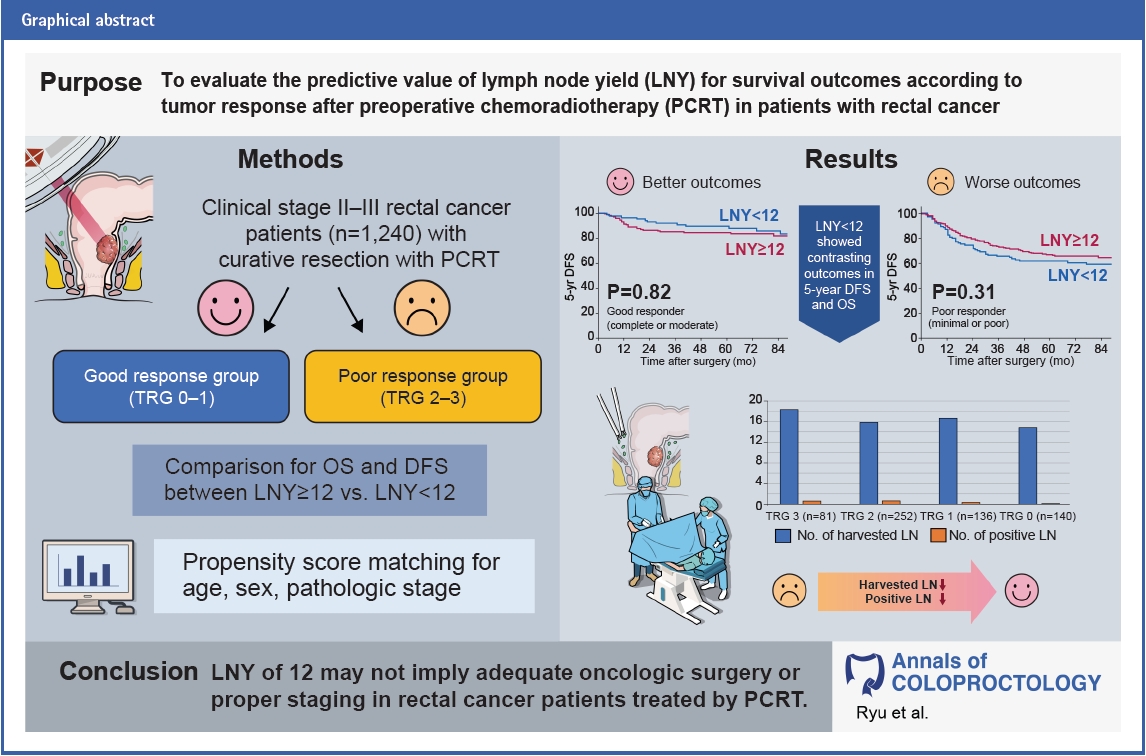
Prognostic significance of lymph node yield on oncologic outcomes according to tumor response after preoperative chemoradiotherapy in rectal cancer patients
Article information
Abstract
Purpose
This study aimed to evaluate the predictive value of lymph node yield (LNY) for survival outcomes according to tumor response after preoperative chemoradiotherapy (PCRT) in patients with rectal cancer.
Methods
This study was a retrospective study conducted in a tertiary center. A total of 1,240 patients with clinical stage II or III rectal cancer who underwent curative resection after PCRT between 2007 and 2016 were included. Patients were categorized into the good response group (tumor regression grade [TRG], 0–1) or poor response group (TRG, 2–3). Propensity score matching was performed for age, sex, and pathologic stage between LNY of ≥12 and LNY of <12 within tumor response group. The primary outcome was 5-year disease-free survival (DFS) and overall survival (OS).
Results
LNY and positive lymph nodes were inversely correlated with TRG. In good responders, 5-year DFS and 5-year OS of patients with LNY of <12 were better than those with LNY of ≥12, but there was no statistical significance. In poor responders, the LNY of <12 group had worse survival outcomes than the LNY of ≥12 group, but there was also no statistical significance. LNY of ≥12 was not associated with DFS and OS in multivariate analysis.
Conclusion
LNY of <12 showed contrasting outcomes between the good and poor responders in 5-year DFS and OS. LNY of 12 may not imply adequate oncologic surgery or proper staging in rectal cancer patients treated by PCRT. Furthermore, a decrease in LNY should be comprehended differently according to tumor response.
INTRODUCTION
Considering that lymph node (LN) status represents a major prognostic factor in colorectal cancer, it is important to obtain a sufficient number of LNs to avoid the underestimation of metastatic LNs [1]. The examination of more LNs allows for more accurate staging and better tailored adjuvant treatments in patients with node-positive disease. Furthermore, the total number of retrieved LNs is associated with survival rates [2, 3]. A more thorough node clearance may itself result in lower rates of recurrence. Other factors associated with LN retrieval, such as the extent and quality of surgical resection, may also affect survival. Therefore, LN retrieval is recognized as a parameter that indicates the quality of oncologic surgery and is suggested as one of the determinants for providing adjuvant treatment in colorectal cancer patients with pathologic T3N0. The current guidelines recommend that at least 12 LNs should be examined to optimize staging [1, 4].
Previous studies have demonstrated that preoperative chemoradiotherapy (PCRT) significantly decreases LN yield (LNY) [5, 6]. However, the implications of lower LNY in patients who underwent PCRT are still unclear. Several studies have suggested that LNY is associated with oncologic outcomes, and efforts should be made to investigate a minimum of 12 LNs [7, 8]. However, some studies have shown that LNY is not significantly associated with survival outcomes even for patients with rectal cancer who received PCRT [9, 10].
A reduction in LNY after PCRT is probably associated with the response to PCRT [11]. Regarding the association between tumor regression and LNY, several studies have shown that a poor tumor regression grade (TRG) is associated with a high LNY [6, 12]. Some studies have suggested that a lower LNY represents a better tumor response, which is associated with a good prognosis [13]. In contrast, some studies have reported that a low LNY is not associated with good tumor response [12]. The relevance in the oncologic outcomes of TRG and LNY is still contradictory.
Therefore, whether a cutoff of at least 12 LNs is appropriate for rectal cancer patients who received PCRT is questionable. In this study, we aimed to evaluate the predictive value of LNY of 12 for survival outcomes according to tumor response after PCRT in patients with rectal cancer.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of Asan Medical Center in Seoul, Korea (No. 2022-0005), with a waiver for informed consent due to the retrospective nature of the study. The study protocol conformed to the tenets of the Declaration of Helsinki.
Enrollment, eligibility, and treatment
Data on all patients with rectal cancer who underwent curativeintent surgery after PCRT between January 2007 and December 2016 were collected in an institutional database. Patients with clinical stage II or III locally advanced rectal cancer after PCRT were considered eligible for inclusion. We excluded patients with hereditary colorectal cancer, inflammatory bowel disease-associated colorectal cancer, synchronous or metachronous cancer, and metastatic rectal cancer and patients who received extended surgery beyond total mesorectal excision. Cancer staging was based on the latest American Joint Committee on Cancer (AJCC) manual at the time of surgery.
Treatment protocols
PCRT included external beam radiation at a total dose of 50.0 to 50.4 Gy in 1.8 to 2.0 Gy fractions, followed by a 4.0 to 5.4 Gy boost in 1.8 to 2.0 Gy fractions and concurrent oral capecitabine or intravenous 5-fluorouracil with leucovorin. Some patients received study-based concurrent chemotherapeutic regimens such as 5-fluorouracil/leucovorin/oxaliplatin, S-1, temozolomide, target agent. Curative-intent surgery was performed according to the principles of total mesorectal excision at 6 to 8 weeks after the completion of PCRT. All operations were performed by 7 experienced colorectal surgeons (50 rectal cancer operations per year for >5 years) by using standardized techniques. Adjuvant chemotherapy was recommended in most cases, except for patients with serious comorbidities, severe side effects expected after chemotherapy, or poor general performance. The regimens and cycles of adjuvant chemotherapy were administered according to the standard protocol, as previously described [14].
Pathologic evaluation
For the complete examination of the harvested LNs, node-bearing pericolic adipose tissue was separated from the specimen. The specimen was carefully palpated for the presence of LNs, and all candidate LNs were dissected for evaluation. The submitted tissue was fixed in 10% buffered formalin for 24 to 48 hours at room temperature before automated tissue processing and embedding to create formalin-fixed, paraffin-embedded tissue blocks. Fivemicron tissue sections were stained with hematoxylin and eosin by using a Leica XL Autostainer (Leica Biosystems) on the basis of the manufacturer’s protocol. The slides were reviewed by pathologists for the number of LNs removed and the presence or absence of metastatic tumors in the LN. If the number of examined LNs is less than 12, additional sections were submitted in an attempt to retrieve additional LNs.
The pathologic response to PCRT was evaluated in the resected specimens by using the AJCC/College of American Pathologists TRG system according to the volume of residual tumor cells as follows: grade 0 (complete response), no remaining viable cancer cells; grade 1 (moderate response), only a small cluster or single cancer cells; grade 2 (minimal response), residual cancer remaining but with predominant fibrosis; and grade 3 (poor response), minimal or no killing of the tumor with extensive residual cancer [15]. On the basis of TRG assessment, we categorized the patients into the good response group (patients with complete or moderate response) or poor response group (patients with minimal or poor response).
Follow-up protocols
All patients were regularly examined every 6 months for the first 5 years after the operation. History taking and physical examination were performed, and laboratory tests including serum carcinoembryonic antigen levels, chest radiography, and abdominopelvic computed tomography (CT) were repeated every 6 months during the follow-up period. Chest CT has been performed annually. Colonoscopy was performed within 1 year after the operation and then once every 2 to 3 years. The primary endpoints were 5-year disease-free survival (DFS) and overall survival (OS) during a median follow-up of 64 months (interquartile range, 55–90 months).
Statistical analysis
The quantitative variables were expressed as means with standard deviations, and categorical variables were presented as numbers and frequencies. We used the chi-square test to compare the distribution of categorical variables, and the t-test was used for continuous variables. The correlation between LNY, positive LNs, and TRG was evaluated using Spearman correlation analysis. Nearest neighbor propensity score matching was performed to reduce the effects of confounding factors between the LNY of ≥12 and LNY of <12 groups, including age, sex, and pathologic stage within the tumor response group. A propensity score was calculated from the logistic equation for each predicted probability, and propensity score matching was performed using the oneto-two method without replacement by using the closest propensity scores. Only patients matched with propensity scores were included in the time-to-event analyses. DFS and OS were calculated using the Kaplan-Meier method and were compared using the log-rank test, and the results were further validated using a Cox proportional hazards regression model. Confounding factors were selected in a forward selection procedure with a limit of 5% change in effect size by using a basic logistic regression model. Statistical significance was established with a 2-sided test at P<0.05. All statistical analyses were performed using IBM SPSS ver. 25.0 (IBM Corp) and R ver. 4.1.2 (R Project for Statistical Computing).
RESULTS
Clinicopathologic characteristics
A total of 1,240 patients with locally advanced rectal cancer who underwent PCRT, followed by curative resection, were included in our study. Table 1 presents the patients and tumor characteristics of the patients and the comparison of the LNY of ≥12 and <12 groups. Among the patients, 1,037 patients (83.6%) had ≥12 harvested LNs, 469 patients (37.8%) had a good response (TRG, 0–1), and 189 patients (15.2%) had a pathological complete response. The mean number of harvested LNs was 17.8. Compared with the LNY of ≥12 group, the LNY of <12 group was significantly older (60.0 years vs. 59.6 years, P<0.001) and had a lower clinical stage and pathologic stage (all P<0.001). The proportion of pathologic complete response was also higher in the LNY of <12 group as compared to the LNY of ≥12 group (22.7% vs. 13.8%, P=0.008).
The mean number of harvested LNs and positive LNs according to TRG was analyzed (Table 2). There was a significant difference in the mean number of harvested LNs (P=0.001) and positive LNs (P<0.001) between each TRG group. The LNY (r=0.106, P<0.001) and positive LNs (r=0.247, P<0.001) were inversely correlated with TRG by correlation analysis.
Tables 3 and 4 show a summary of the patient characteristics according to LNY after propensity score matching. In the good response group, the 86 propensity score–matched patients in the LNY of <12 group were compared with the 172 patients who had LNY of ≥12. The LNY of <12 group had a higher proportion of clinical N0 stage (23.3% vs. 10.5%, P=0.003) and were more likely to receive adjuvant chemotherapy (98.8% vs. 94.8%, P=0.049) than the LNY of ≥12 group (Table 3). In the poor response group, the 117 propensity score–matched patients in the LNY of <12 group were compared with 234 patients in the LNY of ≥12 group. The LNY <12 group had a lower proportion of clinical T4 stage than the LNY of ≥12 group (1.7% vs. 9.0%, P=0.001) and had a different distribution of clinical N stage (P=0.037) than the LNY of ≥12 group (Table 4). There were no other significant differences in clinicopathological characteristics such as tumor location, histologic type, lymphovascular invasion, perineural invasion (PNI), and circumferential resection margin involvement between the 2 groups.

Clinicopathologic features of 1:2 propensity score–matched in good response group (tumor regression grade, 0–1)
Association of LNY with oncologic outcomes
The Kaplan-Meier curves for 5-year DFS (P=0.42) and 5-year OS (P=0.44) comparing LNY of ≥12 and <12 also did not show significant differences (Fig. 1).
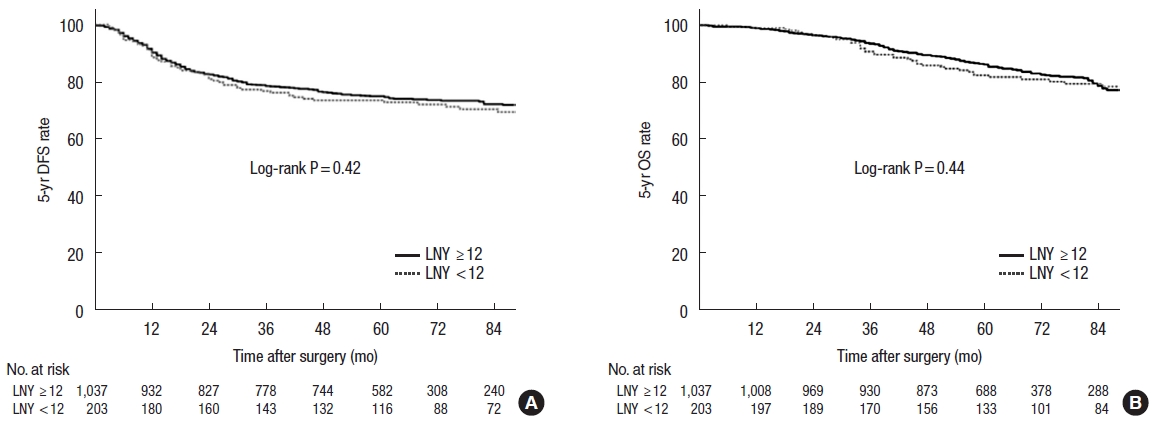
Cumulative 5-year (A) disease-free survival (DFS) and (B) overall survival (OS) rates in the whole study population. LNY, lymph node yield.
We further analyzed the DFS and OS according to LNY in the good and poor response groups. In the good response group, patients in the LNY of <12 group had a higher 5-year DFS and 5-year OS than those in the LNY of ≥12 group but did not produce a statistical significance (P=0.82 and P=0.97, respectively) (Fig. 2A, B). By contrast, in the poor response group, the LNY <12 group had a poorer 5-year DFS (P=0.31) and 5-year OS (P=0.43) than the LNY of ≥12 group (Fig. 2C, D).
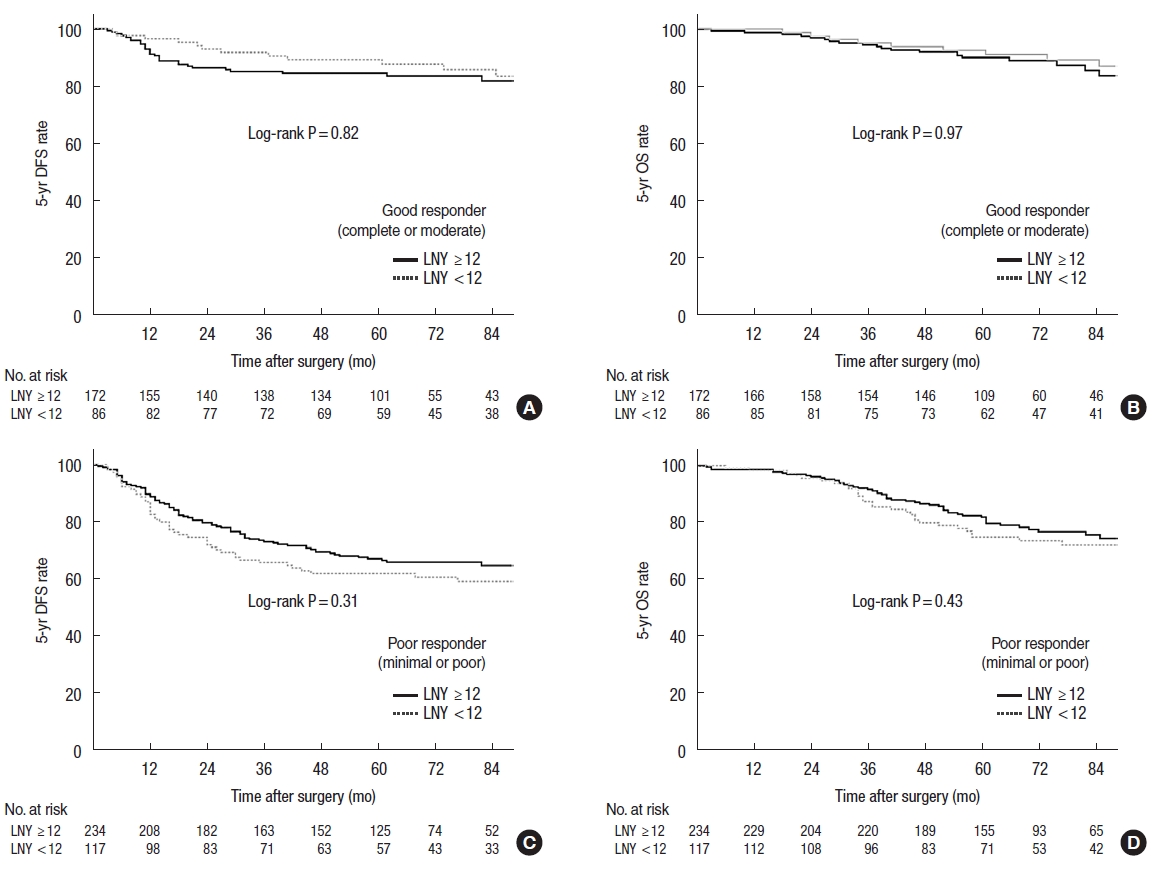
Cumulative 5-year disease-free survival (DFS) and overall survival (OS) rates according to tumor regression grade (TRG) after propensity score matching. (A) DFS and (B) OS in patients with good response (TRG, 0–1). (C) DFS and (D) OS in patients with a poor response (TRG, 2–3). LNY, lymph node yield.
Multivariate analysis was performed separately according to the tumor response group. LNY was not found to have a significant association with DFS and OS in both the good response group and poor response group (Tables 5, 6). In the good response group, undifferentiated histologic type, PNI, advanced ypT stage, and ypN positive disease were revealed as risk factors for DFS. Histologic type, PNI, and ypN+ were significant risk factors for OS (Table 5). Similarly, in the poor response group, histologic type, PNI, ypT stage, and ypN stage were associated factors for poor DFS and OS (Table 6).

Univariate and multivariate analyses of risk factors affecting DFS and OS in good responders among the patients (tumor regression grade, 0–1) (n=469)
DISCUSSION
This study showed that the retrieval of <12 LNs did not lead to significant differences in the subsequent oncologic outcomes for patients with locally advanced rectal cancer who received PCRT. An LNY of <12 showed, however, contrasting outcomes within the good and poor response groups. Among good responders, survival outcomes for those with LNY of <12 were better than those with LNY of ≥12. In contrast, among poor responders, the survival outcomes for those with LNY of <12 were worse than those with LNY of ≥12 but did not reach significance.
The association between PCRT and decreased LNY from a specimen is widely accepted [5, 6, 11, 16]. A large-scale retrospective study [6] showed that PCRT significantly decreases the mean number of LNs retrieved in patients treated with PCRT compared with those not treated with PCRT, and the reduction rate of LNY by PCRT was approximately 33%. A recent meta-analysis [5] also confirmed a mean decrease of LNY of 3.9 in the PCRT group.
PCRT affects LNs via lymphocyte apoptosis within the nodes, in addition to atrophy and fibrosis of the stroma [17, 18]. An increase in the expression of the proapoptotic gene p53 in irradiated lymphocytes, which are highly sensitive to radiation, results in stromal atrophy, fibrosis, and shrinkage, thus leading to the reduction in lymph node size, making them unrecognizable and less likely to contain malignant cells [18, 19]. For these reasons, a lower LNY would be reported in patients with good tumor response after PCRT. In the population of the current study, we showed that there was a significant correlation between LNY and positive LNs with TRG. The results of this study agree with those of prior studies [13]. In addition, some studies reported that good tumor response was an independent predictor for LNY of <12 in multivariate analysis [9, 11, 20]. They concluded that the decrease in LNY after PCRT was affected by tumor response to chemoradiation.
Given that PCRT significantly reduces LNY, the implication of LNY as a prognostic factor in patients who received PCRT should be interpreted with caution. In this study, an LNY of <12 did not have a significant effect on DFS and OS. In line with our results, several studies have shown that an LNY of 12 was not associated with oncologic outcomes in patients who underwent PCRT [9–11, 16, 21–23].
Considering the relationship between tumor response and LNY, a low LNY might be interpreted differently in good responders. Although the difference did not reach statistical significance, we identified favorable DFS and OS in good responders with LNY of <12, which is contrary direction with those in poor responders. de Campos-Lobato et al. [22] reported that LNY of <12 had more pathologic complete responses and that the 5-year local recurrence rate was lower in patients with good response and LNY of <12 than in those with LNY of ≥12. They suggested that the retrieval of <12 LNs may be a marker of higher tumor response and decreased local recurrence rate. Kim et al. [13] also reported a more favorable DFS in good responders with LNY of <12 than in those with LNY of ≥12. Consistent with prior studies, the LNY of <12 group had more pathologic complete response in the population of the current study.
On the contrary, patients with poor response represented higher LNY and have worse survival outcomes when they have <12 harvested LNs. Wang et al. [24] reported that LNY reduction was preferentially observed in cases with good tumor response, and poor responding tumors were found to bear the same number of LNs as tumors that had not been subjected to PCRT. They concluded that the ideal number of LNY may differ according to tumor response. However, for poor responders, 12 LNs may be justified.
Although our results did not show a significant difference in oncologic outcomes according to LNY in both good and poor responders, they showed opposing trends in DFS and OS. Therefore, it is necessary to consider the possibility that the oncologic effect of LNY may differ depending on the tumor response.
Our study has some limitations. First, this was a retrospective, single-center study; therefore, it may have an inherent selection bias even though we attempted to control for known confounders via adjusted analysis. Second, there is a possibility that the skill of the technician may have affected the number of LNs submitted for the examination despite the use of the standardized procedure in the process of making the slide. If LNY was <12, a more skilled technician performed an additional inspection to avoid missing LNs due to the inexperience of the technician. In addition, we did not consider all factors that could affect LNY. In our analysis, age, sex, and pathological stage were adjusted. Multiple factors, such as tumor location, type of surgery, and body mass index, are also likely to affect LNY [6, 25]. Also, details of adjuvant chemotherapy which might have affected the oncologic result have not been investigated. Finally, we did not show the optimal cutoff of LNY representing the difference in survival rates in patients treated with PCRT; however, it is not the purpose of the present study and will be studied in the future. Despite these limitations, our study could clarify the implications of LNY in rectal cancer patients after PCRT. The fewer LNs retrieved after PCRT does not imply an inadequate oncologic resection and may indicate a tumor response. Thus, we consider that the current recommendation of ≥12 LNs does not seem to be reasonable for patients with rectal cancer patients who underwent PCRT.
In conclusion, LNY of <12 showed contrasting outcomes between good and poor responders. LNY of 12 may not imply adequate oncologic surgery or proper staging in patients with rectal cancer treated by PCRT. Furthermore, decreased LNY should be comprehended differently according to tumor response.
Notes
Conflict of interest
In Ja Park is the Editor-in-Chief of Annals of Coloproctology, but was not involved in the review process of this article. No other potential conflict of interest relevant to this article was reported.
Funding
None.
Author contributions
Conceptualization: HSR, IJP; Data curation: all authors; Formal analysis: HSR, IJP; Investigation: all authors; Methodology: HSR, BKA; Project administration: IJP, SBL, JCK; Resources: YIK; Software: MSK, MYP; Supervision: IJP, SBL, JCK; Validation: IJK; Visualization: HSR, YIK; Writing–original draft: HSR; Writing–review & editing: all authors. All authors read and approved the final manuscript.