- Search
| Ann Coloproctol > Epub ahead of print |
|
Abstract
Purpose
This study was performed to assess the long-term annual functional outcomes and quality of life (QOL) after transanal rectocele repair.
Methods
We evaluated retrospectively collected data from patients who underwent transanal repair for symptomatic rectocele between February 2012 and December 2018. The Constipation Scoring System (CSS), the Fecal Incontinence Severity Index (FISI), and several QOL questionnaires (e.g., the Patient Assessment of Constipation-QOL [PAC-QOL], Fecal Incontinence QOL, and the 36-Item Short Form Survey [SF-36]) were administered before surgery and annually after surgery. Additionally, physiological assessments and defecography were performed before and after surgery. Substantial symptom improvement, indicated by at least a 50% reduction in the CSS or FISI score, was evaluated postoperatively. All postoperative follow-up results were compared with the preoperative data.
Results
Thirty-two patients were included in the study. The median follow-up period was 5 years (range, 0.5−7 years). Postoperative defecography showed that the rectocele size significantly decreased (P<0.0001). However, the physiological assessment did not reveal postoperative changes. The CSS score 1 year after surgery was significantly lower than the preoperative score (P<0.0001) and remained significantly low until the long-term follow-up. Constipation improved by more than 80% 2 to 5 years postoperatively, and fecal incontinence improved in 2/3 of the patients after 5 years. The PAC-QOL scores significantly improved (all P<0.05) over time until the 3-year and long-term follow-ups, and 6 of the 8 SF-36 scores significantly improved at specific points postoperatively.
A rectocele is a herniation of the anterior rectal wall into the vaginal lumen. The anorectal symptoms of rectocele are a sense of incomplete evacuation, the need to strain, the sensation of a vaginal bulge, the need for vaginal or perineal digitation, rectal pain, and fecal incontinence (FI) [1]. Surgery is considered for patients with rectoceles when conservative treatment fails.
Surgical procedures to repair rectoceles include transvaginal, transanal, transperineal, and transabdominal approaches [2]. Transanal repair has good short-term results in 70% to 90% of cases [3-6]. The long-term crude outcomes of transanal repair have been documented using simple questionnaires to assess symptoms or subjective global satisfaction rating scales to evaluate the procedure’s efficacy; however, information regarding repetitive bowel function or health-related quality of life (QOL) is limited [7-9]. However, findings from global satisfaction scores may not provide enough evidence to comprehensively evaluate the effectiveness of the procedure [2].
This study assessed long-term functional outcomes and QOL after transanal repair in patients with symptomatic rectocele using patient symptom scores and generic and symptom-specific QOL instruments.
This study was a retrospective study and included the first 30 cases with short-term results from our previous study [10]. The Ethical Committee of Kameda Medical Center of Kameda Medical Center approved this study (No. 21-106). Information about the study protocol was made public, and patients were ensured that they could withdraw consent. However, no patients or their relatives subsequently refused to participate in the study.
Patients with symptoms of disordered rectal evacuation, such as obstructed defecation (OD), FI, or a sensation of a vaginal bulge, underwent defecography as part of the investigation plan unless they rejected the examination. Between February 2012 and December 2018, 693 patients underwent defecography, and 242 patients had rectoceles. Rectocele was considered symptomatic if the patient had at least 1 OD symptom (e.g., straining, incomplete evacuation, a sensation of anorectal obstruction, digitation at least once per week, and repeated visits to the toilet), or a sensation of a vaginal bulge or mass, mucus discharge, or post-evacuation FI. Patients with persistent symptoms after failed conservative treatments, such as dietary advice and medication, were candidates for surgical treatment.
Transanal repair was performed when patients had rectocele alone with the above symptoms and/or FI, or rectocele plus rectal intussusception with the above symptoms who were not associated with FI. Rectocele associated with enterocele was not an indication for transanal repair. Patients with enterocele, those with rectal intussusception who had FI symptoms, or those with weak anal sphincter muscles underwent laparoscopic ventral rectopexy (LVR) [11]. Stapled transanal rectal resection (STARR) was performed for symptomatic rectocele and/or rectal intussusception until May 2012 but ceased for female patients in June 2012 because of anal function impairment or possible severe postoperative complications such as rectovaginal fistula. In this study period, STARR was performed for male patients alone with symptomatic rectal intussusception without FI (Table 1). A colonic transit study was not routinely performed.
The patient’s defecatory function was evaluated using the Constipation Scoring System (CSS) and the Fecal Incontinence Severity Index (FISI). CSS quantifies constipation on a 0 to 30-point scale, with a higher score indicating worse constipation [12]. The FISI quantifies incontinence on a 0 to 61-point scale, with a score of 61 indicating total incontinence [13]. In January 2015, the Altomare obstructed defecation syndrome (ODS) score was introduced with the CSS score to quantify OD symptoms on a scale of 0 to 31 points, with a higher score indicating worse OD [14]. A postoperative score was at least 50% lower than the preoperative scores, which was considered a substantial improvement.
The validated Japanese version of the Patient Assessment of Constipation-Quality of Life (PAC-QOL) assesses a patient’s QOL [15] using 4 scales that contain 28 different items related to worries/concerns, physical discomfort, psychosocial discomfort, and satisfaction. The higher the score, the worse the QOL. The validated Japanese version of the Fecal Incontinence Quality of Life scale (FIQL) assesses QOL in patients with FI [16] using 4 scales that contain 29 different items related to lifestyle, coping/behavior, depression/self-perception, and embarrassment with higher scores indicating better QOL. Finally, the validated Japanese version of the 36-Item Short Form Survey (SF-36) evaluates generic QOL, including the 8 scales of physical functioning, role physical, bodily pain, health perception, energy, social functioning, role emotional, and mental health, with scores ranging from on a scale of 0 (lowest QOL) to 100 (perfect QOL) [17].
The transanal repair technique has been previously described in detail [10]. Briefly, in the prone jackknife position under spinal anesthesia, mucosectomy was performed using diathermy with an incision from 1 cm above the dentate line to 7−8 cm up the anterior rectal wall. Next, vertical plication of the muscle wall was performed using interrupted absorbable sutures. Finally, the mucosa was repaired with sutures.
A standardized defecography technique was used. The small bowel was opacified with a mixture containing 100 mL of barium sulfate (100% w/w) and 10 mL of amidotrizoic acid (60% w/w), ingested 2 hours before the procedure. All measurements were obtained from the maximal straining images during defecation. Enterocele was diagnosed when the extension of the bowel loop was located between the vagina and the rectum. Rectoanal intussusception (RAI) was diagnosed when the apex of the rectal intussusception impinged on the internal anal orifice or was intraanal, based on images taken during maximal straining defecation. In contrast to RAI, rectorectal intussusception (RRI) was diagnosed if the apex remained intrarectal and did not impinge on the internal anal orifice. Pelvic floor descent during defecation was measured as the range to which the anorectal junction moved in relation to the inferior margin of the ischial tuberosity. Rectoceles were classified as small (< 2 cm in depth), moderate (2−4 cm in depth), or large (> 4 cm in depth). The size was calculated in a standard fashion in the anterior-posterior dimension by measuring the distance between the ventral part of the anterior rectal wall and an extrapolated line of the expected portion of the rectal wall [18]. Entrapment was noted if the contrast medium remained in the rectocele after straining to defecate.
We used a previously described procedure for anorectal manometry and rectal sensation [19]. Anal pressure was measured using a catheter-tip pressure transducer. The capacity of the rectum was measured by balloon distension, and the volumes for defecation, desire volume, and maximum tolerated volume were obtained.
CSS, ODS, FISI, and QOL questionnaires were administered before surgery and annually after surgery. The questionnaires were delivered to patients by a nurse and self-recorded in the outpatient clinic. Patients received questionnaires by mail or were examined in the outpatient clinic between October and December 2021 for further follow-up. The patients underwent defecography 6 months postoperatively, per standard care. The physiological assessment was repeated 1 year postoperatively.
Quantitative data are presented as medians and ranges. The Mann-Whitney U-test was used for unpaired data and the Wilcoxon signed-rank test for paired data (2-sided test). Univariate correlations were analyzed using Pearson coefficients for continuous variables and the chi-square or Fisher exact tests for qualitative data. Data were analyzed using IBM SPSS Statistics ver. 26 (IBM Corp., Armonk, NY, USA). Statistical significance was set at a P-value of < 0.05.
Eighty-three patients underwent surgery; 159 patients were unwilling to undergo surgery because their symptoms were tolerable. Forty-six patients underwent LVR, and 5 male patients underwent a STARR procedure. The remaining 32 patients underwent a transanal repair. Twenty-three patients had OD alone, 4 had OD and FI, 4 had vaginal bulge or mass sensations, and 1 had FI alone. Overall, 4, 18, and 10 patients had small, moderate, and large rectoceles, respectively. Seven patients without FI had rectal intussusception. None of the patients had pelvic floor dyssynergia (Table 2).
The median operative time was 77 minutes (range, 45−126 minutes) with the median blood loss of 20 mL (range, 5−260 mL). Associated procedures included hemorrhoidectomy (n= 9), surgeries for anal fistula or polyp (n= 2), and excision of carcinoid tumor (n = 1). No mortality or major morbidity occurred. The median length of the postoperative stay was 2 days (range, 1−10 days). Only 1 patient (3.1%) had a minor complication (a wound abscess that resolved with antibiotics) and was discharged 10 days postoperatively. The median follow-up was 5 years (range, 0.5−7 years).
In total, 27 patients (84.4%) had preoperative OD, of which 23 had OD alone and 4 had both OD and FI. A total of 20 patients completed the CSS questionnaire at the median follow-up of 5 years (range, 4.3−7 years), of which 17 (85.0%) had a CSS score at least 50% lower than their preoperative score, while the remaining 3 (15.0%) had persistent OD. Overall, the CSS scores significantly decreased at 1 year after surgery (median score: preoperative, 12 and postoperative, 5; P< 0.0001) and remained significantly decreased for 5 years (Fig. 1).
Furthermore, 10 patients who completed the ODS at the median follow-up of 5 years (range, 4.3−6 years), of which 7 (70.0%) had an ODS score at least 50% lower than the preoperative score. Overall, the ODS scores significantly decreased at 1 year after surgery (median score: preoperative, 11 and postoperative, 3; P = 0.003) and remained significantly decreased at 2, 3, and 5 years after surgery (Fig. 2).
Preoperative vaginal digitation for fecal evacuation was reported in 21 patients. However, it was reported less frequently (preoperative, 21 of 32 patients and postoperative, 2 of 25 patients; P < 0.0001) at the median follow-up of 5 years (range, 4.3−7 years).
Among the included patients, 7 (21.9%) had preoperative FI, 5 had mixed FI and OD, and 2 had FI alone. At the median follow-up of 4.3 years (range, 4.3−5 years), 2 of 3 patients (66.7%) had a FISI score at least 50% lower than their preoperative score. Twenty-three patients did not have FI before surgery. Of them, 1 patient reported FI after 1 year but not at the long-term 5-year follow-up (Fig. 3).
Of the 27 patients with OD before surgery, 23 completed the PACQOL questionnaire preoperatively. The median follow-up was 5.7 years (range, 4.3−7 years). The number of patients who completed the questionnaire at each postoperative time point was inconsistent and decreased with time. All PAC-QOL scales significantly improved over time, until 3 years and at the long-term follow-up. Four of the 5 PAC-QOL scores did not reach statistical significance at 4 years because of the small number of evaluations (Fig. 4).
Six patients with FI before surgery completed the FIQL questionnaire preoperatively. None of the FIQL scales improved over time because of the small number of evaluations (Fig. 5). Of the 32 patients who underwent surgery, 19 completed the SF-36 questionnaire, whereas 13 did not complete the questionnaire or did not receive it preoperatively. The scores for the “energy” and “social functioning” scales significantly improved after 1, 2, and 3 years, and the “role physical” and “role emotional” scores significantly improved after 1 year. The “mental health” and “physical functioning” scores significantly improved after 2 and 3 years, respectively. The remaining 2 scale scores did not change considerably after surgery. None of the SF-36 scores significantly improved at the long-term follow-up (Fig. 6).
Table 3 presents the defecographic findings. Of the 32 patients, 4 did not undergo postoperative examination. Rectocele size significantly decreased after surgery (median value: preoperative, 33 mm and postoperative, 9 mm; P< 0.0001). Pelvic floor descent also significantly decreased after surgery (median: preoperative, 32 mm and postoperative, 27 mm; P< 0.0001). Postoperatively, RRI disappeared in 4 of the 5 patients with preoperative RRI, and RAI disappeared in 1 of 2 patients with preoperative RAI. Postoperative defecography was not performed in the other patient with RAI. Meanwhile, 2 and 1 patients without postoperative OD and FI symptoms had new-onset RRI and RAI, respectively (Table 3). Contrast trapping within the rectocele was significantly less frequent after surgery (preoperative, 32 of 32 patients and postoperative, 18 of 28 patients; P< 0.0001).
Twenty-seven patients with OD underwent postoperative defecography. Rectocele size reduction did not correlate with a 50% minimum decrease in the CSS score at the median follow-up of 5 years (range, 4.3−7 years; coefficient, 0.10; P= 0.720). Additionally, the incidence of a reduction of a 50% minimum decrease in the CSS score at the long-term follow-up did not differ between those with (n= 13) and without (n= 4) barium trapping after surgery (P> 0.999). Additionally, preoperative rectocele size did not correlate with a 50% minimum decrease in the CSS score at the long-term follow-up (n= 20; coefficient, 0.27; P= 0.260). Rectal intussusception or pelvic floor descent before surgery did not affect the long-term clinical outcomes.
The maximum resting pressure, the maximum squeeze pressure, the defecatory desire volume, and the maximum tolerated volume did not change postoperatively (Table 4). However, the maximum resting pressure decreased in 1 patient who developed de novo FI 1 year postoperatively (preoperative, 106 cmH2O and postoperative [after 1 year], 86 cmH2O).
This study annually assessed long-term functional outcomes and QOL after rectocele transanal repair. This technique decreased the rectocele size and improved OD symptoms. Overall, 70% to 80% of patients with preoperative OD experienced sustained improvement postoperatively. Additionally, the PAC-QOL scores significantly improved postoperatively until 3 years and at the long-term follow-up (median, 5.7 years). The long-term results of transanal repair for rectoceles vary among previous studies (50%–83%) [7, 8, 20], which used simple questionnaires to assess symptoms or subjective global satisfaction rating scales to evaluate the procedure’s efficacy, without including validated symptoms or QOL scores. Furthermore, they only performed preoperative and long-term follow-up evaluations. The criteria used to determine the surgical effectiveness influence the results. Therefore, we estimated bowel function using a yearly symptom score and defined substantial functional outcome as a postoperative CSS, ODS, or FISI score at least 50% lower than the preoperative score. As such, we identified that postoperative constipation (assessed by CSS) improved by > 80% 2 to 5 years after surgery. Likewise, FI improved in two-thirds of the patients after 5 years.
Patient selection inevitably influences postoperative outcomes [5]. Arnold et al. [8] performed surgery on 60 patients with constipation, reporting that half remained constipated, and 1/3 were incontinent. The authors postulated that their relatively poor results might be attributed to unselective approach to patients requiring rectocele repair. A randomized study comparing vaginal posterior colporrhaphy and transanal repair for symptomatic rectocele reported that the postoperative posterior vaginal wall prolapse incidence was 7% (1 patient) and 67% (10 patients), respectively [21]. Six of the 10 patients with vaginal wall prolapse in the transanal group had enterocele, a contraindication for transanal repair [3]. However, in a randomized study, patients with enterocele would not be preoperatively excluded entirely because oral contrast medium is not used in defecography. In our study, rectocele associated with enterocele was not an indication of transanal repair. Patients with rectocele alone with OD and/or FI, or rectocele combined with rectal intussusception who did not have FI were selected to undergo transanal repair. Patients with enterocele, those with rectal intussusception who had FI symptoms, or those with weak anal sphincter muscles underwent LVR. STARR was exclusively done for male patients. Because the indication of transanal repair was different from that of LVR or STARR procedure, the authors did not make a comparison among the 3 procedures.
Defecography is the most reliable examination for diagnosing rectocele [9], potentially allowing the surgeon to determine the size of the rectocele and other associated findings, such as rectal intussusception or pelvic floor descent. During defecation, feces trapped in the rectocele impedes evacuation, resulting in prolonged and severe straining and contributing to rectal intussusception and increased pelvic floor descent. However, pre- and postoperative defecography findings do not seem to predict postoperative functional results. For example, we found that long-term symptom improvement could not be predicted based on the preoperative rectocele size, consistent with previous studies [7, 9]. This finding suggests that transanal repair is possible for larger rectoceles not associated with an enterocele [22]. Furthermore, previous studies found that reducing the rectocele size and postoperative barium trapping in the rectum did not affect the long-term outcome [7, 9], in agreement with our study results. We also found that pelvic floor descent decreased postoperatively, consistent with a previous study [23]. This result may be ascribed to the lifting effect of the sutures or decreased straining from improved rectal evacuation.
Approximately 1/3 of patients with rectoceles experience some degree of anal incontinence [24], but data regarding postoperative long-term outcomes in patients with rectoceles associated with anal incontinence are scarce. Abbas et al. [6] reported that the FISI scores improved significantly at the 4-year follow-up in patients with anal incontinence. Additionally, we report a substantial postoperative improvement in FI in 2 of the 3 patients at the long-term follow-up.
This study has evaluated patient-reported outcomes on the effect of transanal repair for rectocele using symptom-specific and global QOL assessments. Thornton et al. [25] used SF-36 to assess patients at a median follow-up of 6.3 years, reporting that the QOL scores neither reflect the extent of improvement nor patient satisfaction and our results support this view. None of the SF-36 scores improved at the median follow-up of 5.7 years in our study. Generally, global QOL assessments, such as SF-36 cannot discriminate differences in clinical severity between individuals. We used symptom-specific questionnaires to evaluate the symptom severity and found that all PAC-QOL scores significantly improved over time until the long-term follow-up. However, only 4 patients reported their FIQL score at the long-term follow-up, and this sample size was too small for within-group comparisons.
The effect of transanal repair on anorectal physiology remains debatable. Previous studies have reported a significant decrease in anal resting and squeeze pressure following transanal repair [26, 27]. Thornton et al. [25] documented a significant postoperative decline in anal resting pressure in patients who underwent transanal rectocele repair compared to those who underwent laparoscopic rectocele repair. In contrast, Heriot et al. [5] reported the resting and squeeze pressures did not change postoperatively, consistent with our findings. Roman and Michot [7] found the resting pressure did not differ between patients who reported recurrence and those who were recurrence-free at the long-term follow-up. However, the resting pressure decreased postoperatively in 1 patient who developed de novo FI 1 year postoperatively in our study. The possible decrease in anal pressure may be secondary to the degree of anal dilatation required to achieve transanal repair [26, 27]. Therefore, surgeons must take care not to stretch the anal canal excessively during the procedure and repair the rectocele as quickly as possible. Deteriorated anal pressure may also disturb FI with age.
Preoperative vaginal digitation has been reported in 40% to 80% of patients with rectoceles [5, 7, 23]. In this study, the need to digitally support rectal evacuation significantly decreased at the long-term follow-up compared with the preoperative condition (66% preoperatively vs. 8% 5 years postoperatively). Additionally, the digitation incidence at the long-term follow-up was comparable with that reported in a previous study (9% 4 years postoperatively) [6].
This study was limited by the small sample size, the decreasing number of evaluated patients over time, and the lack of a control group. Furthermore, we did not assess the CSS and FISI scores in all patients and only used the ODS evaluation in a few patients. The questionnaires were not offered to or collected from all patients every time. Thus, the loss of patients in our follow-up might have influenced the results; possibly, patients dissatisfied with the surgical results were less likely to complete the assessments.
In conclusion, transanal repair provided sustained OD improvement in 70% to 80% of patients. Constipation-specific QOL significantly improved over time until 3 years and at the long-term follow-up. These results suggest that transanal repair is a reliable technique to repair symptomatic rectoceles. Further studies are needed to assess long-term functional effects using patient symptom scores or QOL evaluations to objectively confirm the usefulness of this procedure and reliably compare the reported results.
Fig. 1.
Constipation Scoring System (CSS) scores. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. aReduction of at least 50% in CSS score after transanal repair. *P<0.0001, †P<0.01 vs. preoperative (Wilcoxon signed-rank test).
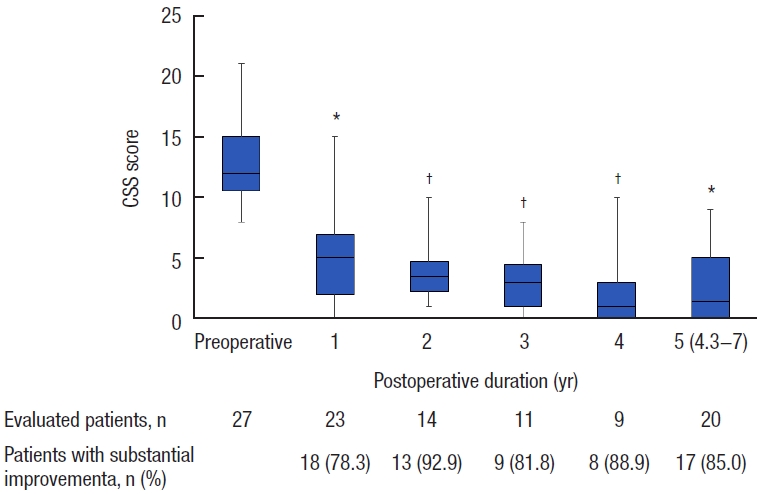
Fig. 2.
Obstructed defecation syndrome (ODS) scores. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. aReduction of at least 50% in ODS score after transanal repair. †P<0.01, §P=0.05 vs. preoperative (Wilcoxon signed-rank test).
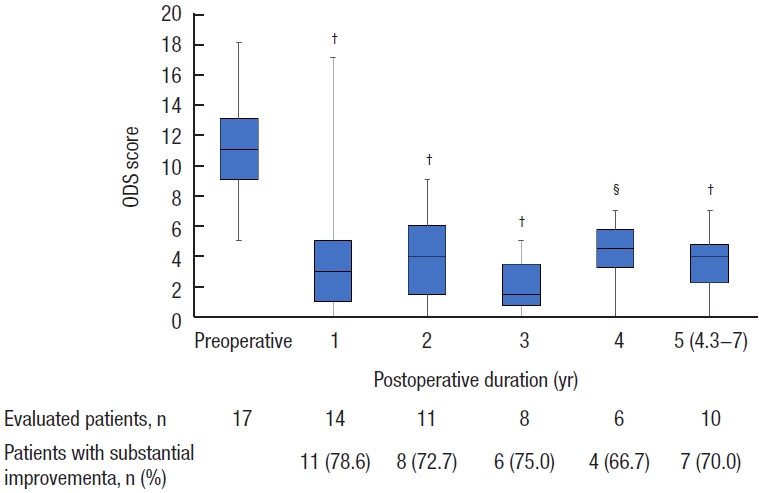
Fig. 3.
Fecal Incontinence Severity Index (FISI) scores. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. aReduction of at least 50% in FISI score after transanal repair. #P>0.05 vs. preoperative (Wilcoxon signed-rank test).
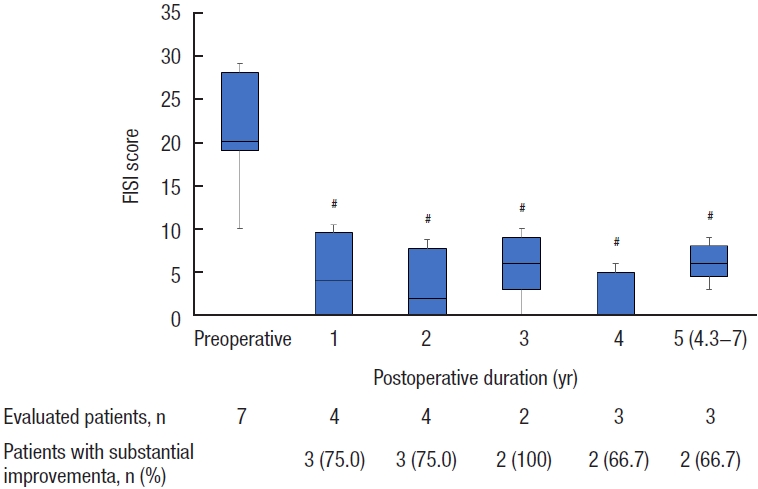
Fig. 4.
The Patient Assessment of Constipation-Quality of Life scores in patients with rectocele (n=23). (A) Worries/concerns, (B) physical discomfort, (C) psychological discomfort, (D) satisfaction, and (E) overall score. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. a5.7 years (range, 4.3–7 years). *P<0.0001, †P<0.01, §P=0.05 vs. preoperative (Wilcoxon signed-rank test).
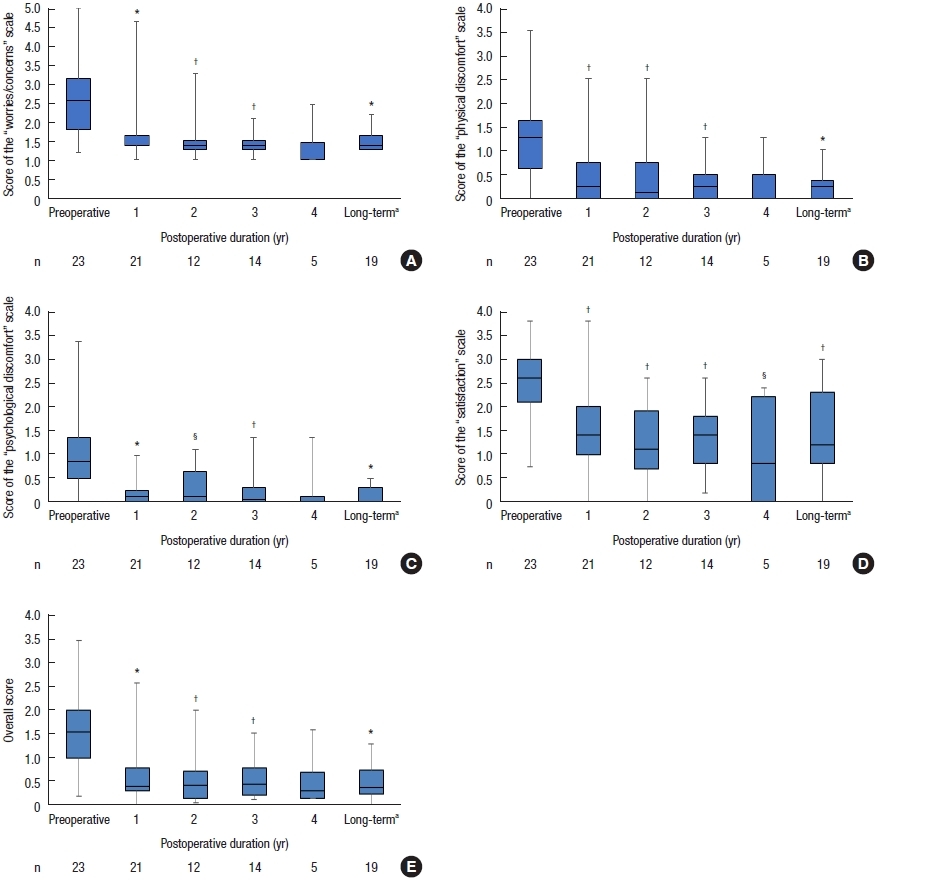
Fig. 5.
Fecal Incontinence Quality of Life scale scores. (A) Lifestyle, (B) coping/behavior, (C) depression/self-perception, and (D) embarrassment. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. #P>0.05 vs. preoperative (Wilcoxon signed-rank test).
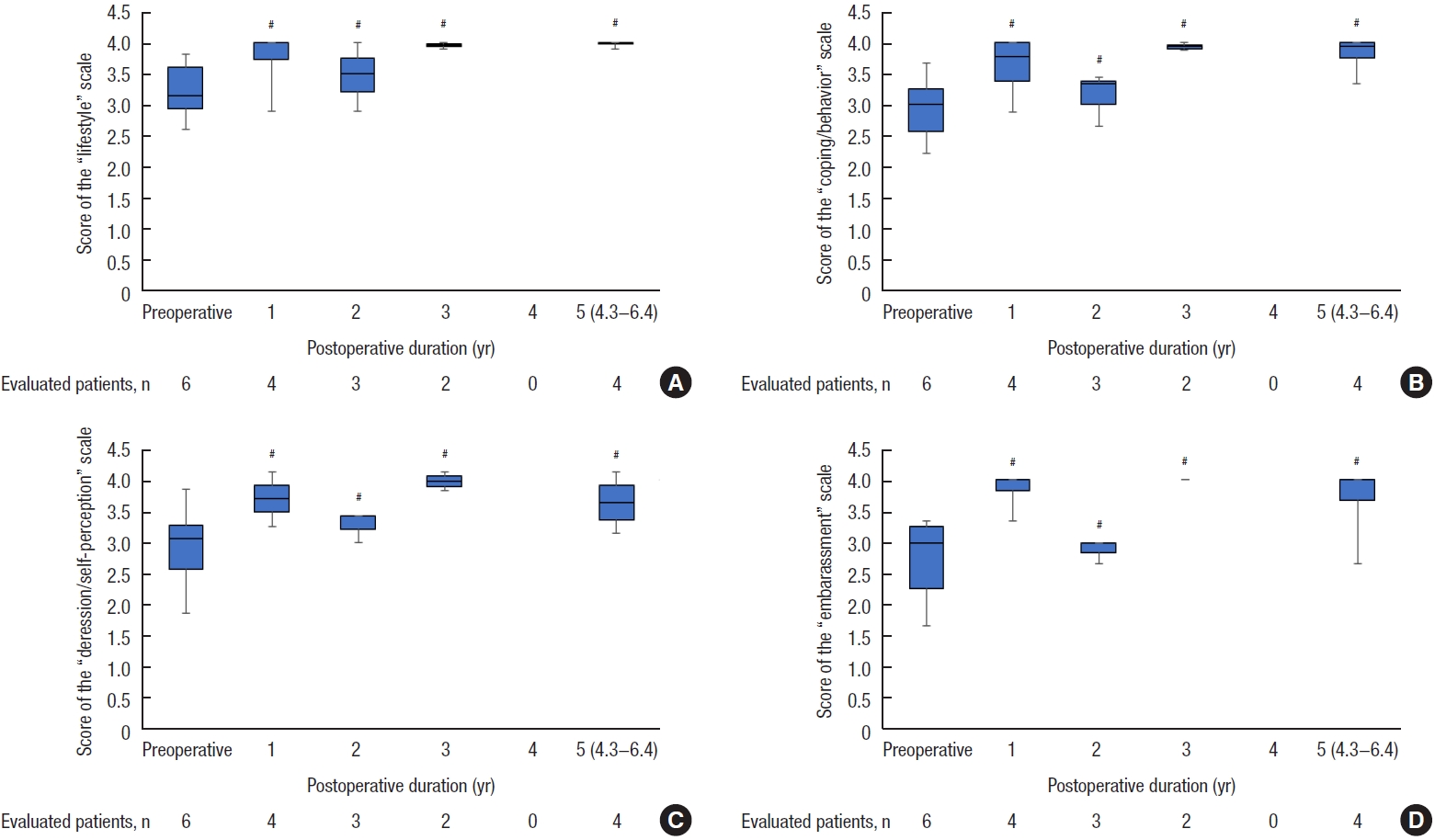
Fig. 6.
Short-Form 36 Health Survey scores in patients with rectocele (n=19). (A) Physical functioning, (B) role physical, (C) energy (vitality), (D) social functioning, (E) role emotional, and (F) mental health. Boxes show median values with upper and lower quartiles. The vertical line extends from the minimum to the maximum values. a5.7 years (range, 4.3–7 years). †P<0.01 and *P<0.05 vs. preoperative (Wilcoxon signed-rank test).
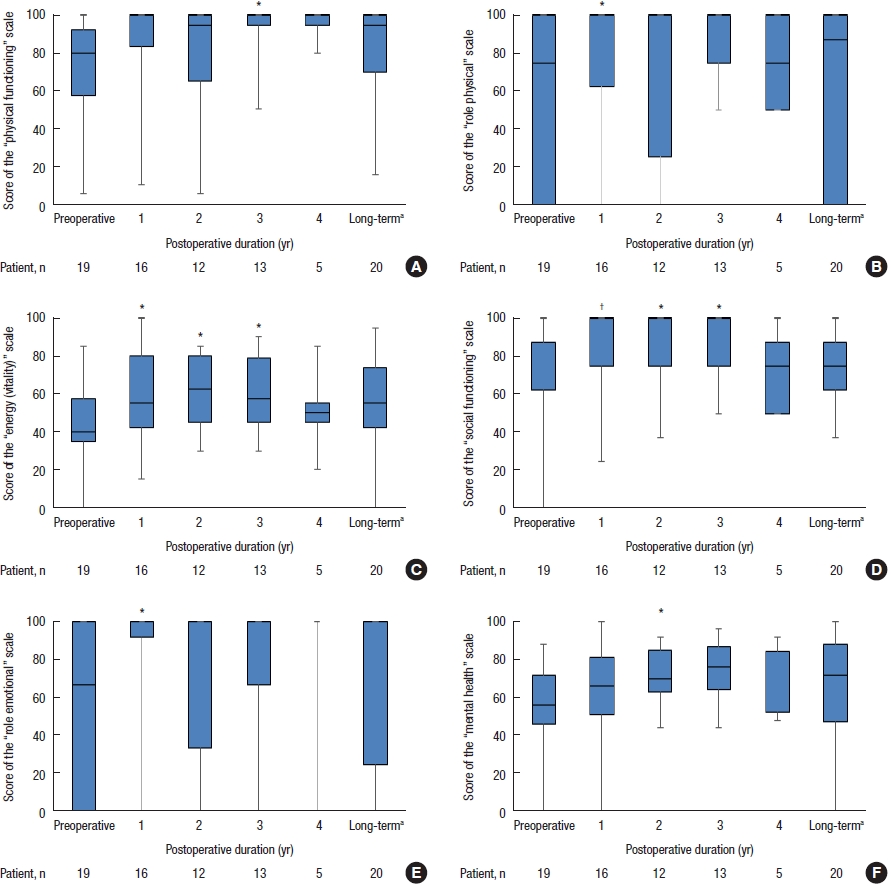
Table 1.
Indication of surgery for symptomatic rectocele and/or RI
| Variable | Transanal repair | LVR | STARR | |
|---|---|---|---|---|
| Rectocele | Alone | + | − | − |
| Plus RI without fecal incontinence | + | +/− | − | |
| Plus RI with FI | − | + | − | |
| Plus enterocele | − | + | − | |
| RI | Alone without FI | − | − | + |
| Alone with FI | − | + | − |
Table 2.
Characteristics of patients
Table 3.
Defecography findings
| Variable | Preoperative (n = 32) | Postoperative 6 mo (n = 28) | P-value |
|---|---|---|---|
| Rectocele size (mm) | 33 (14−52) | 9 (0−28) | < 0.0001a |
| Entrapment | 32 | 18 | < 0.0001b |
| Pelvic floor descent (mm)c | 32 (14−55) | 27 (7−52) | < 0.0001a |
| Rectorectal intussusception | 5 | 3 (2d) | |
| Rectoanal intussusception | 2 | 1d |
Table 4.
Anorectal manometry and volumetric tests
| Variable | Preoperative (n=29) | 1 year (n=24) | P-valuea |
|---|---|---|---|
| MRP (cmH2O) | 97 (36−185) | 89 (42−155) | 0.450 |
| MSP (cmH2O) | 213 (100−491) | 230 (122−385) | 0.510 |
| DDT (mL) | 80 (25−300) | 75 (50−190) | 0.540 |
| MTV (mL) | 180 (48−300) | 200 (95−350) | 0.270 |
REFERENCES
1. Lubowski DZ, King DW. Obstructed defecation: current status of pathophysiology and management. Aust N Z J Surg 1995;65:87–92.


2. Grossi U, Horrocks EJ, Mason J, Knowles CH, Williams AB; NIHR CapaCiTY working group, et al. Surgery for constipation: systematic review and practice recommendations: results IV: recto-vaginal reinforcement procedures. Colorectal Dis 2017;19 Suppl 3:73–91.

3. Janssen LW, van Dijke CF. Selection criteria for anterior rectal wall repair in symptomatic rectocele and anterior rectal wall prolapse. Dis Colon Rectum 1994;37:1100–7.


4. Khubchandani IT, Clancy JP 3rd, Rosen L, Riether RD, Stasik JJ Jr. Endorectal repair of rectocele revisited. Br J Surg 1997;84:89–91.



5. Heriot AG, Skull A, Kumar D. Functional and physiological outcome following transanal repair of rectocele. Br J Surg 2004;91:1340–4.



6. Abbas SM, Bissett IP, Neill ME, Macmillan AK, Milne D, Parry BR. Long-term results of the anterior Délorme’s operation in the management of symptomatic rectocele. Dis Colon Rectum 2005;48:317–22.

7. Roman H, Michot F. Long-term outcomes of transanal rectocele repair. Dis Colon Rectum 2005;48:510–7.


8. Arnold MW, Stewart WR, Aguilar PS. Rectocele repair. Four years’ experience. Dis Colon Rectum 1990;33:684–7.

9. van Dam JH, Ginai AZ, Gosselink MJ, Huisman WM, Bonjer HJ, Hop WC, et al. Role of defecography in predicting clinical outcome of rectocele repair. Dis Colon Rectum 1997;40:201–7.


10. Tsunoda A, Takahashi T, Kusanagi H. Transanal repair of rectocele: prospective assessment of functional outcome and quality of life. Colorectal Dis 2020;22:178–86.



11. Tsunoda A, Ohta T, Kiyasu Y, Kusanagi H. Laparoscopic ventral rectopexy for rectoanal intussusception: postoperative evaluation with proctography. Dis Colon Rectum 2015;58:449–56.

12. Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 1996;39:681–5.


13. Rockwood TH, Church JM, Fleshman JW, Kane RL, Mavrantonis C, Thorson AG, et al. Patient and surgeon ranking of the severity of symptoms associated with fecal incontinence: the fecal incontinence severity index. Dis Colon Rectum 1999;42:1525–32.

14. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis 2008;10:84–8.


15. Tsunoda A, Yamada K, Takano M, Kusanagi H. The translation and validation of the Japanese version of the patient assessment of constipation quality of life scale. Surg Today 2016;46:414–21.



16. Tsunoda A, Yamada K, Kano N, Takano M. Translation and validation of the Japanese version of the fecal incontinence quality of life scale. Surg Today 2013;43:1103–8.



17. Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol 1998;51:1037–44.


18. Bartram CI, Turnbull GK, Lennard-Jones JE. Evacuation proctography: an investigation of rectal expulsion in 20 subjects without defecatory disturbance. Gastrointest Radiol 1988;13:72–80.



19. Tsunoda A, Takahashi T, Hayashi K, Yagi Y, Kusanagi H. Laparoscopic ventral rectopexy in patients with fecal incontinence associated with rectoanal intussusception: prospective evaluation of clinical, physiological and morphological changes. Tech Coloproctol 2018;22:425–31.



20. Murthy VK, Orkin BA, Smith LE, Glassman LM. Excellent outcome using selective criteria for rectocele repair. Dis Colon Rectum 1996;39:374–8.


21. Nieminen K, Hiltunen KM, Laitinen J, Oksala J, Heinonen PK. Transanal or vaginal approach to rectocele repair: a prospective, randomized pilot study. Dis Colon Rectum 2004;47:1636–42.


22. Sullivan ES, Leaverton GH, Hardwick CE. Transrectal perineal repair: an adjunct to improved function after anorectal surgery. Dis Colon Rectum 1968;11:106–14.

23. Karlbom U, Graf W, Nilsson S, Påhlman L. Does surgical repair of a rectocele improve rectal emptying? Dis Colon Rectum 1996;39:1296–302.


24. Meschia M, Buonaguidi A, Pifarotti P, Somigliana E, Spennacchio M, Amicarelli F. Prevalence of anal incontinence in women with symptoms of urinary incontinence and genital prolapse. Obstet Gynecol 2002;100:719–23.


25. Thornton MJ, Lam A, King DW. Laparoscopic or transanal repair of rectocele?: a retrospective matched cohort study. Dis Colon Rectum 2005;48:792–8.


- TOOLS
-
METRICS

-
- 1 Crossref
- Scopus
- 1,758 View
- 44 Download
- Related articles in ACP







