- Search
| Ann Coloproctol > Volume 36(4); 2020 > Article |
|
Abstract
Purpose
Present an updated classification for symptomatic hemorrhoids, which not only guides the treatment of internal hemorrhoids but also the treatment of external components. In addition, this new classification includes new treatment alternatives created over the last few years.
Methods
Throughout the past 7 years, the authors developed a method to classify patients with symptomatic hemorrhoids. This study, besides presenting this classification proposal, also retrospectively analyzed 149 consecutive patients treated between March 2011 and November 2013 and aimed to evaluate the association between the management adopted with Goligher classification and our proposed BPRST classification.
Results
Both classifications had a statistically significant association with the adopted management strategies. However, the BPRST classification tended to have fewer management discrepancies when each stage of disease was individually analyzed.
Conclusion
Although there is much disagreement about how the classification of hemorrhoidal disease should be updated, it is accepted that some kind of revision is needed. The BPRST method showed a strong association with the management that should be adopted for each stage of the disease. Further studies are needed for its validation, but the current results are encouraging.
Hemorrhoidal disease (HD) is one of the most common anorectal conditions of adulthood. It is estimated to affect approximately 4% of the population, with 50% of people over 50 years-old referring to related symptoms at some point in life [1-3]. Although it is a benign condition, it generates a social burden (as it impacts lifestyle), an economic burden (on health systems), and a social security burden (by the working days lost or harmed by the disease itself) [2].
Hemorrhoids are not, essentially, varicose veins, but vascular cushions composed of veins, sinusoids, arterioles, smooth muscle fibers, and connective tissue that are located in the anal canal [3, 4]. In normal circumstances, hemorrhoids are normal vascular plexuses, detected in all genders and ages, including newborns. Anatomically, the hemorrhoids can be divided as external hemorrhoids (below the dentate line) and internal hemorrhoids (above the dentate line) [3]. The term HD is used when there are complications or related symptoms [3, 4].
In pathological conditions, the hemorrhoidal plexus suffers from venous hypertension and dilation, resulting in complications, such as prolapse (when its origin is above the dentate line), mucous discharge, itching, and thrombosis (resulting in edema and intense pain). The connective tissue of the hemorrhoidal cushions may degenerate over time, especially when there is associated prolapse. This results in the emergence of fibrotic skin tags, which can be very symptomatic, with many patients complaining of local discomfort and soiling [3-5].
It is important to note that HD may be internal, external, or both, with single or multiple prolapses, and there may be hemorrhoidal tissue of different sizes in the same patient [4].
Although all of these symptoms can be related to HD in general, the current (and most used) classification only evaluates the internal hemorrhoids, considering only the existence and extent of prolapse during the evaluation, and it does not take into account external hemorrhoidal thrombosis. Published in 1980, Goligher classification grades the internal hemorrhoids from I to IV [3, 6]. In the first degree, the hemorrhoid plexuses are insinuated through the anal canal during evacuation but do not exteriorize. Second-degree hemorrhoids protrude below the dentate line during the evacuation effort and return spontaneously as soon as the effort ceases. When prolapse occurs and there is a need for manual reduction, the hemorrhoids are classified as third degree. Finally, fourth-degree hemorrhoids are considered irreducible because the vascular cushions are permanently externalized [6].
By the time Goligher classification was published, the management alternatives were limited to medical treatment, outpatient procedures (such as sclerotherapy or rubber-band ligation), and conventional surgery (such as the Milligan-Morgan and Ferguson-Heaton techniques). Therefore, patients classified as having HD grades I and II underwent medical treatment and outpatient procedures, while grades III and IV patients were referred for conventional surgery [6].
However, over the last 30 years, new surgical techniques for the management of HD were developed; they had good acceptance by the medical population and were better preferred by the patients. Such techniques are characterized by not requiring anodermal excision, which results in lesser postoperative pain and discomfort [3, 7, 8].
Despite this modernization, the classification of symptomatic hemorrhoids has not been updated since the publication of the Goligher classification. Many surgical techniques (which are largely used) are not factored into Goligher classification, which is considered to be anachronistic since it may not be able to guide and evaluate the outcomes of the treatment [2, 3].
Thus, it is urgent to propose another method to classify HD since a thorough record of the staging of disease can help in the choice of treatment method and help in evaluating its efficacy [2].
Over the past 7 years, motivated to facilitate teaching on the assessment and management of symptomatic hemorrhoids, the authors developed this classification, which was entitled as âBPRST.â Unlike the most commonly used classification described by Goligher in 1980, our method also includes other signs and symptoms related to the disease, besides considering external hemorrhoids as well. The rationale for this inclusion is that not only the prolapse is determinant for guiding treatment (medical, office procedures, or surgery).
So, in order to evaluate our method capability of predicting management, we retrospectively analyzed 149 medical records of patients that were treated in accordance with the current guidelines and classified them according to Goligher classification and our BPRST classification [3, 9, 10].
The acronym BPRST, created to list and grade the most frequent complaints from patients that seek for medical care, due to hemorrhoids, was inspired by the TNM system, created in the late 1950s by Pierre Denoix and has widely used since the late 1960s for staging malignant neoplasms [11].
In the BPRST classification, each letter corresponds to a specific characteristic of the clinical history and physical examination, where B corresponds to bleeding, P corresponds to prolapse, R corresponds to reduction, S corresponds to skin tags, and T corresponds to thrombosis.
Within this model, the characteristics can be graded according to their intensity or number (seen on physical examination). The details are shown in Table 1. The sum of these characteristics allows the patient to be classified into 3 clinical stages, not necessarily graded by severity, but where each one has a well-established treatment.
Stage I includes patients with bleeding, with no report of prolapse or external components (fibrotic skin tags or thrombosed piles) detectable on physical examination. For these patients, clinical measures (such as lifestyle modifications) are proposed; dietary fiber supplementation, increased water intake, physical activities, or sitz baths [12-14]. Outpatient interventions such as rubber-band ligation, infrared photocoagulation, or sclerotherapy are also indicated on an individual basis [13-16].
Stage II comprises patients with prolapse (whether circumferential or not, regardless of the number of prolapsed piles) that can be reduced spontaneously or by digital maneuver [6, 8]. For these patients, it is feasible to adopt the strategies taken for patients with stage I HD (especially outpatient procedures, also highlighting the possibility of using the high-macro rubber-band macroligation procedure) [13], although the use of non-excisional surgical treatments should be considered; mechanical stapled anopexy (procedure for prolapse and hemorrhoids) [17], transanal hemorrhoidal dearterialization (THD) [18], and radiofrequency ablation [19]. We highlight these treatment options for those with circumferential prolapse, once it is possible to treat all prolapsed piles in a single procedure, differently from rubber-band ligation that requires more than one procedure for that [20].
Finally, stage III comprises patients with irreducible prolapse, symptomatic fibrotic skin tags, or acute hemorrhoidal thrombosis (in which conservative treatment is contraindicated or not improved with conservative treatment). Surgical treatment is indicated by excisional methods (Milligan-Morgan technique, Ferguson-Heaton technique, laser, or Obando technique) [1, 3, 6, 12,15]. However, nonanodermal excision techniques can be an alternative, once the external components (skin tags) are also removed.
The summarized classification, with proposed therapies for each stage, is described in Table 2.
This is a longitudinal observational study, conducted in a single institution, which analyzed 149 medical records of consecutive patients with symptomatic hemorrhoids treated between March 2011 and November 2013; the study aimed to evaluate the association between the Goligher classification and our proposed BPRST classification.
At admission, all patients were classified according to Goligher classification and evaluated for their main complaints and signs found on physical examination. Their treatment was guided according to current guidelines and surgeonâs preference based on the best practice of hemorrhoid care [9, 10].
The patients were followed by us during their treatment. Specifically, 119 patients underwent surgical procedures, whereas 30 patients underwent medical therapy (with painkillers, sitz baths, and ointments) and outpatient procedures, such as rubber-band ligation or sclerotherapy. In our service, we most often adopt rubberband ligation as preferred method for office procedures.
Finally, after completing the treatment of these patients, a retrospective analysis of their medical records was performed, aiming to classify them according to BPRST classification and evaluate its association with the treatment adopted.
This study was previously authorized by the Institutional Review Board of University of SĂŁo Paulo (No. 05156818.2.0000.0068).
Statistical analysis was performed to examine the association between Goligher classification and the BPRST classification with the management adopted in the studied sample. Fisher exact test was used for the statistical analysis, in conjunction with 95% confidence intervals. The database was analyzed with the IBM SPSS Statistics ver. 25 (IBM Corp., Armonk, NY, USA).
The patients included in the study had an average follow-up of 32 months. Most of these patients underwent some surgical treatment during their follow-up (119/149). One reason for this is that many of them exhibit a more advanced disease profile, as they were referred by nonspecialist doctors in the region. Some patients had previously undergone hemorrhoidectomy and relapsed.
Tables 3 and 4 refer to the treatment adopted comparing both classifications. Even though there was a statistical association with Goligher and BPRST classifications, we noticed that several patients who were initially classified as being Goligher classification I were reclassified as BPRST stages I, II, and III and that affected clinical practice (Table 5).
Of the 30 nonsurgical patients, 4 rejected the proposal for surgical treatment (after an episode of acute hemorrhoidal thrombophlebitis). Of these, 3 showed good responses to clinical treatment and one was lost to follow-up (without being able to know if symptoms had resolved).
The study of anorectal diseases, particularly HD, has deepened over the last few years, with the establishment of new therapeutic methods [3, 5, 9, 10, 12, 21, 22]. Such modernization extends the possibilities of treatment, which was once limited to clinical treatment for grade I and II internal hemorrhoids and conventional surgery for grades III and IV [6].
Our goal, in proposing a new classification, was to give a holistic approach to HD, not only contemplating internal hemorrhoids but also focusing on external hemorrhoids. The external hemorrhoids itself and their complications (thrombosis and thrombophlebitis) have a similar pathogenesis to internal hemorrhoids and may also undergo surgical treatment [1, 3, 12]. Because they are behaviorally similar diseases that affect extremely close topographies (and can sometimes coexist), we believe that allocating them to the same classification is the most rational.
Goligher classification does not encompass important features of HD and considers only the presence of prolapse and whether it is (or not) reducible. In addition to being imprecise, the current classification does not consider the number of prolapsed piles, their size, or whether the prolapse is circumferential [8]. This difference influences not only symptomatology but also the management of these cases [3, 5, 8]. Taking as an example the stage II (reducible) hemorrhoids, the prolapses restricted to 1 or 2 piles can be successfully treated in a single office procedure (such as rubber-band ligation), whereas circumferential prolapses mostly require more than 1 session of ligation (or better nonanodermal excision surgical procedures) [13, 14, 20, 21].
Another condition that is extremely prevalent in patients with HD (especially when the disease is more advanced) is the presence of redundant and intolerable skin tags, which result from chronic inflammation and degeneration of the perianal connective tissue and skin; skin tags can cause discomfort, pain, and difficulties in local hygiene, and can sometimes be more bothersome than the HD itself [5].
Therefore, when we proposed our model for the classification of HD, we aimed at 2 goals: to contemplate the disease holistically, addressing not only prolapse but also other equally significant details (such as the presence of external components or thrombosis/thrombophlebitis), and to assist the decision making, as the current classification does not include new forms of treatment (such as stapled anopexy, radiofrequency, or THD).
In the statistical analysis, we noticed a strong association between the presence of acute hemorrhoidal thrombosis in the earliest stages of the disease (mostly classified as Goligher classification I and II). Often, the first consultation with the specialist occurs at this point (also being a determining factor in choosing clinical or surgical treatment).
Another very interesting and statistically significant association was the presence of circumferential prolapse and symptomatic skin tags in patients with more advanced degrees of HD. Although not covered by the Goligher classification, these characteristics are taken into consideration when choosing the best approach (most often surgical). Such associations can be seen in Table 6.
Even with the Goligher classification not considering all clinical features of HD, there was still a strong significant association with the management adopted in the study patients. However, when analyzing each column individually, we noticed discrepancies between the management recommended by Goligher and the treatment adopted, with approximately 35% of Goligher classification I patients and 63% of Goligher classification II patients undergoing surgical procedures.
On the other hand, when we analyzed the association between the BPRST classification and the treatment adopted, we noticed that not only was there an extremely significant association, but also there were no individual discrepancies (when assessing each stage of the disease individually). An exception was made for 4 patients of stage III who refused the surgical treatment offered to them. So far, it is known that 3 of these patients had a satisfactory response to clinical treatment, and 1 patient was lost to follow-up.
The authorsâ objective is to build, in the long term, a prospective database that allows the comparison of this new classification with Goligher classification, and it is possible to reliably assess its impact on decision making (outpatient and surgical treatment). In this way, it will be possible (in future studies) to evaluate its scientific validation.
The cases listed below are examples of the applicability of the BPRST classification in clinical practice.
Case 1: A 67-year-old male patient sought outpatient care for an acute onset of anal pain that worsened when sitting or during evacuation effort, with no improvement after 5 days of painkillers, sitz baths, and anesthetic ointments. On examination, there were no prolapses but a large thrombosed external hemorrhoid. He also reports a history of rectal bleeding, previously diagnosed as internal hemorrhoids (in previous outpatient care, when colonoscopy was performed). According to the Goligher classification, this patient would be considered to have grade I internal hemorrhoids, which has no surgical management at all. Considering that this classification does not contemplate the external hemorrhoids, it would have no value in predicting the management that could be applied to this case. However, by our classification, due to acute hemorrhoidal thrombosis, this patient is classified as having stage III hemorrhoids and is therefore a candidate for conventional surgery (hemorrhoidectomy or even thrombectomy). Therefore, this patient underwent conventional closed hemorrhoidectomy (by the Ferguson-Heaton technique), with excellent postoperative results, and was discharged on postoperative day 1. Fig. 1 show preoperative and immediate postoperative images.
Case 2: A male patient with bleeding complaints on evacuation effort associated with discomfort due to an irreducible prolapse, even with digital maneuvers. In the proctological examination, the irreducible component was restricted to a single (noncircumferential) pile, as shown in Fig. 2A. By Goligher classification, this patient would be a candidate for classical excisional hemorrhoidectomy because he had grade IV internal HD. On the other hand, by the BPRST classification, even though the patient had stage III HD (due to the irreducible prolapse), he could also be submitted to THD because the hemorrhoid was not circumferential. In this patient, THD was performed, with good immediate and late results (at 20 months of follow-up). Fig. 2B shows an immediate postoperative status.
HD has a myriad of clinical presentations, where the prolapse is not the only reason for seeking medical care. Currently, knowledge about HD pathogenesis, natural history, and treatment methods have greatly improved. However, since the current classification has not been updated since its publication, the choice of treatment methods has been delegated exclusively to the surgeon (who makes this decision based on his own experience), since there is no guidance about the new surgical and outpatient managements.
We believe that developing a new classification, which contemplates not only the internal hemorrhoids but also the external hemorrhoids and taking into account other symptoms and clinical signs, can greatly help in choosing the best management and, consequently, contribute to better outcomes. The BPRST classification, as it provides various therapeutic possibilities for each stage of the disease, allows the surgeon to tailor their preferred technique, maintaining the individualization of treatment.
In our survey, BPRST staging was more accurate than Goligher classification and had fewer discrepancies in regard to the treatment adopted for the patients in the sample. Although further studies are needed to validate it, the current results are optimistic. In the near future, a multicentric prospective study will be conducted by the authors.
Fig. 1.
A case of a male patient with the hemorrhoidal disease of BPRST classification stage III. (A) Preoperative status. (B) Immediate postoperative status.

Fig. 2.
A case of a male patient with the hemorrhoidal disease of BPRST classification stage III. (A) Preoperative status. (B) Immediate postoperative status.
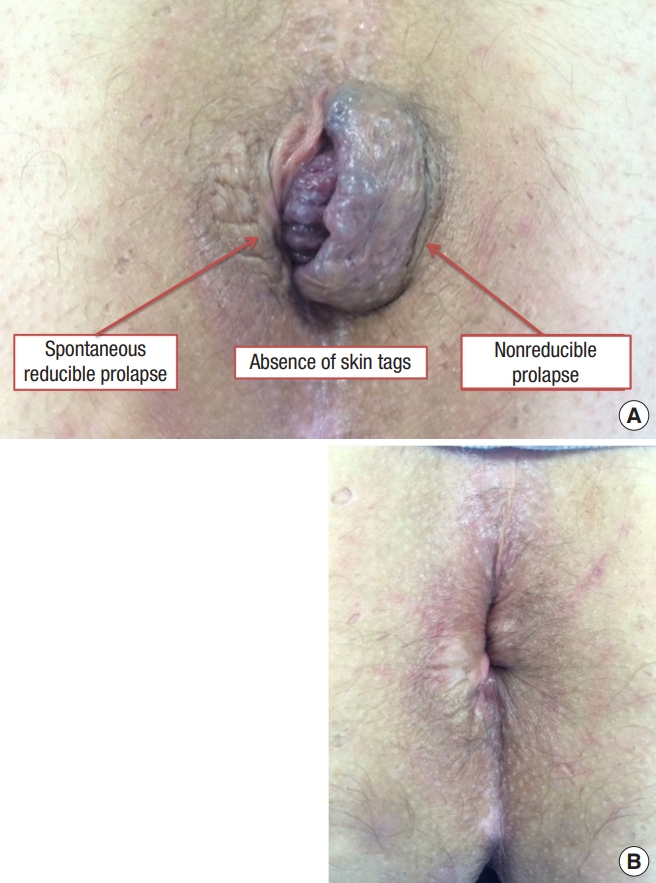
Table 1.
Characteristics evaluated on BPRST classification, with gradation and descriptions
| Bleeding (B) | Prolapse (P) | Reduction (R) | Skin tag (S) | Thrombosis (T) |
|---|---|---|---|---|
| B0 | P0 | R0 | S0 | T0 |
| No bleeding | No prolapse | Spontaneous reduction | No skin tags | Without acute thrombosis |
| B1 | P1 | R1 | S1 | T1 |
| Bleeding | Prolapse of 1 pile | Manual reduction | Symptomatic skin tags | With thrombosisa |
| - | P2 Prolapse of 2 or more piles | R2 Irreducible prolapse | - | - |
Table 2.
Clinical staging of hemorrhoids based on BPRST classification and proposed therapeutic approaches for each stage
| Clinical staging | BPRST descriptiona | Proposed approach |
|---|---|---|
| Stage I | B1 | Lifestyle modifications AND outpatient procedures |
| P0 and R0 and S0 and T0 | ||
| Stage II | Any B | Approaches for stage I AND nonanodermal excision methods (especially if circumferential prolapse) |
| P1 or P2 or R1 | ||
| T0 | ||
| Stage III | Any B | Anodermal excision methods (first option) OR nonanodermal excision methods (associated with excision of external components) |
| Any P | ||
| R2 or S1 or T1 |
Table 3.
Associations between Goligher classification and the treatment adopted
Table 4.
Associations between BPRST classification and the treatment adopted
| Management |
BPRST classification |
||
|---|---|---|---|
| 1 | 2 | 3 | |
| Clinical treatment | 5 (83.3) | 9 (13.0) | 4 (5.4)a |
| Outpatient procedures | 1 (16.7) | 11 (15.9) | 0 (0) |
| Techniques without anodermal excision | 0 (0) | 49 (71.0) | 18 (24.3) |
| Techniques with anodermal excision | 0 (0) | 0 (0) | 52 (70.3) |
Table 5.
Correlation between Goligher and BPRST classifications in the studied sample
| BPRST stage |
Goligher classification |
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| 1 | 6 (35.3) | 0 (0) | 0 (0) | 0 (0) |
| 2 | 2 (11.8) | 28 (60.9) | 39 (60.9) | 0 (0) |
| 3 | 9 (52.9) | 18 (39.1) | 25 (39.1) | 22 (100) |
Table 6.
Association between Goligher classification and different attributes evaluated on BPRST classification
REFERENCES
1. Sneider EB, Maykel JA. Diagnosis and management of symptomatic hemorrhoids. Surg Clin North Am 2010;90:17â32.


2. Rubbini M, Ascanelli S, Fabbian F. Hemorrhoidal disease: is it time for a new classification? Int J Colorectal Dis 2018;33:831â3.



3. Rubbini M, Ascanelli S. Classification and guidelines of hemorrhoidal disease: present and future. World J Gastrointest Surg 2019;11:117â21.



5. Sun Z, Migaly J. Review of hemorrhoid disease: presentation and management. Clin Colon Rectal Surg 2016;29:22â9.




6. Goligher JC. Haemorrhoids or piles. In: Goligher JC, Duthie HL, Nixon HH, editors. Surgery of the anus, rectum and colon. 4th ed. London: BailliĂšre Tindall; 1980. p. 96.
7. Ratto C, CampennĂŹ P, Papeo F, Donisi L, Litta F, Parello A. Transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease: a single-center study on 1000 consecutive cases and a review of the literature. Tech Coloproctol 2017;21:953â62.




8. Gerjy R, Lindhoff-Larson A, Nystrom PO. Grade of prolapse and symptoms of haemorrhoids are poorly correlated: result of a classification algorithm in 270 patients. Colorectal Dis 2008;10:694â700.


9. Davis BR, Lee-Kong SA, Migaly J, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum 2018;61:284â92.


10. Yamana T. Japanese Practice Guidelines for Anal Disorders I. Hemorrhoids. J Anus Rectum Colon 2018;1:89â99.



11. Doll R. The Pierre Denoix Memorial Lecture: nature and nurture in the control of cancer. Eur J Cancer 1999;35:16â23.


12. Lohsiriwat V. Hemorrhoids: from basic pathophysiology to clinical management. World J Gastroenterol 2012;18:2009â17.



13. Reis Neto JA, Reis Junior JA, Kagohara OH, Simoes-Neto J, Banci SO, Oliveira LH. High macro rubber band ligature. J Coloproctol 2013;33:145â50.

14. Reis Neto JA, Quilici FA, Cordeiro F, Dos Reis JA Junior. Tratamento ambulatorial de hemorrĂłidas: estudo prospectivo randomizado. Rev Bras Colo-Proctol 1989;9:131â7. Portuguese.
15. MacRae HM, McLeod RS. Comparison of hemorrhoidal treatment modalities: a meta-analysis. Dis Colon Rectum 1995;38:687â94.


16. Iyer VS, Shrier I, Gordon PH. Long-term outcome of rubber band ligation for symptomatic primary and recurrent internal hemorrhoids. Dis Colon Rectum 2004;47:1364â70.


17. Longo A. Treatment of haemorrhoids disease by reduction of mucosa and haemorrhoidal prolapse with a circular suturing device: a new procedure. In: Montori A, Lirici MM, Montori J, European Association for Endoscopic Surgery, editors, editors. Proceedings of the 6th World Congress of Endoscopic Surgery; 1998 Jun 3-6; Rome, Italy. Bologna: Monduzzi Editore; 1998. p. 777â84.
18. Morinaga K, Hasuda K, Ikeda T. A novel therapy for internal hemorrhoids: ligation of the hemorrhoidal artery with a newly devised instrument (Moricorn) in conjunction with a Doppler flowmeter. Am J Gastroenterol 1995;90:610â3.

19. Gupta PJ. Novel technique: radiofrequency coagulation: a treatment alternative for early-stage hemorrhoids. MedGenMed 2002;4:1.
20. Brown SR, Tiernan JP, Watson AJ, Biggs K, Shephard N, Wailoo AJ, et al. Haemorrhoidal artery ligation versus rubber band ligation for the management of symptomatic second-degree and third-degree haemorrhoids (HubBLe): a multicentre, open-label, randomised controlled trial. Lancet 2016;388:356â64.











