- Search
Most viewed
- Page Path
-
- HOME
- BROWSE ARTICLES
- Most viewed
"Most viewed" articles are updated on a quarterly basis. The following are the most frequently accessed articles from Annals of Coloproctology in the preceding months.
- Anorectal benign disease
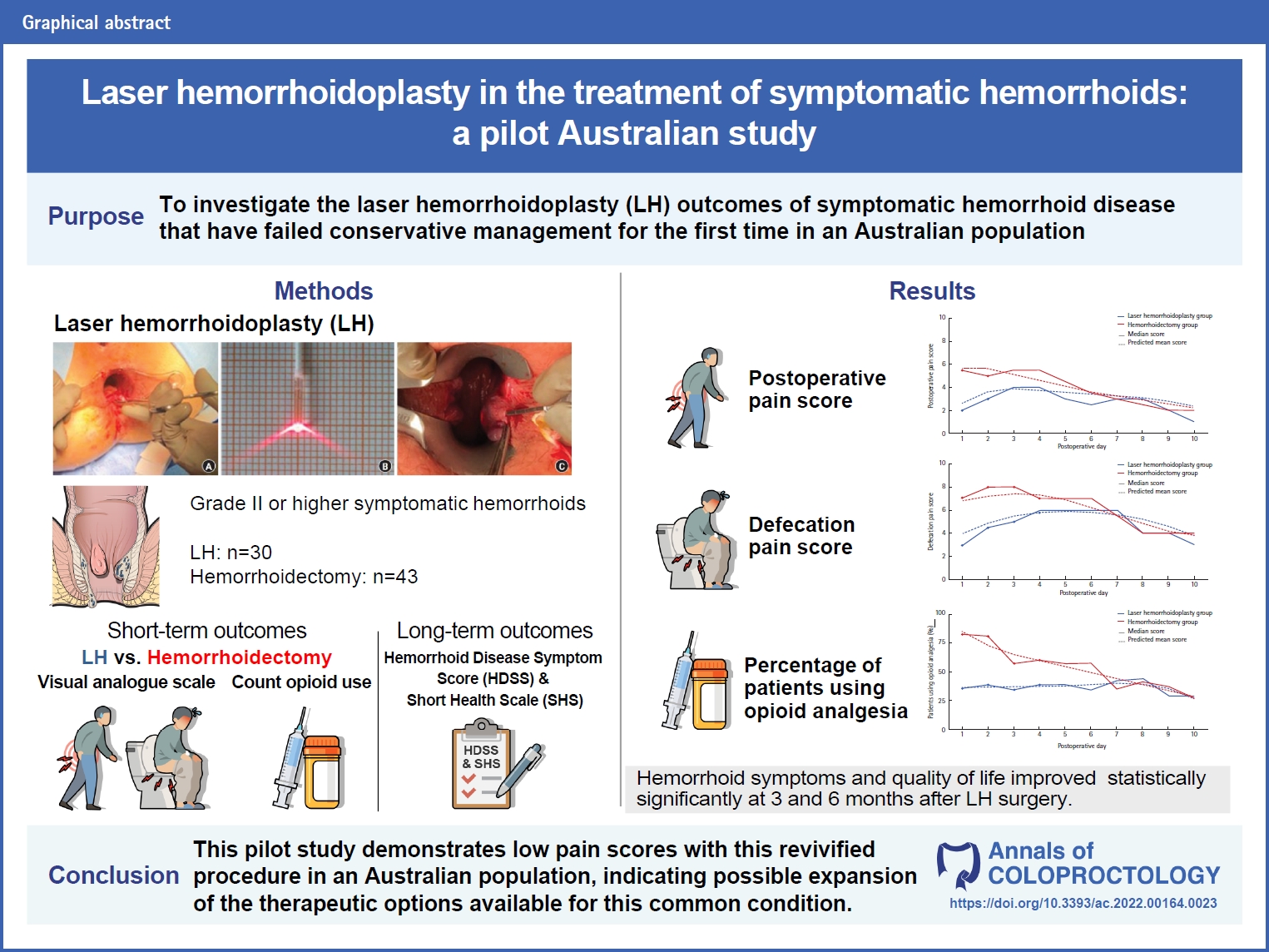
- Laser hemorrhoidoplasty in the treatment of symptomatic hemorrhoids: a pilot Australian study (8,024 times)
- Anshini Jain, Chen Lew, Gamze Aksakal, Richard Hiscock, Naseem Mirbagheri
- Ann Coloproctol. 2024;40(1):52-61. Published online May 19, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- A rare presentation of low-grade appendiceal mucinous neoplasm within an amyand’s hernia: a case report (4,570 times)
- Hani Atiqah Saim, Ian Chik, Fahrol Fahmy Jaafar, Zamri Zuhdi, Razman Jarmin, Azlanudin Azman
- Ann Coloproctol. 2023;39(2):183-187. Published online October 18, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Colorectal cancer
- Long-term clinical outcomes after high and low ligations with lymph node dissection around the root of the inferior mesenteric artery in patients with rectal cancer (1,524 times)
- Min Wan Lee, Sung Sil Park, Kiho You, Dong Eun Lee, Dong Woon Lee, Sung Chan Park, Kyung Su Han, Dae Kyung Sohn, Chang Won Hong, Bun Kim, Byung Chang Kim, Hee Jin Chang, Dae Yong Kim, Jae Hwan Oh
- Ann Coloproctol. 2024;40(1):62-73. Published online February 26, 2024
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Benign bowel disease
- Development of a home health care service platform for ostomy patient management (3,175 times)
- Seongwoo Yang, Ji Won Park, Hyuk Hur, Min Jung Kim, Seung-Yong Jeong, Kyounghoon Park, Ik Yong Kim
- Ann Coloproctol. 2024;40(1):36-43. Published online November 21, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Multimodal prerehabilitation for elderly patients with sarcopenia in colorectal surgery (2,712 times)
- Jingting Wu, Hannah Chi, Shawn Kok, Jason M.W. Chua, Xi-Xiao Huang, Shipin Zhang, Shimin Mah, Li-Xin Foo, Hui-Yee Peh, Hui-Bing Lee, Phoebe Tay, Cherie Tong, Jasmine Ladlad, Cheryl H.M. Tan, Nathanelle Khoo, Darius Aw, Cheryl X.Z. Chong, Leonard M.L. Ho, Sharmini S. Sivarajah, Jialin Ng, Winson J.H. Tan, Fung-Joon Foo, Bin-Tean Teh, Frederick H. Koh
- Ann Coloproctol. 2024;40(1):3-12. Published online March 31, 2023
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Local plus oral antibiotics and strict avoidance of constipation is effective and helps prevents surgery in most cases of anal fissure (5,539 times)
- Pankaj Garg, Vipul D. Yagnik, Kaushik Bhattacharya
- Ann Coloproctol. 2023;39(2):188-189. Published online November 29, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Colorectal cancer
- Performance reporting design in artificial intelligence studies using image-based TNM staging and prognostic parameters in rectal cancer: a systematic review (1,180 times)
- Minsung Kim, Taeyong Park, Bo Young Oh, Min Jeong Kim, Bum-Joo Cho, Il Tae Son
- Ann Coloproctol. 2024;40(1):13-26. Published online February 28, 2024
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Long-term bowel functional outcomes following anal sphincter-preserving surgery for upper and middle rectal cancer: a single-center longitudinal study (946 times)
- Ahmad Sakr, Seung Yoon Yang, Min Soo Cho, Hyuk Hur, Byung Soh Min, Kang Young Lee, Nam Kyu Kim
- Ann Coloproctol. 2024;40(1):27-35. Published online February 28, 2024
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Can the Heald anal stent help to reduce anastomotic or rectal stump leak in elective and emergency colorectal surgery? A single-center experience (1,006 times)
- Michael Jones, Brendan Moran, Richard John Heald, John Bunni
- Ann Coloproctol. 2024;40(1):82-85. Published online February 26, 2024
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Minimally invasive surgery
- Learning curve for single-port robot-assisted colectomy (2,044 times)
- Moon Suk Choi, Seong Hyeon Yun, Sung Chul Lee, Jung Kyong Shin, Yoon Ah Park, Jungwook Huh, Yong Beom Cho, Hee Cheol Kim, Woo Yong Lee
- Ann Coloproctol. 2024;40(1):44-51. Published online December 20, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Robotic natural orifice specimen extraction surgery (NOSES) for anterior resection (2,088 times)
- Toan Duc Pham, Tomas Larach, Bushra Othman, Amrish Rajkomar, Alexander G. Heriot, Satish K. Warrier, Philip Smart
- Ann Coloproctol. 2023;39(6):526-530. Published online December 19, 2023
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF  Supplementary Material
Supplementary Material
- Benign proctology,Rare disease & stoma,Surgical technique
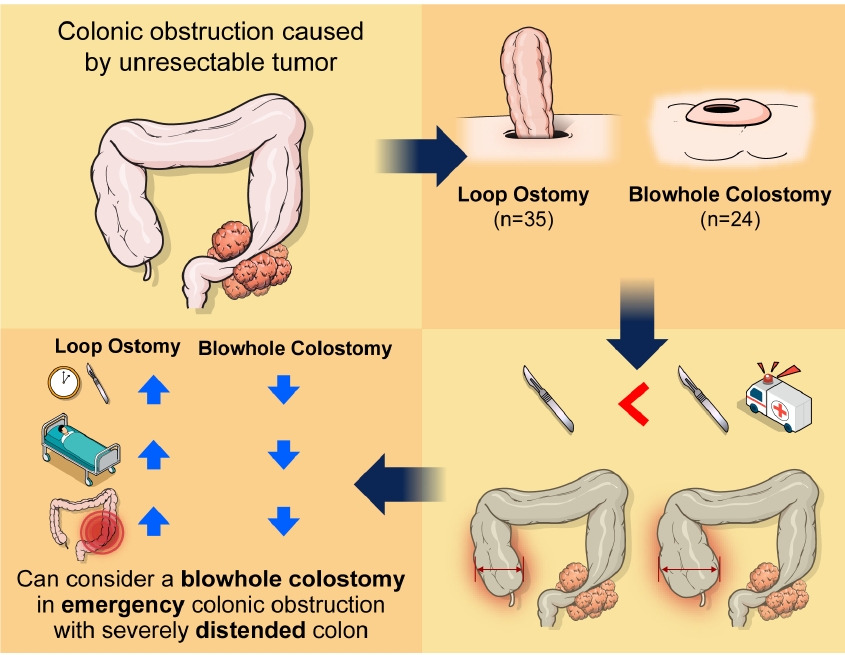
- Comparison of blowhole colostomy and loop ostomy for palliation of acute malignant colonic obstruction (5,715 times)
- Yongjun Park, Dong Uk Choi, Hyung Ook Kim, Yong Bog Kim, Chungki Min, Jung Tack Son, Sung Ryol Lee, Kyung Uk Jung, Hungdai Kim
- Ann Coloproctol. 2022;38(4):319-326. Published online March 7, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Malignant disease, Rectal cancer,Colorectal cancer,Prognosis,Biomarker & risk factor
- Pretreatment inflammatory markers predicting treatment outcomes in colorectal cancer (4,179 times)
- Sanghyun An, Hongjin Shim, Kwangmin Kim, Bora Kim, Hui-Jae Bang, Hyejin Do, Hyang-Rae Lee, Youngwan Kim
- Ann Coloproctol. 2022;38(2):97-108. Published online March 29, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Benign bowel disease
- Short-term outcomes in patients undergoing laparoscopic surgery for deep infiltrative endometriosis with rectal involvement: a single-center experience of 168 cases (2,727 times)
- Sara Gortázar de las Casas, Emanuela Spagnolo, Salomone Di Saverio, Mario Álvarez-Gallego, Ana López Carrasco, María Carbonell López, Sergio Torres Cobos, Constantino Fondevila Campo, Alicia Hernández Gutiérrez, Isabel Pascual Miguelañez
- Ann Coloproctol. 2023;39(3):216-222. Published online March 7, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Influence of colonic mesenteric area on the number of lymph node retrieval for colon cancer: a prospective cohort study (6,575 times)
- Nadir Adnan Hacım, Ahmet Akbaş, Yigit Ulgen, Talar Vartanoglu Aktokmakyan, Serhat Meric, Merve Tokocin, Onder Karabay, Yuksel Altinel
- Ann Coloproctol. 2023;39(1):77-84. Published online September 16, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Anorectal physioloy
- Validation of low anterior resection syndrome score in Brazil with Portuguese (2,669 times)
- Kelly C.L.R. Buzatti, Andy Petroianu, Søren Laurberg, Rodrigo G. Silva, Beatriz D.S. Rodrigues, Peter Christensen, Antonio Lacerda-Filho, Therese Juul
- Ann Coloproctol. 2023;39(5):402-409. Published online May 13, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF