Laser hemorrhoidoplasty in the treatment of symptomatic hemorrhoids: a pilot Australian study
Article information
Abstract
Purpose
Traditional therapeutic approaches to the surgical management of hemorrhoid disease such as hemorrhoidectomies are plagued with severe postoperative pain and protracted recovery. Our pilot study aims to the laser hemorrhoidoplasty (LH) patients with symptomatic hemorrhoid disease that have failed conservative management for the first time in an Australian population.
Methods
Thirty patients were prospectively enrolled to undergo LH. Postoperative pain, time to return to function, and quality of life (QoL) were determined through the Hemorrhoid Disease Symptom Score and Short Health Scale adapted for hemorrhoidal disease and compared to a historical group of 43 patients who underwent a Milligan-Morgan hemorrhoidectomy by the same surgeon at 3, 6, and 12 months.
Results
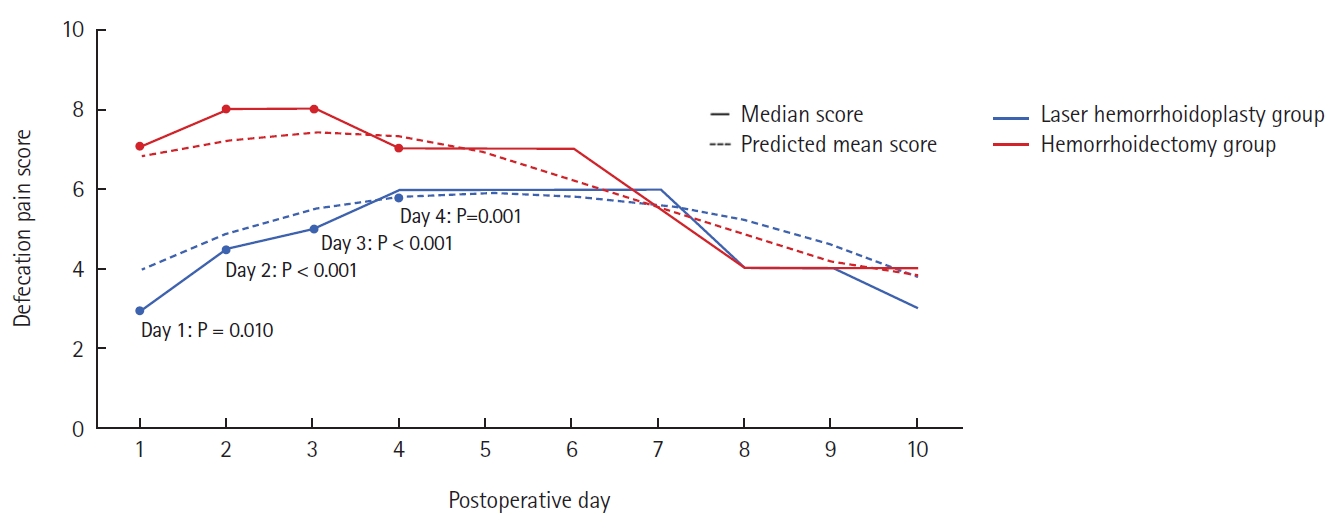
The LH group had significantly lower mean predicted pain scores on days 1 and 2 and lower defecation pain scores and lower opioid analgesia use on days 1, 2, 3, and 4. The median time to return to normal function was significantly lower in the LH group (2 days vs. 9 days, P<0.001). Similarly, the median days to return to the workplace was significantly lower in the LH group (6 days vs. 13 days, P=0.007). During long-term follow-up (12 months), hemorrhoid symptoms and all QoL measures were significantly improved, especially among those with grade II to III disease.
Conclusion
This pilot study demonstrates low pain scores with this revivified procedure in an Australian population, indicating possible expansion of the therapeutic options available for this common condition. Further head-to-head studies comparing LH to other hemorrhoid therapies are required to further determine the most efficacious therapeutic approach.
INTRODUCTION
Hemorrhoid disease is a common entity, with a worldwide prevalence of up to 27.9% [1] and an Australian prevalence of 38.9% [2]. It is estimated that more than 50% of the population will experience symptoms from hemorrhoids within their lifetime [3, 4].
Symptomatic hemorrhoids that have failed conservative medical management can be managed in a variety of ways, depending on their size and symptomatology. The gold standard is a traditional hemorrhoidectomy [5]; however, this is plagued with severe postoperative pain and other complications such as urinary retention, bleeding, anal stenosis, and chronic fissure [6].
Other nonexcisional treatments cause similar issues with pain and are associated with high recurrence rates. Despite the range of surgical treatments and several modifications to their technique, postoperative pain remains the key concern for both patients and clinicians in the management of symptomatic hemorrhoid disease. This often results in reluctance to undergo definitive surgical treatment or extended time off work for those that do [7].
Lasers were first described for use in hemorrhoid disease over 30 years ago [7], but only utilized recently. Although adopted widely in Europe and Asia, its use in Australia has been limited by cost and lack of experience. There are 2 main laser approaches to hemorrhoidal disease. A laser hemorrhoidoplasty (LH) involves an incision at the base of hemorrhoid, via which the hemorrhoidal tissue is coagulated using the laser probe. A hemorrhoidal laser procedure utilizes a Doppler ultrasound probe to identify the terminal branches of the superior rectal artery, which are coagulated with laser energy.
A systematic review in 2021 [8] found that laser treatment universally reported low postoperative pain scores as well as satisfactory symptom relief and recurrence rates on long-term follow-up. Nine out of 19 studies reported significantly lower pain compared with hemorrhoidectomy. Thus far, no Australian studies have been performed.
The authors present a pilot study investigating the Australian experience of LH in patients with symptomatic hemorrhoid disease that have failed conservative management. The primary outcomes are to assess severity and duration of postoperative pain using a 10-day visual analog scale, as well as time to return to normal function and work and compare this to a historical cohort of patients who underwent a traditional Milligan-Morgan hemorrhoidectomy. Secondary outcomes are to objectively assess severity of hemorrhoidal symptoms and their effect on patients’ quality of life (QoL) after 1 year and overall patient satisfaction. We hypothesize that LH involves a speedier and less painful recovery when compared to traditional hemorrhoidectomy and has comparable clinical outcomes in controlling symptoms of hemorrhoidal disease on long-term follow-up.
METHODS
Ethics statement
The study’s protocol was reviewed and approved by the Human Research Ethics Committee of Eastern Health (No. EH 2019-467) and written consent was obtained from each patient for inclusion in the study including the use of deidentified operative photography.
Study design
In this prospective, single-center pilot study, we consecutively recruited 30 patients who presented to Epworth HealthCare (Melbourne, Australia) with symptomatic hemorrhoidal disease between September 2019 and March 2020. Symptomatic hemorrhoids were defined by the presence of hemorrhoidal symptoms (bleeding, itch/discomfort, soiling, and prolapse) and the presence of at least grade II hemorrhoids on clinical examination in whom conservative measures had failed. The cohorts were not stratified by grade of hemorrhoid as it is known that there is no correlation between the grade of hemorrhoid and severity of symptoms [9, 10]. Consecutive patients who presented to the clinic with symptomatic hemorrhoids were clinically assessed and, with informed consent, recruited to the LH group. A historical comparative group, who underwent a traditional Milligan-Morgan hemorrhoidectomy, was enrolled in the trial retrospectively.
We compared the characteristics of LH and hemorrhoidectomy patients using a 2-sided t-test for continuous variables and Fisher exact test for categorical variables. The short-term postoperative outcomes, measured using a 10-day postoperative questionnaire, were as follows: overall daily pain and defecation pain measured daily using a visual analog scale; opioid use measured as any opioid intake in the 24-hour period; and time to return to normal function and normal work (measured in days). They were also asked at day 10 to rate both overall satisfaction and likelihood to undergo the procedure again using a score out of 10. These were recorded in a 10-day patient questionnaire and returned to the surgeon at the routine 2-week postoperative clinical review. For comparison, data collected historically on 43 patients who underwent a hemorrhoidectomy by the same surgeon was used.
Long-term outcomes were assessed using a Hemorrhoidal Disease Symptom Score (HDSS) and Short Health Scale (SHS) adapted for hemorrhoidal disease [11], to objectively document the severity of their hemorrhoidal symptoms (bleeding, itching/discomfort, soiling, and symptom-related QoL). Patients repeated this assessment at 3 and 6 months postoperatively with a further qualitative symptom assessment via telephone interview 1 year after the procedure. Subjectivity in observations by participants was controlled by an identical baseline prehemorrhoidectomy assessment for comparison.
The procedure
The procedure was performed under general anesthesia in lithotomy position. It involved the use of an anal retractor to identify the hemorrhoidal pedicles. To begin with, a 2-0 Vicryl ligature (Ethicon Inc) was used to perform a mucopexy by hitching the hemorrhoidal bundle to the proximal rectal mucosa. A small incision was made at the anoderm adjacent to the hemorrhoidal pedicle to allow the passage of the laser probe (1.8 mm). Using a small artery forceps, a plane between the internal anal sphincter and hemorrhoid tissue was bluntly dissected via this stab incision to form a tract for laser probe to pass into the hemorrhoid tissue (Fig. 1A).

Images of the procedure. (A) Blunt dissection of tract for laser probe. (B) Laser probe. (C) Obliteration of hemorrhoidal tissue using laser energy.
The hemorrhoid tissue was coagulated using a 12-W, 1,470-nm diode laser system by neoLaser via a Biopsy Bell Hemorrhoid 14 G cannula (neoLaser Ltd). The laser probe was advanced into the hemorrhoidal tissue and moved in and out to target the entire bulk of tissue. This laser probe (Fig. 1B) delivers single 3-second pulses in a radial trajectory, emitting energy over a 5- to 6-mm field. The laser beam is considered a divergent beam, where the laser energy dissipates and causes no damage to surrounding normal tissue. We aimed to deliver no more than 250 J per hemorrhoidal node (Fig. 1C). Any bleeding from the site of the tract was controlled with diathermy. A cold wet gauze was compressed against hemorrhoid to reduce swelling. This was repeated for all present hemorrhoid nodes. Any residual large skin tags were excised using diathermy to the level of the anoderm. A bilateral pudendal nerve block was performed, and a cold pack was placed in the anal canal and removed prior to discharge. All patients were discharged home on the day of the procedure.
Patient follow-up
Patients were assessed clinically at day 14 postoperatively and subsequently as required determined by their recovery. In the interim, they were asked to complete a daily pain score and defecation pain score and report any analgesia used. An overall satisfaction score, time to return to baseline function and return to work was also recorded on this questionnaire. The patients were again contacted via phone at 3 and 6 months postoperatively to repeat the SHS to objectively assess the severity of their hemorrhoidal disease postoperatively. At 1 year, all 30 patients were contacted via a short qualitative telephone interview to determine incidence of residual symptoms and whether they were satisfied with the procedure overall.
Statistical analysis
Data were summarized using mean±standard deviation, median (range), and number (%) according to type and distribution. A student T-test was used to compare the characteristics between the two groups. Short-term continuous outcomes (total pain, defecation pain scores, and proportion requiring opioid analgesia) were assessed using a nonlinear B-spline regression model to fit curves plotting the estimated mean for each outcome over the 10-day period. This model incorporates an interaction between outcome and time. Fit was assessed using both locally weighted regression curves and by plotting group medians for each day. The mean predicted difference between groups was tested using unpaired z-score tests for each day with P-values adjusted for the 10 comparisons using the Holm-Sidak correction [12] to account for the increased type I error due to the multiple comparisons performed.
Differences between the groups in medians for overall satisfaction, time to return to normal activities, and time to return to work were tested using the Bonett-Price method [13] and presented as 95% confidence intervals (CIs) and associated P-value. Changes from baseline in the LH group in the SHS 3 and 6 months were assessed using a Wilcoxon signed-rank test. Statistical analysis was performed using the nonparametric series regression suite within Stata ver. 16 (Stata Corp). The significance level was 2-sided and set at 0.05.
RESULTS
In our study, 30 patients underwent LH, of which 1 patient failed to complete their postoperative pain questionnaire. At the 3-month follow-up, 7 patients were lost to follow-up; and at 6 months, 13 patients were lost to follow-up. In our historical comparison group, 43 patients were recruited, and all patients completed their postoperative pain questionnaire. Due to posthemorrhoidectomy outcomes available in existing literature, hemorrhoidectomy patients were not followed up beyond 10 days after the procedure.
The median age in the LH group was 43.5 years (range, 32–88 years) with 23 female patients and 7 male patients. This group had no smokers, with 2 patients on oral anticoagulation (withheld perioperatively). This is compared to the hemorrhoidectomy group, where the median age was 42 years (range, 22–76 years) with 35 female patients and 8 male patients. This group included 2 smokers and did not have any patients on anticoagulation. In the LH group, 5 patients (16.7%) had a history of previous hemorrhoid procedures, which is similar to the hemorrhoidectomy group which had 6 participants (13.9%) with previous hemorrhoid interventions. The median of the grade of hemorrhoids was III in both groups (range, II–IV) and neither group had significant comorbidities. Baseline characteristics are further presented in Table 1.
Laser procedure
The mean procedure time of the laser procedure was 19.8±4.9 minutes (range, 10–32 minutes), average total laser energy used per patient was 611.3±117.8 J (range, 217–988 J). Additionally, 25 patients (83.3%) underwent a mucopexy and 16 (53.3%) had concurrent skin tag removal.
Short-term postoperative functional outcomes and satisfaction
Predicted mean scores, Holm-Sidak adjusted P-values, and raw median scores for daily overall pain and defecatory pain are presented in Table 2 and Figs. 2 and 3. The LH cohort reported the highest pain scores (out of 10) on days 3 and 4 postoperatively, with a median score of 4 on each of these days. The lowest median score was 1 and occurred on day 10 in this cohort of patients. In the hemorrhoidectomy group, the highest pain score was on days 1, 3, and 4 with a score of 5.5 on each of these days. The lowest median pain score of 2 occurred on days 9 and 10.
In terms of pain on defecation (score out of 10), this was highest on days 4 through 7 with a median score of 6 on each of these 4 days in the LH group. Whereas, in the hemorrhoidectomy group, the defecation pain score was highest on days 2 and 3, with a median score of 8 on each of these days. Median pain scores were lowest on day 10 for both groups (3 for the LH group and 4 for the hemorrhoidectomy group).
The LH group had significantly lower mean predicted pain scores on day 1 (P<0.001) and day 2 (P<0.001) and lower defecation pain scores on day 1 (P=0.010), day 2 (P<0.001), day 3 (P<0.001), and day 4 (P=0.001). On the remainder of the days, the differences between the 2 groups were not statistically significant. Furthermore, the differences between the 2 groups became less disparate as time progressed toward day 10 (Table 2).
Furthermore, in the LH group, the mean proportion of patients using opioid analgesia was similar among the 10 days, with a range from 29.2% to 44.0% using opioids, highest on days 7 and 8. Conversely, in the hemorrhoidectomy group, the proportion of patients using opioid analgesia was higher in the earlier postoperative period (days 1–4), with daily percentages of 82.6%, 81%, 57.1%, and 60%, respectively. On day 10, only 26.7% of patients were using opioid analgesia, the lowest percentage within the 10-day period. A significantly smaller proportion of participants used opioid analgesia on days 1 to 4 in the LH group (Table 2, Fig. 4)
The median time to normal function was significantly lower in the LH group (2 days; range, 1–14 days) compared with the hemorrhoidectomy group (9 days; range, 1–21 days; difference in medians, 7; 95% CI, 3–11; P<0.001). Similarly, the median days to return to work was significantly lower in the LH group (6 days; range, 2–21 days) compared with the hemorrhoidectomy group (13 days; range, 4–21 days; difference in medians, 7; 95% CI, 2–12; P=0.007).
Patients in the LH group reported a median overall satisfaction of 8 out of 10 (range, 5–10), which was lower compared with the hemorrhoidectomy group of 10 (range, 5–10; median difference, 2; 95% CI, 1–3; P<0.001).
For patients with grade IV hemorrhoids, the mean satisfaction score at day 10 was 7.4±2.5, which was lower than those undergoing an excisional hemorrhoidectomy (9.3±1.3); however, this was not significant (P=0.056).
There were no perioperative complications. In the LH group, any intraoperative bleeding from the laser tract was easily controlled with diathermy. In the postoperative course, 1 patient presented with small volume bleeding on day 5, managed conservatively. Importantly, patients who were on anticoagulation did not present with delayed bleeding on recommencement of their blood thinners.
One patient presented to hospital with a thrombosed hemorrhoid on day 10, which was managed conservatively with analgesia and ice packs. The incidence of postoperative infection, urinary retention, and return to theatre within 30 days was 0.
Adverse outcomes in the hemorrhoidectomy group were low, with 2 patients (4.7%) going into urinary retention, 2 (4.7%) with fecal impaction, and 1 (2.3%) with postoperative infected abscess requiring drainage.
Long-term outcomes
A summary of the raw median data for both the SHS and hemorrhoidal symptom–related QoL is presented in Table 3. At 3 and 6 months postoperatively, all symptoms and QoL measures indicated improvements for all domains. When the P-values were adjusted for the introduction of type I error by the utilization of multiple comparisons (Holm-Sidak adjustment), all outcomes remained statistically significant. Therefore, at both 3 and 6 months postoperatively, patients report a statistically significant improvement in all hemorrhoidal symptoms and associated QoL measures post-LH.
A shorter qualitative telephone survey at 12 months obtained responses from 16 of 30 LH patients (53.3%) with 13 of the respondents (81.3%) indicating being satisfied overall with the outcomes of the laser procedure. At this time, residual hemorrhoidal symptoms were minimal: pain, 1 (6.3%); bleeding, 4 (25.0%); itch/discomfort, 4 (25.0%); soiling, 0; and swelling, 5 (31.3%).
For those with grade II to III hemorrhoids, 12 of 19 participants (63.2%) responded in the LH group at a 12-month follow-up. Of these 12 participants, 10 (83.3%) were satisfied with the procedure and 9 (75.0%) had no residual symptoms. For those who had grade IV hemorrhoids, 4 of 11 participants (36.4%) responded in the LH group at a 12-month follow-up. Of these 4 participants, 3 (75.0%) were satisfied with the procedure but only 1 (25.0%) had no residual symptoms (P=0.118).
During the 1-year study period, 3 patients (10.0%) underwent a second procedure to excise residual external skin tags. Furthermore, 1 patient went on to have a definitive hemorrhoidectomy 12 months after the initial laser procedure.
DISCUSSION
This pilot study evaluated the outcomes of postoperative pain and return to function and work in patients with symptomatic hemorrhoids undergoing LH in an Australian population. The postoperative pain scores and recovery period were compared with a historical cohort of patients who underwent a hemorrhoidectomy by the same surgeon. This pilot trial demonstrated that LH is feasible with acceptable short- and long-term outcomes, in particular low pain scores and decreased recovery period.
The ideal choice of treatment for hemorrhoidal disease is not straightforward. While hemorrhoid-preserving procedures are purported to reduce pain and improve recovery, there is conflicting evidence regarding their clinical efficacy and long-term outcomes. A traditional hemorrhoidectomy is considered to be the gold standard and allows complete remission of hemorrhoidal disease with recurrence estimated to be 2% to 16% for grade II to IV hemorrhoids at 1 year; however, it is fraught with a painful postoperative journey [14–16]. Therefore, we are always looking for alternatives that result in similar clinical outcomes, but with less postoperative pain.
Literature suggests that LH is more suitable for lower-grade hemorrhoids (grade II and III) with low rates of recurrence [17]. A systematic review by Longchamp et al. [17] highlights that the recurrence rate of hemorrhoids after LH ranges from 0% to 11.3% after 1 year for this cohort, and a 2019 prospective study in Switzerland by Faes et al. [18] on 50 men and women with grade II to III hemorrhoids undergoing LH estimates the 5-year recurrence to be 36% [19]. Our study highlights a similarly low rate of recurrence at 25.0% (3 of 12) for those with grade II and III hemorrhoids at 1 year. However, long-term outcomes of grade IV hemorrhoids have been understudied in literature, as LH is thought to be incomplete with severe hemorrhoid disease based on clinical experience in other countries [20]. A study by Maloku et al. [21] in 2014 highlights that LH is equally efficacious to surgical hemorrhoidectomy at a 1-month follow-up. Our study finds a 75.0% recurrence rate (3 of 4) at 1 year for those undergoing LH with grade IV disease, highlighting that LH may be less effective in severe disease. Therefore, as LH has shown to have minimal intraoperative complications, and low rates of recurrence for those with grade II and III hemorrhoids, this procedure is likely to be safe in moderate hemorrhoidal disease and this pilot study may guide larger clinical trials in Australia [22].
A randomized controlled trial of 121 patients in 2019 [20], comparing LH with suture mucopexy and excisional hemorrhoidectomy found that LH was significantly less painful than excisional hemorrhoidectomy (P<0.001) and associated with earlier return to regular activity (15 days vs. 30 days, P<0.001). Similar to our study, they utilized a 1,470-nm diode laser with similar amounts of energy delivered per hemorrhoid and the results of our study were comparable.
Unexpectedly, the 2-week postoperative satisfaction scores reported were higher in the hemorrhoidectomy cohort compared with the laser cohort. It may be that once the postoperative recovery period is over and the acute pain symptoms have subsided, the hemorrhoidectomy cohort are more satisfied. It is difficult to make further inferences as “satisfaction” is a subjective measure and may be related to factors other than postoperative pain.
Significant complications after LH are uncommon. The occurrence of skin tags is reported in up to 1 of 3 patients after LH [17] and our cohort included 3 patients (10.0%) who required a repeat intervention for excision of residual skin tags. Skin tags may result in patients secondary to the inflammatory response from the heat energy. Such residual tags may be problematic for patients to maintain anal hygiene or for cosmesis and as such, require subsequent excision.
Although the study’s findings are favorable toward the LH cohort, several limitations must be considered. This study may be limited by the sampling error due to the low sample size (n=30). Furthermore, low response rates (n=16) at 1-year follow-up may also cause bias. As this was the first time that LH was trialed in an Australian setting, it was treated as a “pilot study” where the procedure was able to be trialed in a small sample of patients. Given that the study has demonstrated the feasibility of the use of laser energy for hemorrhoids and safety of its use in this Australian cohort, it may serve as a stepping-stone to similar trials with larger patient populations in the future.
Furthermore, our sample of participants undergoing LH has a higher proportion of women than men in both the LH group (76.7% of women) and the comparative Milligan-Morgan hemorrhoidectomy group (81.4% of women). A New Zealand cross-sectional study by Xia et al. [23] in 2020 of over 45,000 participants identifies that the incidence of hemorrhoids in women is 4% less than in men. As these proportions may therefore not be reflective of the general population, our sample may be more reflective of the local demographic of our institution and may have the potential for bias and is a limitation of the small-sampled feasibility study.
Additionally, there may be a component of response bias, whereby the reporting of patients’ pain scores in the LH group may have been more unfavorable as patients may have expected no pain after the anticipated “newer” procedure. There may also be substantial selection bias, due to the loss to follow-up in the postoperative questionnaires. Furthermore, there may be some recall bias, if patients filled in the questionnaire retrospectively before their 2-week review and did not recall their pain scores accurately.
This is the first pilot study to trial laser techniques in the use of symptomatic hemorrhoidal disease in an Australian population and the results have corroborated the international experience, with decreased pain and analgesia use, earlier return to function and the workplace, and clinically efficacy on long-term follow-up. Future studies investigating LH should expand their population size, reproduce the study with randomized patient selection to compare and utilize established symptom scores to be able to objectively assess outcomes.
This pilot study demonstrates low pain scores with this revivified procedure in an Australian population, demonstrating the safety of the use of LH in symptomatic hemorrhoidal disease. LH resulted in significantly lower pain scores, defecation pain scores, and opioid analgesia use in the early postoperative period. Additionally, there was statistically significant symptom resolution and improvement in symptom-related patient QoL on long-term follow-up. Further head-to-head studies comparing LH to other hemorrhoid therapies with larger sample sizes and the utilization of objective postoperative symptoms scores are required to determine the most efficacious therapeutic approach for this common condition.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by a research grant obtained from the Epworth Medical Foundation which facilitated the provision of the laser hemorrhoidoplasty to the patients in the study.
Author contributions
Conceptualization: AJ, NM; Data curation: AJ, CL, GA, NM; Formal analysis: AJ, RH; Funding acquisition: NM; Investigation: AJ; Methodology: AJ, NM; Project administration: GA; Supervision: RH; Validation: CL, RH, NM; Writing–original draft: AJ; Writing–review & editing: all authors. All authors read and approved the final manuscript.