- Search
| Ann Coloproctol > Volume 40(1); 2024 > Article |
|
Abstract
Purpose
The use of an ostomy for urination and defecation leads to reduced quality of life. Although many ostomy management strategies are needed, such strategies are often implemented by patients. Thus, there is a need for a home health care service platform that can be used in ostomy patient management.
Methods
We developed an ostomy patient management platform by identifying the needs of patients and medical staff through the Chronic Care Ostomy Self-Management Training Program in the United States and from studies conducted in Korea.
Results
The platform encompassed physical management, psychological management, maintenance of social function, spiritual stability, and home medical care. These components were implemented through monitoring, self-care guidance, and a community platform. For the monitoring function, patients entered their health status in a mobile application (app); the medical staff at the affiliated hospital then monitored the stoma status through a web interface.
Conclusion
Our platform allows medical staff to monitor ostomy patients through a web interface and help such patients to fully manage their ostomy at home using an app. We expect that the continued development of patient-oriented functions in our app will allow ostomy patients to experience quality-of-life improvements.
An ostomy or artificial anus refers to a passage through which urine or feces is artificially discharged from the abdominal wall as a result of disease (e.g., congenital anomaly, inflammatory bowel disease, or cancer); it may be permanent or temporary [1]. The numbers of cases of inflammatory bowel disease and colorectal cancer—both of which inevitably require a stoma—are increasing in Korea [2, 3]. Accordingly, the number of ostomy patients registered as disabled in Korea increased from 13,072 in 2010 to 15,427 in 2020 [4].
When an ostomy is established after surgical treatment of a life-threatening disease, the patient’s life expectancy is generally prolonged. However, the use of an ostomy for urination and defecation requires many changes that reduce the patient’s overall quality of life. Patients complain of sexual problems, depression, difficulty managing the artificial stoma, constipation, dissatisfaction with appearance, difficulty changing clothes, difficulty traveling, and fatigue [5]. Therefore, continuous management is crucial after stoma establishment. However, many problems must be solved by patients themselves after discharge from the hospital. Thus, we developed a mobile application (app) and a web-based digital health platform that can facilitate stoma management by ostomy patients.
This study was prepared based on the existing literatures, and no individual patient information was included. Therefore, it was not subject to approval from the Institutional Review Board.
In the late 1990s, the Chronic Care Model was developed in the United States for organizational support of human and medical systems, with the aim of helping patients to manage their chronic diseases [6]. Among diverse types of programs based on this model, the Chronic Care Ostomy Self-Management Training Program (CCOSMTP) was developed for ostomy care; it laid the foundation for the development of a program that could facilitate stoma management by ostomy patients and improve daily life for those patients [7].
The CCOSMTP model was developed through surveys using the City of Hope-Quality of Life-Ostomy questionnaire, a focus group, and reviews of various studies (concerning social factors, patient symptoms, and comorbidities) to understand the needs of ostomy patients [7]. This model consisted of four components that required separate physical, psychological, social, and spiritual programming. Clinical trials to facilitate programs for each component have been conducted; the programs have allowed medical staff to provide regular education to patients via telemedicine [8, 9].
In Korea, many related studies have been performed (particularly in the nursing field) concerning the type of discomfort experienced by an ostomy patient and the degree of effort needed to manage that discomfort. Upon discharge from the hospital, ostomy patients have nursing needs for treatment and prognosis; such needs include psychological support, complication management, and dietary management [10]. Ostomy patients also experience difficulties in the implementation of treatment instructions, use of treatment instruments and equipment, and interaction with treatment professionals [11]. Furthermore, patients with a permanent or temporary stoma require detailed information regarding the stoma, rapid access to medical staff, management of fear related to the stoma, and explanations of examination and treatment information [12]. They also complain of difficulties eating, managing their stool, and engaging in social activities [13]. Therefore, the four components (physical, psychological, social, and spiritual programming) included in the CCOSMTP model can be similarly applied to ostomy patients in Korea.
Based on a literature review, we developed a non–face-to-face service platform for at-home management of ostomy patients, with consideration of the following essential components: physical management, psychological management, maintenance of social function, spiritual stability, and home medical care. These components were implemented through three functions: monitoring, self-care guidance, and a community for ostomy patients. These functions were configured within a platform that was developed as an app and a website. The app and website establish a connection between ostomy patients and medical staff who specialize in stoma management and self-care for ostomy patients (Fig. 1).
The monitoring function for discharged ostomy patients enables systematic patient management through a smartphone app; this is more robust than traditional patient management through a conventional telephone. A patient can be asked to upload several stoma pictures for assessment through their smartphone; guidance markers are displayed on the smartphone screen to ensure that the correct area is photographed. Stoma complications (e.g., bleeding, prolapse, hernia, necrosis, ischemia, stenosis, depression, intestinal obstruction, fistula formation, or mucosal skin boundary separation), skin complications (e.g., irritant contact dermatitis, allergic dermatitis, folliculitis, candidiasis, pyoderma gangrenosum, periosteal varices, softening/infiltration, epidermal hypertrophy, or physical damage), and information concerning the stoma bag cycle, weight, and other side effects were collected and used for education and counseling.
Patients living with a stoma can experience difficulty maintaining a healthy life because they lack knowledge and are recovering from physical damage. Therefore, it is important to reduce these burdens and support a rapid return to daily life through the use of an appropriate lifestyle guide. Some guides have been proposed for physical, psychological, and social well-being (Table 1). The main guides referenced in the app are the patient guide published by the United Ostomy Associations of America Inc (UOAA), the travel and exercise guide published by the Ileostomy and Internal Pouch Association (IA), and the symptom coping guide for cancer patients published by the Korean Oncology Nursing Society and the Korean Cancer Study Group [1, 14–18]. Each well-being category includes guidance concerning difficulties with replacing the stoma bag, difficulties with daily life and social activity, difficulties with diet and nutrition, the management of frequent stool leakage, and psychological problems. The app is configured to provide relevant guidance for specific patient questions.
Guidance for physical well-being includes the provision of customized stoma management, provision of checklists for stoma management, management of stoma product inventories, and considerations regarding nutrition and physical activity. Patients discharged from the hospital may not be accustomed to replacing the stoma bag; the suggested guide in the app may help them to manage this task. Additionally, ostomy patients may experience difficulty preparing a stoma-compatible diet; the nutritional management guide can provide helpful information [17]. This management guide contains stoma-specific recommendations concerning water intake and dietary habits. Moreover, the importance of physical activity may be underestimated by ostomy patients; their recovery may be delayed because of insufficient physical activity. Thus, the suggested physical activity guide in the app can help patients to quickly improve their health. The app provides pictures and videos to help patients follow the recommended physical activities [14], warnings about specific activities, and explanations of stoma-specific exercise modifications [16]. In addition, psychological problems can develop in ostomy patients. Because most of these patients have impaired body image recognition, self-esteem, depression, sexual problems, and low psychosocial adaptation [19], the app provides guidance to alleviate stoma-related psychological symptoms and to stabilize mood through meditation and abdominal respiration; it also assists with self-management [18]. Ostomy patients may experience difficulties controlling stool, which limits their ability to engage in social activities [13]. A guide for maintaining social function; engaging in travel, transportation, and sex; and returning to daily work will assist ostomy patients in their daily social activities is also provided (Table 2) [1, 15].
According to a report published by the Korea Disabled People’s Development Institute, most ostomy patients are discharged from the hospital without adequate education; they gain useful tips through trial and error, which is a painful process [20]. In addition, patients will likely find it difficult to attend external education because of the psychological burden. Accordingly, there might be a demand for community support at the time of discharge. The community function for the social and spiritual well-being of ostomy patients consists of functions that connect people outside the home, such as ostomy patient gatherings, bulletin board communities, and the provision of a space for sharing welfare benefits with ostomy patients. In addition, a bulletin board related to a specific religion or belief in the community may be used to share spiritual beliefs.
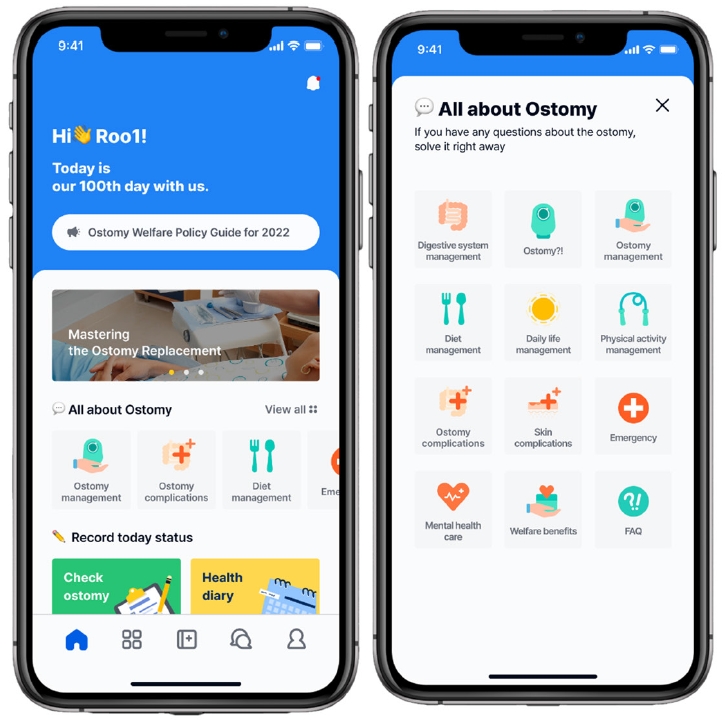
Patients discharged from the hospital after surgery are registered as outpatients; they receive a registration number and temporary app password from the app administrator. They access the home screen after logging in using the given information; available sections are “all about ostomy” (containing stoma information) and “health records.” The ostomy information section provides information necessary for daily life, such as an introduction to the digestive system, methods to manage the ostomy, types of ostomy complications, replacement of the ostomy bag, diet management, and a checklist for emergency management. Such information supplements the patient’s physical, psychological, and social well-being. In the “health records” section, patients enter their ostomy status and receive feedback from the medical staff through regular checkups twice monthly on a set date through the “check ostomy” function; this function directly addresses the patient’s physical well-being. In addition, the “health diary” function enables patients to make daily entries regarding their weight, water intake, bowel movements, and meals consumed.
Ostomy inspections can be initiated by the patient or the patient’s guardian; they begin by determining the patient’s body weight and major problems requiring education (e.g., difficulty replacing the stoma or difficulties with diet and nutrition). The questionnaire about stoma and skin complications may differ depending on the type of ostomy (e.g., colostomy or ileostomy). Then, patients are asked to upload three photos of their stoma and skin condition for assessment by medical staff; a video guide is provided for an accurate collection of images containing the front, left, and right sides of the stoma. In addition, patients can ask questions in the app before they submit the questionnaire. Medical staff at the affiliated hospital will review the submitted documents within a few days to evaluate the patient’s stoma status; they provide feedback to the patient in the app. The patient confirms receipt of the feedback and explains whether they understand the information provided by the medical staff. The community function within the app supports social well-being in ostomy patients; it allows information exchange between patients and the support system. Registered patients support each other by clicking the support button or writing comments for a new post on the community bulletin (Fig. 2).
The web-based administration platform is a system in which the medical staff of the affiliated hospital access and manage information entered through the app. After login, the staff can view information (e.g., the total number of patients to be managed, patient sex, distribution of stoma types, and number of recent stoma inspections) along with graphs on the dashboard. In terms of stoma inspection, stomas can be managed according to the date of each patient’s regular ostomy check; the questionnaire is completed and feedback is provided by the medical staff. A separate patient list is created with the names of individuals who have not requested an ostomy check on the expected day; if a patient does not request the ostomy check service after 3 days of push notification reminders, medical staff will directly contact the patient and remind them to request the ostomy check service.
Each patient is evaluated on the ostomy check screen; medical staff review basic patient information, ostomy management records, health diary data, and any graphs or photos. The medical staff checks the questionnaire and stoma photos entered through the app; they then enter the evaluation and consultation details. When all items have been entered, the full document is printed in the form of a report and exported from the web interface. In addition, the health diary data and any graphs or photos allow medical staff to identify health problems that require more than a standard stoma inspection before the next outpatient visit (Fig. 3).
To improve health status and quality of life in patients with a stoma, a mobile app has been developed as well as a web-based administration platform for medical staff who engage in ostomy care. As a previous review study suggests that mobile app use has become commonplace for a variety of health-promoting behaviors in addition to physical activity and weight control [21], ostomy care through the mobile app might become a part of daily life effectively. In addition, this mobile app can bring many advantages for medical staff in virtue of no time constraint and direct collection of abundant health data from each patient, which enables more thorough evaluation of patients’ health status.
However, some limitations may exist for these digital platforms to settle down in the health care system. Among them, obstacles to licensing and regulation of mobile apps should be mainly considered. There are still few guidelines on the regulation of digital health software or apps, so it is hard for developers to expect the scope of regulation. Therefore, practical use of these apps will be possible only when specific guidelines for licensing and regulation are established.
Medical staff can access and manage information entered in the mobile app; thus, it is easy to understand the patient’s condition remotely and reduce the burden of additional medical treatment. In addition, outcomes can be improved when patients continuously use these functions in the app to manage their stoma. Thus, ostomy patients learn how their stoma functions and whether they have correctly replaced the stoma bag. They can also check the stoma and skin condition, stoma-related complications, outpatient schedule, diet/nutrition/weight, and mental health. Even though the target users are the elderly who may not be accustomed to fully exploiting functions of smartphone apps, a high rate of smartphone penetration in Korea will gradually help overcome this limitation. We expect that the continued development of patient-oriented functions in our app will allow ostomy patients to experience the quality-of-life improvements.
Notes
Conflict of interest
Seongwoo Yang and Kyounghoon Park participated in the study as employees of HERINGS (Seoul, Korea).
Acknowledgments
As part of preparation for the home treatment pilot project for cancer patients in Korea, this paper was audited by the Korean Wound and Ostomy Study Group of The Korean Society of Coloproctology (Seoul, Korea). The authors would like to thank all reviewers.
Table 1.
Functions included in the self-care solutions
| Function | Domain | Subject | Topic |
|---|---|---|---|
| Guidance | Physical well-being | Ostomy management | • Customized ostomy management guide |
| • Stoma-care checklist | |||
| • Stoma supply management | |||
| Diet | • Dietary considerations after surgery | ||
| • Information about food that can and cannot be eaten | |||
| Physical activity | • Appropriate activities for ostomy patients | ||
| • Warnings about specific activities | |||
| Psychological well-being | Psychological symptoms | • Management of fatigue, anxiety, and depression | |
| • Guidance for deep breathing and meditation | |||
| Self-management | • Guidance to promote self-management | ||
| Social and spiritual well-being | Daily life guidance | • Travel tips for ostomy patients | |
| • Transportation guidance | |||
| • Intimacy guidance | |||
| • Returning to the workplace | |||
| Community | Social and spiritual well-being | Support group | • Bulletins for sharing information about stoma care and communication |
| • Explanations of benefits for disabled people through the Korean Ostomy Association (http://www.ostomy.or.kr/) | |||
| • Connection to related communities | |||
| Spiritual community | • Bulletins for sharing religious or spiritual values among ostomy patients |
Table 2.
Components of well-being addressed in ostomy patient guides
REFERENCES
1. In: Settlemire I. editor. New ostomy patient guide. United Ostomy Associations of America Inc; 2021.

2. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat 2020;52:335–50.




3. Kwak MS, Cha JM, Lee HH, Choi YS, Seo SI, Ko KJ, et al. Emerging trends of inflammatory bowel disease in South Korea: a nationwide population-based study. J Gastroenterol Hepatol 2019;34:1018–26.



4. Korean Ministry of Health and Welfare in Korea. [Registration of persons with disabilities (2020)] [Internet]. Korean Ministry of Health and Welfare; 2021 [cited 2021 Dec 1]. Korean. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_11732S0101&conn_path=I2
5. Vonk-Klaassen SM, de Vocht HM, den Ouden ME, Eddes EH, Schuurmans MJ. Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res 2016;25:125–33.




6. Ercolano E, Grant M, McCorkle R, Tallman NJ, Cobb MD, Wendel C, et al. Applying the chronic care model to support ostomy self-management: implications for oncology nursing practice. Clin J Oncol Nurs 2016;20:269–74.



7. Grant M, McCorkle R, Hornbrook MC, Wendel CS, Krouse R. Development of a chronic care ostomy self-management program. J Cancer Educ 2013;28:70–8.




8. Grant M, Sun V, Tallman NJ, Wendel CS, McCorkle R, Ercolano E, et al. Cancer survivors’ greatest challenges of living with an ostomy: findings from the Ostomy Self-Management Telehealth (OSMT) randomized trial. Support Care Cancer 2022;30:1139–47.



9. Weinstein RS, Holcomb MJ, Mo J, Yonsetto P, Bojorquez O, Grant M, et al. An ostomy self-management telehealth intervention for cancer survivors: technology-related findings from a randomized controlled trial. J Med Internet Res 2021;23:e26545.



10. Ju AR, Yeoum SG, Park KS. The nursing needs of post-surgical colon cancer patients at discharge. J Korean Acad Fundam Nurs 2009;16:392–401. Korean.

11. Oh EG, Sung JH, Park YS, Lee HJ, Kim YK. Physiological functional status and the levels of unmet care needs after discharge in patients with chronic pulmonary disease, colorectal cancer, and strokes. J Korean Clin Nurs Res 2016;22:194–204. Korean.

12. Kim JM, Park JS. Comparison of unmet need and quality of life between permanent ostomates and temporary ostomates. J Korea Acad Ind Coop Soc 2018;19:374–83. Korean.

13. Oh EH, Hong SJ, Mo MH, Woo MY, Kim SJ, Chung BY. Distress of the patients with ostomy. J Korean Oncol Nurs 2011;11:9–19. Korean.


16. Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc 2019;51:2375–90.



17. Burgess-Stocks J. Eating with an ostomy: a comprehensive nutrition guide for those living with an ostomy. 2nd ed. United Ostomy Associations of America Inc; 2022.

18. Korean Oncology Nursing Society; Korean Cancer Study Group. [Guidelines for controlling side effects of anticancer therapies] [Internet]. Korean Oncology Nursing Society, Korean Cancer Study Group; 2021 [cited 2021 Dec 1]. Korean. Available from: https://www.kcsg.org/web/board/noticeView.do?boardIdx=1547
19. Ayaz-Alkaya S. Overview of psychosocial problems in individuals with stoma: a review of literature. Int Wound J 2019;16:243–9.




20. Korea Disabled People’s Development Institute (KODDI). [Welfare needs and policy direction of the ostomy and urostomy disabled people (2018)] [Internet]. KODDI; 2018 [cited 2021 Dec 1]. Korean. Available from: https://www.koddi.or.kr/data/research01_view.jsp?brdNum=7405328
- TOOLS