INTRODUCTION
Vascular ectasias are the most common vascular lesions observed in the gastrointestinal tract and probably the most frequent cause of recurrent or chronic lower intestinal bleeding in persons over the age of 60. Colonic vascular ectasias are also known as arteriovenous malformations (AVMs) or angiodysplasia, meaning that the condition involves abnormal dilation of a blood vessel, which is thought to be caused by degenerative changes [1]. These lesions may be solitary or multiple, isolated abnormalities, or part of a systemic disorder [2].
Vascular ectasias have mainly been discovered in the appendix and the ascending colon, and approximately 10% are found in the distal small bowel. Endoscopically, vascular ectasias generally appear as flat or slightly elevated bright red lesions [3]. A pedunculated appearance is extremely rare [3]. We report on a large, pedunculated, polypoid, vascular ectasia, which was successfully removed by using an endoscopic polypectomy with a detachable snare.
CASE REPORT
A 50-year-old man was referred to Ajou University Hospital for a large pedunculated polyp, which was found on colonoscopy during a regular health check-up. The patient had no symptoms and no history of gastrointestinal bleeding, such as melena or hematochezia. In the laboratory findings, hemoglobin was 15.3 g/dL, and hematocrit was 43.7%.
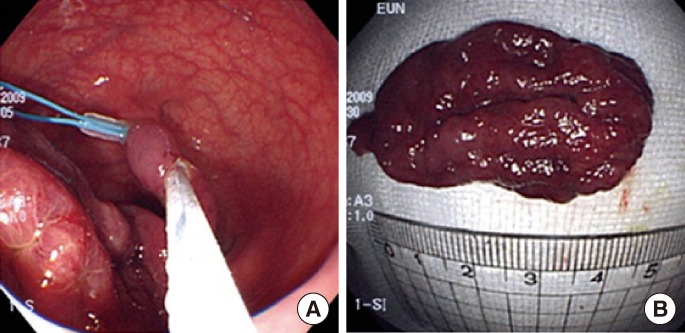
At the time of colonoscopy, a pedunculated polypoid mass measuring approximately 4 cm, with a long stalk, was found in the sigmoid colon (Fig. 1). The head portion of the polyp had a hyperemic mucosal surface with some folds, but no evidence of hemorrhage. To prevent bleeding during polypectomy, we applied a detachable snare to the base of the mass, and we performed a polypectomy successfully without complications (Fig. 2). Pathologic results showed an edematous submucosa with an obvious dilated vein lined with endothelial cells, which was consistent with a vascular ectasia (Fig. 3).
DISCUSSION
Vascular ectasia of the colon was first found during intraoperative angiography by Margulis et al. [4] in 1960 and was diagnosed using colonoscopy by Skibba et al. [5] in 1976. The incidence of vascular ectasia detected by colonoscopy has been reported to range from 1% to 6% [6,7]. Regarding the pathogenesis of vascular ectasia, intermittent low-grade obstruction of submucosal veins was thought to have an important role, involving penetration of muscular layers of the colon, causing small AVMs [1]. This resulted in increased pressure in the venules and capillaries, causing vascular dilatation, tortuosity, and arteriovenous shunts. Histologically, hypertrophy of the submucosal layer, infiltration of inflammatory cells, and irregularly-thickened vessels were found [8].
A pedunculated, polypoid-shaped, colonic vascular ectasia has been reported in 9 cases, including our case. The sizes of the pedunculated vascular ectasias ranged from 0.7 to 6.2 cm, and their main symptom was gastrointestinal bleeding. Hematochezia developed in seven of the 9 cases, iron deficiency anemia in one, and no symptoms in our case. As to shape, seven were pedunculated polyps, and two were semipedunculated polyps. Most of the cases were initially mistaken for a polyp. All things considered, an elevated bright red lesion with a fern-like pattern or ectatic blood vessels radiating from a central vessel must be considered as a vascular ectasia, not a polyp.
As to treatment, six of the 9 cases were treated by using a snare polypectomy or an endoscopic mucosal resection whereas one was treated with a bowel resection, owing to its large size [8], and of the snare polyectomy cases, one required epinephrine and argon plasma coagulation, owing to excessive bleeding [9]. In the remaining 2 cases, including our case, an endoscopic removal with a detachable snare and a polypectomy was done, but having such a patient without symptoms was a first. Therefore, if a polyp is suspected to be hypervascular or to have a high bleeding risk, as in this case, injection of a sclerosing agent or use of a detachable snare prior to a polypectomy may prevent bleeding after the polypectomy [10].
In summary, we reported on a large pedunculated polyp, which was confirmed as an vascular ectasia after a polypectomy, in an asymptomatic patient.