- Search
Most cited
- Page Path
-
- HOME
- BROWSE ARTICLES
- Most cited
“Most cited” articles are based on citations from 2022–2024. The list of the most cited articles can be downloaded by clicking on the “Cited-by list” button.
- Malignant disease, Rectal cancer,Colorectal cancer,Prognosis,Biomarker & risk factor
- Pretreatment inflammatory markers predicting treatment outcomes in colorectal cancer
- Sanghyun An, Hongjin Shim, Kwangmin Kim, Bora Kim, Hui-Jae Bang, Hyejin Do, Hyang-Rae Lee, Youngwan Kim
- Ann Coloproctol. 2022;38(2):97-108. Published online March 29, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
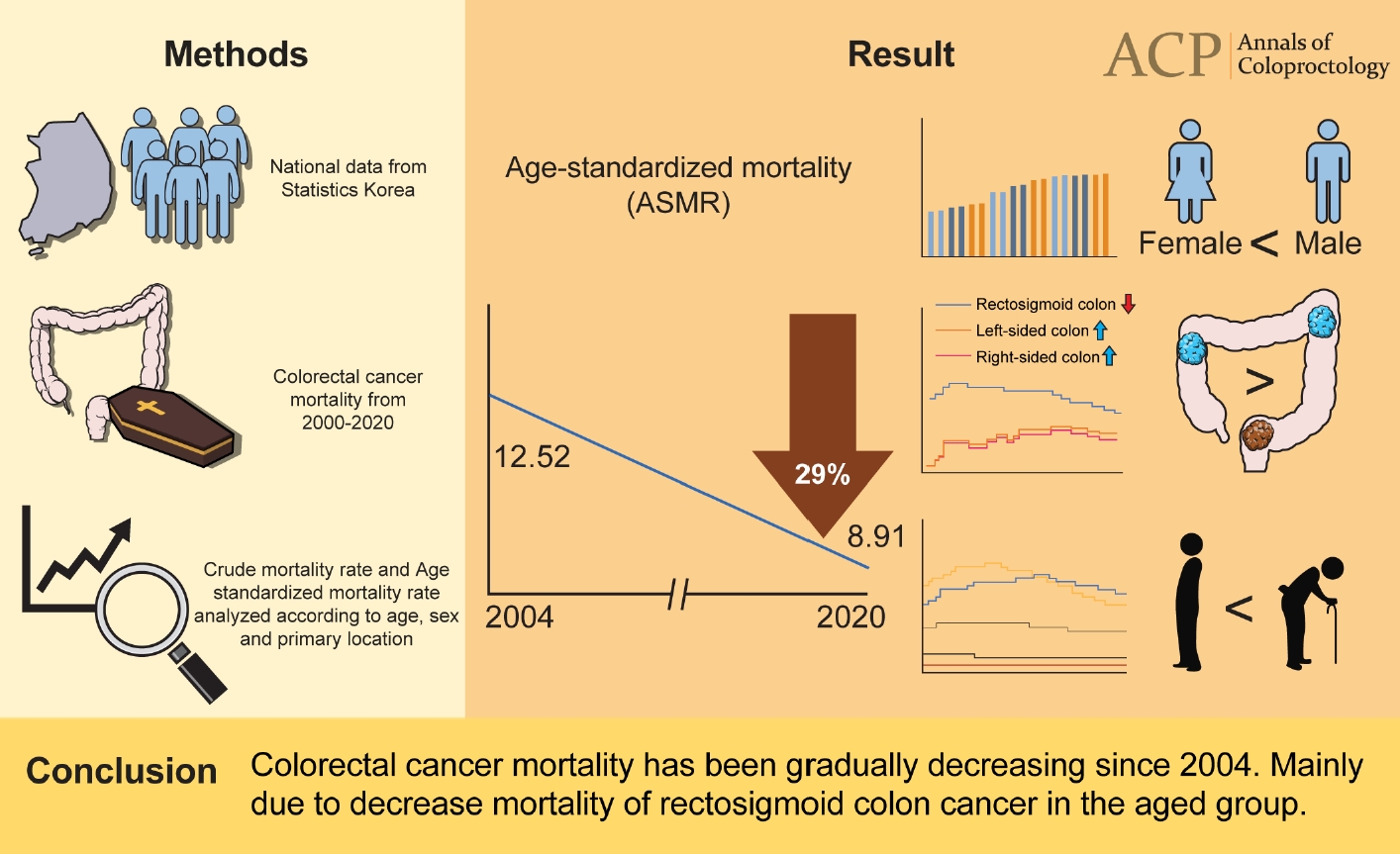
- Malignant disease,Epidemiology & etiology
- Colorectal cancer mortality trends in the era of cancer survivorship in Korea: 2000–2020
- Min Hyun Kim, Sanghee Park, Nari Yi, Bobae Kang, In Ja Park
- Ann Coloproctol. 2022;38(5):343-352. Published online October 28, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF  Supplementary Material
Supplementary Material
- Malignant disease, Rectal cancer,Prognosis,Biomarker & risk factor
- Can pretreatment platelet-to-lymphocyte and neutrophil-to-lymphocyte ratios predict long-term oncologic outcomes after preoperative chemoradiation followed by surgery for locally advanced rectal cancer?
- Sang Hyun An, Ik Yong Kim
- Ann Coloproctol. 2022;38(3):253-261. Published online March 7, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Malignant disease, Rectal cancer,Colorectal cancer,Surgical technique
- The “reverse air leak test”: a new technique for the assessment of low colorectal anastomosis
- Francesco Crafa, Augusto Striano, Francesco Esposito, Amalia Rosaria Rita Rossetti, Mario Baiamonte, Valeria Gianfreda, Antonio Longo
- Ann Coloproctol. 2022;38(1):20-27. Published online December 4, 2020
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Complication,Biomarker & risk factor
- Intraoperative fluorescence angiography as an independent factor of anastomotic leakage and a nomogram for predicting leak for colorectal anastomoses
- Mikhail Alekseev, Evgeny Rybakov, Evgeniy Khomyakov, Irina Zarodnyuk, Yuri Shelygin
- Ann Coloproctol. 2022;38(5):380-386. Published online July 22, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Malignant disease,Prognosis and adjuvant therapy,Functional outcomes,Colorectal cancer,Postoperative outcome & ERAS
- Clinical validation of implementing Enhanced Recovery After Surgery protocol in elderly colorectal cancer patients
- Wooree Koh, Chul Seung Lee, Jung Hoon Bae, Abdullah Al-Sawat, In Kyu Lee, Hyeong Yong Jin
- Ann Coloproctol. 2022;38(1):47-52. Published online July 21, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF  Supplementary Material
Supplementary Material
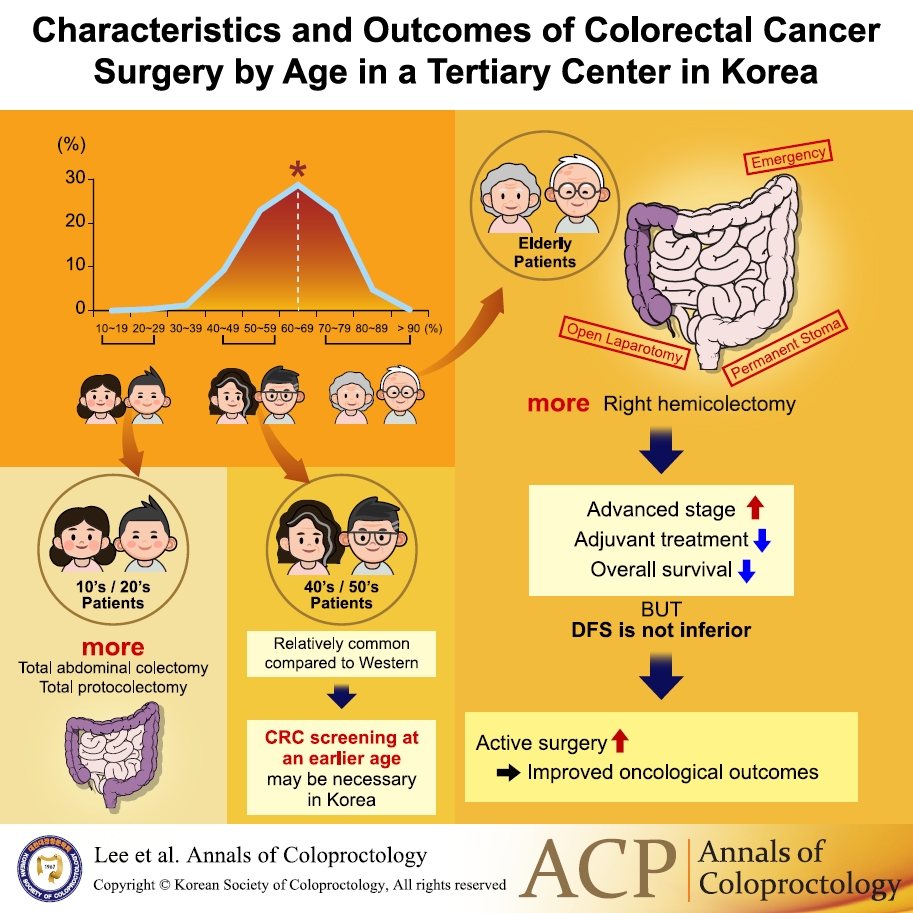
- Malignant disease,Prognosis and adjuvant therapy,Colorectal cancer,Epidemiology & etiology
- Characteristics and outcomes of colorectal cancer surgery by age in a tertiary center in Korea: a retrospective review
- Tae-Hoon Lee, Jeong Min Choo, Jeong Sub Kim, Seon Hui Shin, Ji-Seon Kim, Se-Jin Baek, Jung-Myun Kwak, Jin Kim, Seon-Hahn Kim
- Ann Coloproctol. 2022;38(3):244-252. Published online November 4, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Malignant disease, Rectal cancer,Prognosis
- Initial local excision for clinical T1 rectal cancer showed comparable overall survival despite high local recurrence rate: a propensity-matched analysis
- Jong Hee Hyun, Mohamed K. Alhanafy, Hyoung-Chul Park, Su Min Park, Sung-Chan Park, Dae Kyung Sohn, Duck-Woo Kim, Sung-Bum Kang, Seung-Yong Jeong, Kyu Joo Park, Jae Hwan Oh, on behalf of the Seoul Colorectal Research Group (SECOG)
- Ann Coloproctol. 2022;38(2):166-175. Published online October 6, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Malignant disease,Prognosis and adjuvant therapy,Functional outcomes,Postoperative outcome & ERAS
- The impact of variations in care and complications within a colorectal Enhanced Recovery After Surgery program on length of stay
- James Wei Tatt Toh, Jack Cecire, Kerry Hitos, Karen Shedden, Fiona Gavegan, Nimalan Pathmanathan, Toufic El Khoury, Angelina Di Re, Annelise Cocco, Alex Limmer, Tom Liang, Kar Yin Fok, James Rogers, Edgardo Solis, Grahame Ctercteko
- Ann Coloproctol. 2022;38(1):36-46. Published online May 6, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF  Supplementary Material
Supplementary Material
- Malignant disease, Rectal cancer,Colorectal cancer,Functional outcome,Surgical technique
- Oncological and functional outcomes of transanal total mesorectal excision in a teaching hospital in the Netherlands
- Joost A.G. van der Heijden, Kelly G.H. van de Pas, Frank J.C. van den Broek, Francois M.H. van Dielen, Gerrit D. Slooter, Adriana J.G. Maaskant-Braat
- Ann Coloproctol. 2022;38(1):28-35. Published online June 29, 2021
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
- Benign bowel disease
- Multimodal prerehabilitation for elderly patients with sarcopenia in colorectal surgery
- Jingting Wu, Hannah Chi, Shawn Kok, Jason M.W. Chua, Xi-Xiao Huang, Shipin Zhang, Shimin Mah, Li-Xin Foo, Hui-Yee Peh, Hui-Bing Lee, Phoebe Tay, Cherie Tong, Jasmine Ladlad, Cheryl H.M. Tan, Nathanelle Khoo, Darius Aw, Cheryl X.Z. Chong, Leonard M.L. Ho, Sharmini S. Sivarajah, Jialin Ng, Winson J.H. Tan, Fung-Joon Foo, Bin-Tean Teh, Frederick H. Koh
- Ann Coloproctol. 2024;40(1):3-12. Published online March 31, 2023
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF
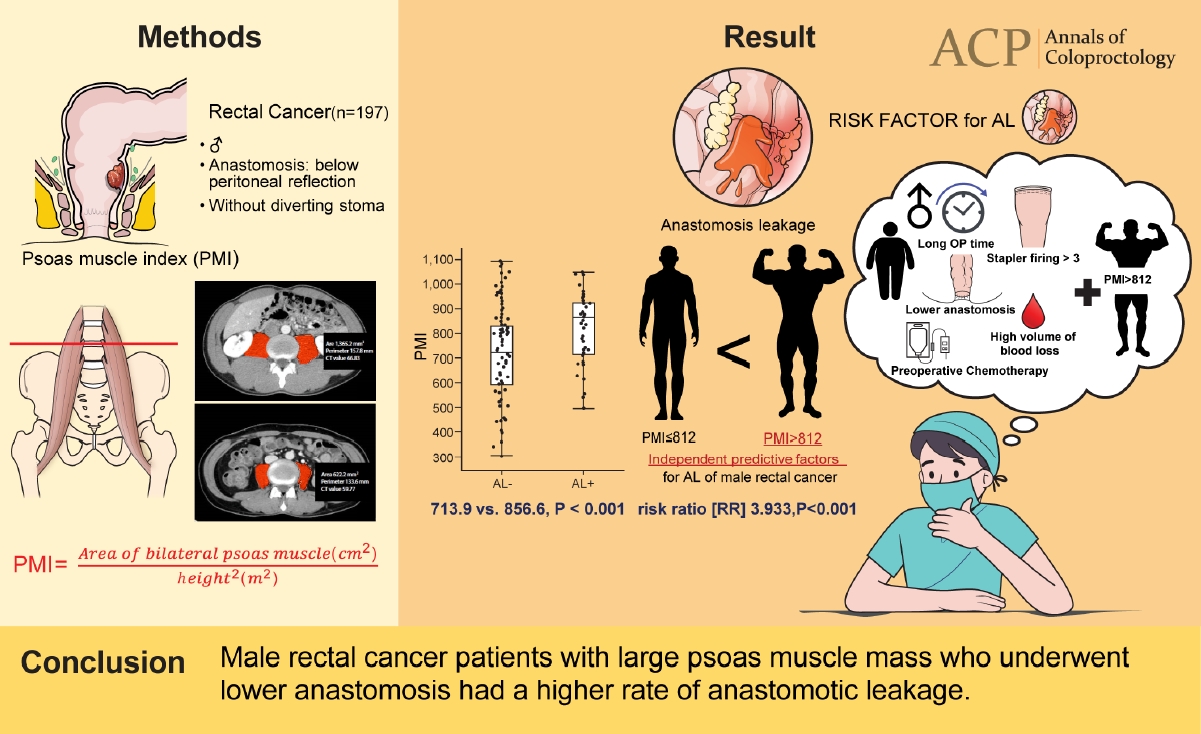
- Malignant disease,Rectal cancer,Complication,Biomarker & risk factor
- Cross-sectional area of psoas muscle as a predictive marker of anastomotic failure in male rectal cancer patients: Japanese single institutional retrospective observational study
- Yusuke Mizuuchi, Yoshitaka Tanabe, Masafumi Sada, Koji Tamura, Kinuko Nagayoshi, Shuntaro Nagai, Yusuke Watanabe, Sadafumi Tamiya, Kohei Nakata, Kenoki Ohuchida, Toru Nakano, Masafumi Nakamura
- Ann Coloproctol. 2022;38(5):353-361. Published online April 12, 2022
-
 Full text
Full text  PubReader
PubReader  ePub
ePub  Citation
Citation  PDF
PDF  Supplementary Material
Supplementary Material