- Search
Abstract
The case of a 23-year-old female treated with aggressive high-dose therapy for Burkitt's lymphoma is reported. A positron emission tomography and computed tomography scan after completion of chemotherapy revealed a residual hypermetabolic lesion in the right pelvic cavity. A pelvic magnetic resonance imaging scan showed circumferential wall thickening at the tip of the appendix. A laparoscopic exploration and appendectomy were performed, and a pathologic examination of the resected appendix revealed xanthogranulomatous appendicitis. This is a rare case of a xanthogranulomatous appendicitis mimicking remnant Burkitt's lymphoma after completion of chemotherapy.
Burkitt's lymphoma was first described in 1958 as a highly-aggressive B-cell non-Hodgkin's lymphoma characterized by monomorphic medium-sized cells. It is the most prevalent type of lymphoma in children [1]. The most commonly involved site in cases of sporadic Burkitt's lymphoma is the abdomen [2]. Because of the abundant lymphoid tissue, the ileocolic region is the most common site affected in children younger than 16 years of age. Burkitt's lymphoma in adults is uncommon and typically presents with symptoms of rapidly developing disease, most commonly in the abdomen. The chemotherapy regimen generally used for adults includes cyclophosphamide, vincristine, doxorubicin, and high-dose methotrexate alternating with ifosfamide, etoposide, and high-dose cytarabine [1]. Magrath et al. [3] reported an 89% 2-year survival rate among 54 adult patients. Because Burkitt's lymphoma produces a very high signal on fluorodeoxyglucose positron emission tomography (PET) scans, PET is a valuable tool for detection of disease recurrence [4].
Xanthogranulomatous appendicitis is a rare phenomenon, with only 10 cases having been reported to date in the English literature [5]. In cases of acute appendicitis, xanthogranulomatous inflammation is more commonly seen with delayed appendectomy [6]. Typically, xanthogranulomatous inflammation is found in the kidneys, gallbladder, lungs, and prostate [7]. Xanthogranulomatous appendicitis can be misdiagnosed as remnant malignancy, which may lead to unnecessary further treatment. We report a rare case of xanthogranulomatous appendicitis mimicking remnant Burkitt's lymphoma on radiologic studies.
In March 2013, a 23-year-old woman was admitted to our hospital for low abdominal pain. PET and computed tomography (CT) scans revealed conglomerated, vessel-encasing hypermetabolic masses extending from the midabdomen into the pelvic cavity. The mass partially encased the terminal ileum without obstruction (Fig. 1). An ultrasound-guided biopsy was performed, and immunohistochemical staining was positive for CD20, CD10, and Bcl-6 and negative for CD3, Bcl-2, CD30, and MUM-1. Ki67 L.I. was nearly 100%. A pathologic diagnosis of malignant Burkitt's lymphoma was made.
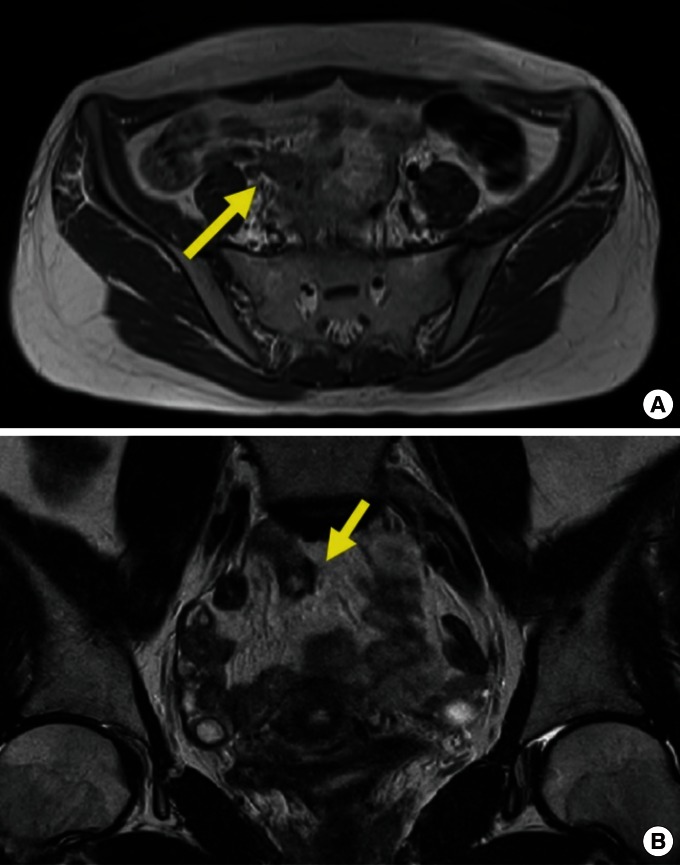
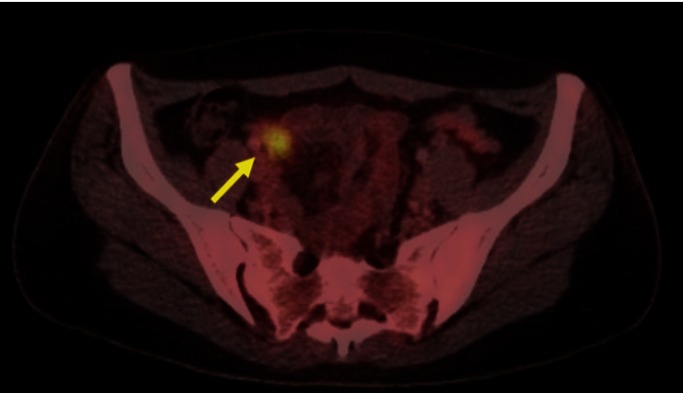
In April 2013, R-hyper cyclophosphamide, vincristine, doxorubicin, dexamethasone (CVAD) chemotherapy was initiated in this patient. Cyclophosphamide, vincristine, doxorubicin, dexamethasone, cytarabine, mesna, and methotrexate were given during the odd cycles. Methotrexate, leucovorin, sodium bicarbonate, and cytarabine were given during the even cycles. A total of 8 cycles of R-hyper CVAD chemotherapy were given until November 2013. After termination of chemotherapy, another PET-CT scan was obtained in December 2013 and showed a residual hypermetabolic lesion in the right pelvic cavity (Fig. 2). Because fluodeoxyglucose (FDG) uptake can be interpreted as physiologic uptake, we opted for reevaluation after 3 weeks. However, there was no change in the hypermetabolic lesion. Pelvic magnetic resonance imaging (MRI) was subsequently performed for further evaluation (Fig. 3) and revealed circumferential wall thickening at the tip of the appendix, suggesting either chronic appendicitis or the formation of a mucocele or regressed lymphoma.
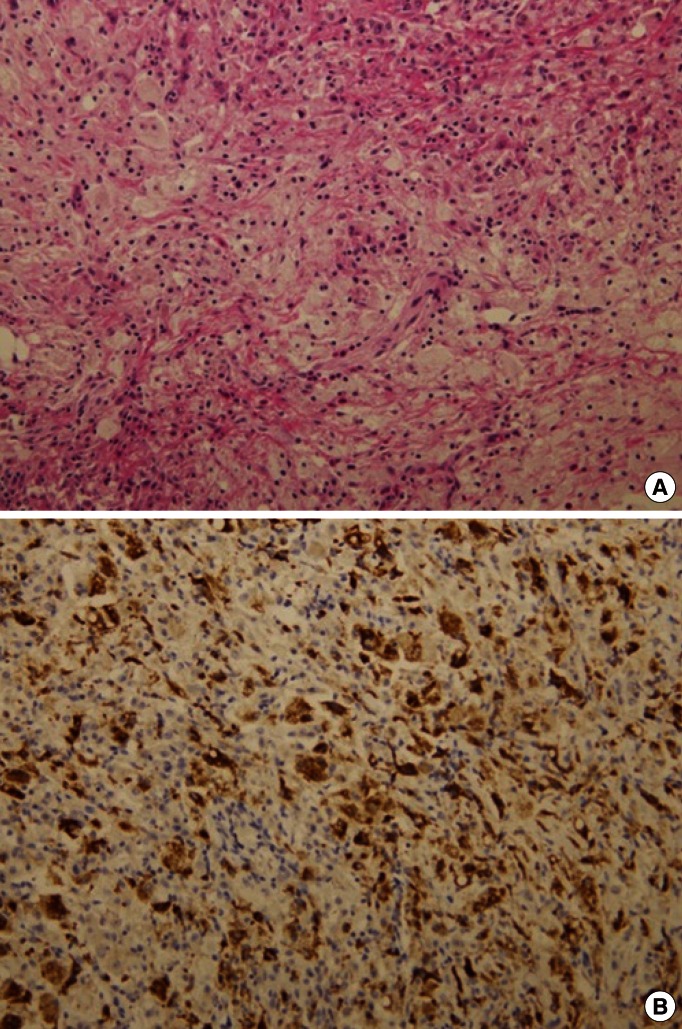
The patient was referred to the Department of Surgery, and a laparoscopic exploration was performed. Some adhesions were found between the mesoappendix and the mesentery of the terminal ileum. Fibrotic scar tissue, suggesting regression of a lymphoma, was also detected in the lower pelvic cavity. An enlargement of the appendiceal tip, which looked consistent with a remnant lymphoma, was onserved. A small mass near the appendix, which was presumed to be a lymph node, was excised along with the appendix. The specimen was sent for histopathologic evaluation, and the patient's postoperative course was uncomplicated. The final pathology of the specimen revealed a xanthogranulomatous appendicitis, with no evidence of a remnant lymphoma. The small mass near the appendix was identified as a foamy histiocytic collection (Fig. 4). No further evaluation or treatment was required, though the patient was scheduled for regular follow-up.
Burkitt's lymphoma typically presents with a bulky abdominal mass, B symptoms, and laboratory evidence of tumor lysis [8]. Prompt diagnosis and initiation of appropriate therapy are necessary for optimal results, as complete regression of a lymphoma is important for long-term survival [9]. Relapses of Burkitt's lymphoma, which most commonly occur within 6 months of completion of treatment, are associated with poor outcomes [1]. In clinical practice, remnant masses have been observed on imaging studies after completion of intensive chemotherapy in several cases [10,11]. Son et al. [11] reported a case of ectopic thymic hyperplasia after chemotherapy for Burkitt's lymphoma. Karmazyn et al. [10] reported 7 patients with residual abdominal masses among 33 children with abdominal Burkitt's lymphoma who were confirmed to be in complete remission after chemotherapy. Complete remission was defined as complete disappearance of all measurable lesions with no blasts in the bone marrow or cerebrospinal fluid. Among those seven patients, 2 underwent a secondlook surgery. The final pathologic diagnosis was fibrosis with no evidence of a viable tumor. The remaining five patients were closely followed, and most of the masses showed spontaneous regression [10]. Among those 7 patients, none relapsed. In this study, the main diagnostic tool was CT and/or ultrasonography, though differentiating viable tumors and fibrosis by using these imaging modalities is sometimes difficult. Nowadays, the PET scan is regarded as a valuable tool for the detection of disease recurrence [4].
In our case, the high FDG uptake on the PET-CT scan after chemotherapy led us to suspect a remnant lymphoma. In addition, a follow-up MRI scan could not discriminate a regressed lymphoma from other benign conditions such as mucoceles or chronic appendicitis. Thus, surgical exploration was inevitable.
Xanthogranulomatous inflammation is a very rare pathologic finding and has been reported to occur in the kidneys, gallbladder, urinary bladder, thyroid, endometrium, adrenal glands, and fallopian tubes [12]. The pathogenesis of xanthogranulomatous inflammation is still unknown. However, xanthogranulomatous change is suspected to be the result of hemorrhage, immunological disorders, bacterial infection, reactions to specific infectious agents, and/or lymphatic obstruction [6,12,13]. Xanthogranulomatous change in the appendix is typically due to a long-standing or recurrent inflammatory process. Guo and Greenson [6] reported that in interval appendectomy specimens, granulomatous inflammation, xanthogranulomatous inflammation, and Crohn's-like changes were more common than they were in acute appendectomy specimens.
When the proximity of the primary mass to the appendix at the time of initial diagnosis is considered, xanthogranuloma appendicitis may be due to a residual change in the appendix after chemotherapy. However, the exact pathogenesis in these cases remains unclear. In addition, the FDG uptake of xanthogranulomatous appendicitis was difficult to distinguish from that of the suspected remnant lesions after chemotherapy for Burkitt's lymphoma. In conclusion, xanthogranulomatous appendicitis is a rare disease that is difficult to diagnose on imaging studies alone.
References
1. Molyneux EM, Rochford R, Griffin B, Newton R, Jackson G, Menon G, et al. Burkitt's lymphoma. Lancet 2012;379:1234ŌĆō1244. PMID: 22333947.


2. Mbulaiteye SM, Biggar RJ, Bhatia K, Linet MS, Devesa SS. Sporadic childhood Burkitt lymphoma incidence in the United States during 1992-2005. Pediatr Blood Cancer 2009;53:366ŌĆō370. PMID: 19434731.



3. Magrath I, Adde M, Shad A, Venzon D, Seibel N, Gootenberg J, et al. Adults and children with small non-cleaved-cell lymphoma have a similar excellent outcome when treated with the same chemotherapy regimen. J Clin Oncol 1996;14:925ŌĆō934. PMID: 8622041.


4. Zeng W, Lechowicz MJ, Winton E, Cho SM, Galt JR, Halkar R. Spectrum of FDG PET/CT findings in Burkitt lymphoma. Clin Nucl Med 2009;34:355ŌĆō358. PMID: 19487844.


5. Al-Rawabdeh SM, Prasad V, King DR, Kahwash SB. Xanthogranulomatous appendicitis in a child: report of a case and review of the literature. Case Rep Med 2013;2013:498191PMID: 24093025.



6. Guo G, Greenson JK. Histopathology of interval (delayed) appendectomy specimens: strong association with granulomatous and xanthogranulomatous appendicitis. Am J Surg Pathol 2003;27:1147ŌĆō1151. PMID: 12883248.


7. Mado K, Mazaki T, Henmi A, Masuda H, Takayama T. Xanthogranulomatous appendicitis. Indian J Surg 2013;75:405ŌĆō406. PMID: 24426487.


8. Perkins AS, Friedberg JW. Burkitt lymphoma in adults. Hematology Am Soc Hematol Educ Program 2008;341ŌĆō348. PMID: 19074108.


9. Aldoss IT, Weisenburger DD, Fu K, Chan WC, Vose JM, Bierman PJ, et al. Adult Burkitt lymphoma: advances in diagnosis and treatment. Oncology (Williston Park) 2008;22:1508ŌĆō1517. PMID: 19133605.

10. Karmazyn B, Ash S, Goshen Y, Yaniv I, Horev G, Kornreich L. Significance of residual abdominal masses in children with abdominal Burkitt's lymphoma. Pediatr Radiol 2001;31:801ŌĆō805. PMID: 11692238.


11. Son SK, Park SS, Kim YD, Choi KU, Lim YT. Ectopic thymic hyperplasia in a patient treated for Burkitt lymphoma. J Pediatr Hematol Oncol 2007;29:506ŌĆō508. PMID: 17609632.


12. Munichor M, Kerner H, Cohen H, Bickel A, Iancu TC. Xanthogranulomatous appendicitis: an incidental finding of localized pathology. Ultrastruct Pathol 2000;24:33ŌĆō39. PMID: 10721150.


13. Antonakopoulos GN, Chapple CR, Newman J, Crocker J, Tudway DC, O'Brien JM, et al. Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med 1988;112:275ŌĆō281. PMID: 3345125.

Fig.┬Ā1
(A-D) Positron emission tomography and computed tomography images at the time of diagnosis showed a hypermetabolic mass suggestive of a lymphoma in the midabdomen and the pelvic cavity.

Fig.┬Ā2
Positron emission tomography scan after completion of aggressive high-dose chemotherapy showed a residual hypermetabolic lesion (arrow) in the right pelvic cavity.
- TOOLS