INTRODUCTION
An intra-abdominal loose body is sometimes observed during laparotomy or autopsy [1]. In most cases, it has a diameter of about 0.5 to 2 cm [2, 3]. A case of an intra-abdominal loose body that was observed in a Korean pediatric patient was reported in 2009 [4]. Some intra-abdominal loose bodies are believed to occur because of adnexal torsion and separation due to the torsion and separation of epiploic appendages [5-8]. Researchers speculate that such small loose bodies grow to giant loose bodies due to intra-abdominal retention of body fluids [5-9].
A giant loose body with a size of more than 4 cm in diameter is very difficult to diagnose before surgery and is rarely diagnosed and reported in clinical practices [10]. Until now, no such case has been reported in Korea. Discrimination between a giant loose body and a tumor or an intra-abdominal foreign body is required before the diagnosis can be confirmed [3]. Although a giant loose body is a rare lesion, careful consideration of this disease could be useful for the diagnosis and treatment of intra-abdominal lesions that show irregular findings.
The authors conducted an explorative laparotomy on a patient who was suspected of having a stromal tumor or teratoma before surgery and experienced a case of giant loose body with a size of 4.5 ├Ś 4.5 ├Ś 3 cm. Accordingly, that case is reported in this paper.
CASE REPORT
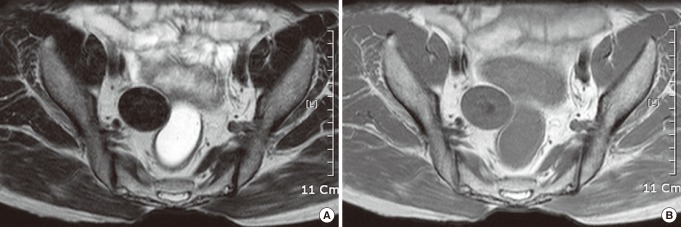
A 60-year-old healthy male patient who had no previous history of disease or medication visited the Seoul Song Do hospital for a regular medical examination. The patient had dyspepsia, but did not complain of abdominal pain and other digestive symptoms such as anorexia, nausea, vomiting, and diarrhea. As a result of computed tomography (CT), an oval-shaped lesion with calcification of the luminal core was observed (Fig. 1). The result of magnetic resonance imaging (MRI) showed a lesion with a size of approximately 4 cm that shared a margin with the rectum and that had signal intensity similar to that of nearby muscle tissues, appearing as a lesion with low intensity in the T1- and the T2-weighted images (Fig. 2).
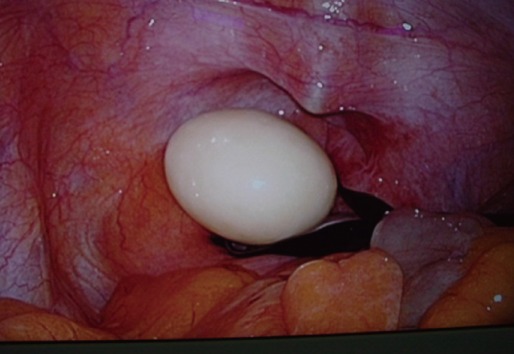
Based on the aforementioned radiological information, a suspected stromal tumor, leiomyoma or teratoma with calcification of the core originating from the rectal wall was diagnosed. Accordingly, the patient underwent laparoscopic surgery. As a result of the surgery, a hard oval-shaped giant loose body that was completely separated from the intrapelvic cavity was found (Fig. 3). The loose body was white, had an elliptical shape with a size of 45 ├Ś 40 ├Ś 30 mm, and had a slightly hard surface (Fig. 4). Histologically, it included central fat necrosis tissues over which fibrosis tissues had formed as a thin layer (Fig. 5).
DISCUSSION
Peritoneal loose body intra-abdominal loose body is sometimes accidentally found during surgery or autopsy [2]. Loose bodies are generally very similar to each other, being white or gray with a soft and light margin and having a density similar to that of rubber [11]. In some cases, it is found as a calcified form. In general, it has a diameter of about 0.5 to 2.5 cm and is freely separated from the inside of the abdominal cavity. However, a loose body with a size of approximately 45 mm is very rare. Despite such a large size, it can be easily removed by laparoscopy without injury related to the surgery.
In general, an intra-abdominal loose body is thought to be formed due to the torsion and separation of epiploic appendages [5, 6]. The torsion, strangulation, and necrosis of epiploic appendages may occur due to inflammation caused by intra-abdominal adhesion, volvulus, intestinal obstruction, or intestinal perforation. Except for a loose body that has undergone normal calcification, no particular pathological importance is found, and no pathology or frequency data are available. However, in some cases, an intra-abdominal loose body has been reported to cause symptoms such as abdominal pain or dyspepsia. In addition, in severe cases, clinical symptoms such as intestinal obstruction may occur [12]. The loose body of the patient in this case report is thought to have been formed by epiploic appendages in the intra-abdomen and to have gradually grown to 45 mm with inflammation, but its exact pathogenesis was unclear.
The discrimination of an intra-abdominal giant loose body from other lesions such as rhabdomyomas, fibrous tumors, desmoid tumors, teratomas, ovarian metastases, urinary stones, gallstones, appendicitis, or calcified lymph nodes is important [3], and CT or MRI can be used for that purpose. In the case of a leiomyoma, it consists of muscle tissues or collagen fiber and has a low signal intensity in the T1- and the T2-weighted images of MRI. Due to this, the discrimination of a leiomyoma from an intra-abdominal loose body is difficult. However, CT is somewhat useful in the process of discrimination because contrast enhancement is achieved in a leiomyoma and a teratoma, but not in a loose body. In addition, an intra-abdominal giant loose body has a homogenous internal region, which is also helpful for discrimination. In microscopic examinations, fat necrosis tissues or calcified tissues that seem to originate from the necrosis of epiploic appendages are sometimes observed in the core of the intra-abdominal loose body. Those tissues are thin and fibrosis, do not have cellular components, and surround the central region.
In most cases, an intra-abdominal loose body is accidentally found as a lesion with a size similar to that of a small bean. If an irregular mass with calcification of the central region is found, a giant intra-abdominal loose body should be suspected [13]. If a peritoneal loose body is suspected, position change imaging will be helpful for diagnosis. The diagnosis of a giant loose body is expected to reduce unnecessary surgical treatments for patients whose giant loose body has been accidentally found asymptomatically.